Abstract
Background
The treatments based on motor control and motor learning principles have gained popularity in the last 20 years, as well as non-invasive brain stimulations that enhance neuroplastic changes after stroke. However, the effect of intermittent theta burst stimulation (iTBS) in addition to evidence-based, intensive neurorehabilitation approaches such as modified constraint-induced movement therapy (mCIMT) is yet to be investigated.
Aim
We aim to establish a protocol for a randomized controlled study investigating the efficiency of mCIMT primed with iTBS after stroke.
Methods
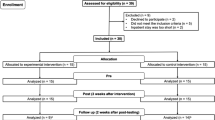
In this randomized controlled, single-blind study, patients with stroke (N = 17) will be divided into 3 groups: (a) mCIMT + real iTBS, (b) mCIMT + sham iTBS, and (c) mCIMT alone. 600-pulse iTBS will be delivered to the primary motor cortex on the ipsilesional hemisphere, and then, patients will receive mCIMT for 1 h/session, 3 sessions/week for 5 weeks. Upper extremity recovery will be assessed with Fugl-Meyer Test-Upper Extremity and Wolf Motor Function Test. Electrophysiological assessments, such as Motor-Evoked Potentials, Resting Motor Threshold, Short-Intracortical Inhibition, and Intracortical Facilitation, will also be included.
Conclusions
In this study, a protocol of an ongoing intervention study investigating the effectiveness of iTBS on ipsilesional M1 prior to the mCIMT in patients with stroke is proposed. This will be the first study to research priming mCIMT with iTBS and it may have the potential to reveal the true effect of the iTBS when it is added to the high-quality neurorehabilitation approaches.
Trial registration
Trial registration number: NCT05308667

Similar content being viewed by others
Data availability
There are no linked data sets for this paper. The data are confidential, since the participant of this study were informed upon admission to the hospital that the data would remain confidential and would not be shared with third parties.
Code availability
Not applicable.
References
Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A et al (2013) An updated definition of stroke for the 21st Century. Stroke 44:2064–2089
World Stroke Organization (2022) Global stroke fact sheet. Available from: https://www.world-stroke.org/assets/downloads/WSO_Global_Stroke_Fact_Sheet.pdf. Accessed 01 Apr 2023
Hussain N, Alt Murphy M, Sunnerhagen KS (2018) Upper limb kinematics in stroke and healthy controls using target-to-target task in virtual reality. Front Neurol 9:300. https://doi.org/10.3389/fneur.2018.00300
Winstein CJ, Joel S, Ross A, Barbara B, Cherney LR, Cramer SC et al (2016) Guidelines for adult stroke rehabilitation and recovery. Stroke 47:e98-169
Hebert D, Lindsay MP, McIntyre A, Kirton A, Rumney PG, Bagg S et al (2016) Canadian stroke best practice recommendations: Stroke rehabilitation practice guidelines, update 2015. Int J Stroke 11:459–484
Taub E, Uswatte G, Pidikiti R (1999) Constraint-Induced Movement Therapy: a new family of techniques with broad application to physical rehabilitation–a clinical review. J Rehabil Res Dev 36:237–251
Hüseyinsinoğlu Ersöz B, Razak ÖA (2015) Kısıtlayıcı-Zorunlu Hareket Tedavisi: Nöral Temeli, Uygulama Prensipleri ve Uygulama Alanları. Turkiye Klin J Physiother Rehabil-Special Top 1:22–29
de Azevedo JA, Barbosa FDS, Seixas VM, da Silva Scipioni KRD, Sampaio PYS, da Cruz DMC, et al. (2022) Effects of constraint-induced movement therapy on activity and participation after a stroke: systematic review and meta-analysis. Front Hum Neurosci 16:987061. https://doi.org/10.3389/fnhum.2022.987061
Kwakkel G, Veerbeek JM, van Wegen EEH, Wolf SL (2015) Constraint-induced movement therapy after stroke. Lancet Neurol 14:224–234
Page SJ, Levine P, Sisto S, Bond Q, Johnston MV (2002) Stroke patients’ and therapists’ opinions of constraint-induced movement therapy. Clin Rehabil 16:55–60
Page S, Boe S, Levine P (2013) What are the “ingredients” of modified constraint-induced therapy? An evidence-based review, recipe, and recommendations. Restor Neurol Neurosci 31:299–309
