Abstract
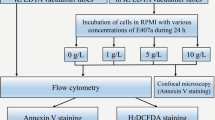
Aim In the current study, hemocompatibility of three major commercially available types of carrageenans (ι, κ and λ) was investigated focusing on eryptosis. Materials and methods: Carrageenans of ι-, κ- and λ-types were incubated with washed erythrocytes (hematocrit 0.4%) at 0–1–5–10 g/L for either 24 h or 48 h. Incubation was followed by flow cytometry-based quantitative analysis of eryptosis parameters, including cell volume, cell membrane scrambling and reactive oxygen species (ROS) production, lipid peroxidation markers and confocal microscopy-based evaluation of intracellular Ca2+ levels, assessment of lipid order in cell membranes and the glutathione antioxidant system. Confocal microscopy was used to assess carrageenan cellular internalization using rhodamine B isothiocyanate-conjugated carrageenans. Results: All three types of carrageenans were found to trigger eryptosis. Pro-eryptotic properties were type-dependent and λ-carrageenan had the strongest impact inducing phosphatidylserine membrane asymmetry, changes in cell volume, Ca2+ signaling and oxidative stress characterized by ROS overproduction, activation of lipid peroxidation and severe glutathione system depletion. Eryptosis induction by carrageenans does not require their uptake by erythrocytes. Changes in physicochemical properties of cell membrane were also type-dependent. No carrageenan-induced generation of superoxide and hydroxyl radicals was observed in cell-free milieu. Conclusions: Our findings suggest that ι-, κ- and λ-types trigger eryptosis in a type-dependent manner and indicate that carrageenans can be further investigated as potential eryptosis-regulating therapeutic agents.












Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author Anton Tkachenko upon reasonable request.
References
Yermak, I. M., Davydova, V. N., & Volod’ko, A. V. (2022). Mucoadhesive Marine Polysaccharides. Marine Drugs, 20, 522.
Ghanbarzadeh, M., Golmoradizadeh, A., & Homaei, A. (2018). Carrageenans and carrageenases: versatile polysaccharides and promising marine enzymes. Phytochemistry Reviews, 17, 535–571.
Liu, F., Duan, G., & Yang, H. (2023). Recent advances in exploiting carrageenans as a versatile functional material for promising biomedical applications. International Journal of Biological Macromolecules, 235, 123787.
Borsani, B., De Santis, R., Perico, V., et al. (2021). The Role of Carrageenan in Inflammatory Bowel Diseases and Allergic Reactions: Where Do We Stand? Nutrients, 13, 3402.
Ścieszka, S., & Klewicka, E. (2019). Algae in food: a general review. Critical Reviews in Food Science and Nutrition, 59, 3538–3547.
Liao, Y. C., Chang, C. C., Nagarajan, D., Chen, C. Y., & Chang, J. S. (2021). Algae-derived hydrocolloids in foods: applications and health-related issues. Bioengineered, 12, 3787–3801.
Ciancia, M., Matulewicz, M. C., & Tuvikene, R. (2020). Structural Diversity in Galactans From Red Seaweeds and Its Influence on Rheological Properties. Frontiers in Plant Science, 11, 559986.
Álvarez-Viñas, M., Souto, S., Flórez-Fernández, N., Torres, M. D., Bandín, I., & Domínguez, H. (2021). Antiviral Activity of Carrageenans and Processing Implications. Marine Drugs 19, 437.
Frediansyah, A. (2021). The antiviral activity of iota-, kappa-, and lambda-carrageenan against COVID-19: A critical review. Clinical Epidemiology and Global Health, 12, 100826.
Krylova, N. V., Kravchenko, A. O., & Iunikhina, O. V., et al. (2022). Influence of the Structural Features of Carrageenans from Red Algae of the Far Eastern Seas on Their Antiviral Properties. Marine Drugs, 20, 60.
Liu, Z., Gao, T., Yang, Y., et al. (2019). Anti-Cancer Activity of Porphyran and Carrageenan from Red Seaweeds. Molecules 24, 4286.
Khotimchenko, M., Tiasto, V., & Kalitnik, A., et al. (2020). Antitumor potential of carrageenans from marine red algae. Carbohydrate Polymers, 246, 116568.
Pacheco-Quito, E. M., Ruiz-Caro, R., Veiga, M. D. (2020). Carrageenan: Drug Delivery Systems and Other Biomedical Applications. Marine Drugs, 18, 583.
Zank, P. D., Cerveira, M. M., & Santos, V. B. D., et al. (2023). Carrageenan from Gigartina skottsbergii: A Novel Molecular Probe to Detect SARS-CoV-2. Biosensors, 13, 378.
McKim, J. M., Willoughby, Sr, J. A., Blakemore, W. R., & Weiner, M. L. (2019). Clarifying the confusion between poligeenan, degraded carrageenan, and carrageenan: A review of the chemistry, nomenclature, and in vivo toxicology by the oral route. Critical Reviews in Food Science and Nutrition, 59, 3054–3073.
Tobacman, J. K. (2001). Review of harmful gastrointestinal effects of carrageenan in animal experiments. Environ Health Perspect, 109, 983–994.
Cohen, S. M., & Ito, N. (2002). A critical review of the toxicological effects of carrageenan and processed eucheuma seaweed on the gastrointestinal tract. Critical Reviews in Toxicology, 32, 413–444.
Martino, J. V., Van Limbergen, J., & Cahill, L. E. (2017). The Role of Carrageenan and Carboxymethylcellulose in the Development of Intestinal Inflammation. Frontiers