Yang YW, Pan WX, Xie Q (2020) Combined effect of repetitive transcranial magnetic stimulation and physical exercise on cortical plasticity. Neural Regen Res 15:1986–1994
Zhang L, Xing G, Fan Y, Guo Z, Chen H, Mu Q (2017) Short- and long-term effects of repetitive transcranial magnetic stimulation on upper limb motor function after stroke: a systematic review and meta-analysis. Clin Rehabil 31:1137–1153
Ackerley SJ, Byblow WD, Barber PA, MacDonald H, McIntyre-Robinson A, Stinear CM (2016) Primed physical therapy enhances recovery of upper limb function in chronic stroke patients. Neurorehabil Neural Repair 30:319–348
Volz LJ, Rehme AK, Michely J, Nettekoven C, Eickhoff SB, Fink GR et al (2016) Shaping early reorganization of neural networks promotes motor function after stroke. Cereb Cortex 26:2882–2894
Chen YJ, Huang YZ, Chen CY, Chen CL, Chen HC, Wu CY et al (2019) Intermittent theta burst stimulation enhances upper limb motor function in patients with chronic stroke: a pilot randomized controlled trial. BMC Neurol 19:69
Suppa A, Huang YZ, Funke K, Ridding MC, Cheeran B, Di Lazzaro V et al (2016) Ten years of theta burst stimulation in humans: established knowledge. Unkn Prospect Brain Stimul 9:323–335
Uswatte G, Taub E (2013) Constraint-induced movement therapy: a method for harnessing neuroplasticity to treat motor disorders. Prog Brain Res 207:379–401
Rossi S, Hallett M, Rossini PM, Pascual-Leone A (2009) Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol 120:2008–2039
Santisteban L, Térémetz M, Bleton J-P, Baron J-C, Maier MA, Lindberg PG (2016) Upper limb outcome measures used in stroke rehabilitation studies: a systematic literature review. PLoS ONE 11:e0154792
Gladstone DJ, Danells CJ, Black SE (2002) The Fugl-Meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair 16:232–240
Fugl-Meyer AR, Jääskö L, Leyman I, Olsson SSS (1975) The post-stroke hemiplegic patient. A method for evaluation of physical performance. Scand J Rehabil Med 7:13–31
Ng S, Tse M, Tam E, Lai C (2017) Reliability and convergent validity of the five-step test in people with chronic stroke. J Rehabil Med 50:16–21
Platz T, Pinkowski C, van Wijck F, Kim I-H, di Bella P, Johnson G (2005) Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block Test: a multicentre study. Clin Rehabil 19:404–411. https://doi.org/10.1191/0269215505cr832oa
Hsieh Y, Wu C, Lin K, Chang Y, Chen C, Liu J (2009) Responsiveness and validity of three outcome measures of motor function after stroke rehabilitation. Stroke 40:1386–1391. https://doi.org/10.1161/STROKEAHA.108.530584
Morris DM, Uswatte G, Crago JE, Cook EW, Taub E (2001) The reliability of the Wolf Motor Function Test for assessing upper extremity function after stroke. Arch Phys Med Rehabil 82:750–755
Uswatte G, Taub E, Morris D, Light K, Thompson PA (2006) the motor activity log-28—assessing daily use of the hemiparetic arm after stroke. Neurology 67:1189–1194
Ersöz Hüseyinsinoğlu B, Razak Özdinçler A, Erkan Oğul Ö, Krespi Y (2011) Reliability and validity of Turkish version of motor activity log-28. Turkish J Neurol 17:83–89
Sakai K, Ugawa Y, Terao Y, Hanajima R, Furubayashi T, Kanazawa I (1997) Preferential activation of different I waves by transcranial magnetic stimulation with a figure-of-eight-shaped coil. Exp Brain Res 113:24–32
Özdemir Z, Acar E, Soysal A (2021) The effects of 30 Hz, 50 Hz AND 100 Hz continuous theta burst stimulation via transcranial magnetic stimulation on the electrophysiological parameters in healthy individuals. Ideggyogy Sz 74:41–49
Veldema J, Nowak DA, Gharabaghi A (2021) Resting motor threshold in the course of hand motor recovery after stroke: a systematic review. J Neuroeng Rehabil 18:158
Legatt AD (2014) Motor evoked potentials. In: Aminoff MJ (ed) Daroff RBBT-E of the NS. Academic Press, Oxford, pp 111–114
Fisicaro F, Lanza G, Cantone M, Ferri R, Pennisi G, Nicoletti A et al (2020) Clinical and electrophysiological hints to TMS in de novo patients with Parkinson’s disease and progressive supranuclear palsy. J Pers Med 10:274
Rossini PM, Burke D, Chen R, Cohen LG, Daskalakis Z, Di Iorio R et al (2015) Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: basic principles and procedures for routine clinical and research application. An updated report from an IFCN Committee. Clin Neurophysiol 126:1071–1107
Lefaucheur JP, Drouot X, Ménard-Lefaucheur I, Keravel Y, Nguyen JP (2006) Motor cortex rTMS restores defective intracortical inhibition in chronic neuropathic pain. Neurology 67:1568–1574
Samusyte G, Bostock H, Rothwell J, Koltzenburg M (2018) Short-interval intracortical inhibition: comparison between conventional and threshold-tracking techniques. Brain Stimul 11:806–817
Kujirai T, Caramia MD, Rothwell JC, Day BL, Thompson PD, Ferbert A et al (1993) Corticocortical inhibition in human motor cortex. J Physiol 471:501–419. https://doi.org/10.1113/jphysiol.1993.sp019912
Huang Y-Z, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC (2005) Theta burst stimulation of the human motor cortex. Neuron 45:201–206
Kolbaşı EN, Hüseyinsinoğlu BE, Özdemir Z, Bayraktaroğlu Z, Soysal A (2022) Enhancement of motor skill acquisition by intermittent theta burst stimulation: a pilot study. Acta Neurol Belg 123:971–977
Hiragami S, Inoue Y, Harada K (2019) Minimal clinically important difference for the Fugl-Meyer assessment of the upper extremity in convalescent stroke patients with moderate to severe hemiparesis. J Phys Ther Sci 31:917–921
Huang W, Chen J, Zheng Y, Zhang J, Li X, Su L et al (2022) The effectiveness of intermittent theta burst stimulation for stroke patients with upper limb impairments: a systematic review and meta-analysis. Front Neurol 13:896651
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
de Morton NA (2009) The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 55:129–133
Teasell R, Salbach NM, Foley N, Mountain A, Cameron JI, de Jong A et al (2020) Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. Part One: Rehabilitation and recovery following stroke. Int J Stroke 15:763–788
Gao B, Wang Y, Zhang D, Wang Z, Wang Z (2022) Intermittent theta-burst stimulation with physical exercise improves poststroke motor function: a systemic review and meta-analysis. Front. Neurol 13:964627. https://doi.org/10.3389/fneur.2022.964627
Fregni F, Boggio P, Valle A, Rocha R, Duarte J, Ferreira M et al (2006) A sham-controlled trial of a 5-day course of repetitive transcranial magnetic stimulation of the unaffected hemisphere in stroke patients. Stroke 37:2115–2122
Plow EB, Cunningham DA, Beall E, Jones S, Wyant A, Bonnett C et al (2013) Effectiveness and neural mechanisms associated with tDCS delivered to premotor cortex in stroke rehabilitation: study protocol for a randomized controlled trial. Trials 14:331
Hao Z, Wang D, Zeng Y, Liu M (2013) Repetitive transcranial magnetic stimulation for improving function after stroke. Cochrane Database Syst Rev 2013(5):CD008862. https://doi.org/10.1002/14651858.CD008862.pub2
Funding
This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: ENK, BEH, ZÖ, ZB, and AS; methodology: ENK, BEH, ZÖ, ZB, and AS; writing—original draft preparation: ENK, BEH, ZÖ, and ZB; writing—review and editing: BH, ZB, ZÖ, and AS; supervision: BEH, ZB, and AS.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
The study was approved by Marmara University Faculty of Medicine Clinical Trials Ethics Committee (date 01.06.2022—no.09.2022.614) and administered according to the Ethical Principles for Medical Research Involving Human Subjects by the Helsinki Declaration.
Consent to participate
Both written and verbal consent will be obtained from the participants before the study.
Consent for publication
It will be obtained from the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kolbaşı, E.N., Huseyinsinoglu, B.E., Ozdemir, Z. et al. Priming constraint-induced movement therapy with intermittent theta burst stimulation to enhance upper extremity recovery in patients with stroke: protocol for a randomized controlled study. Acta Neurol Belg (2024). https://doi.org/10.1007/s13760-024-02472-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13760-024-02472-6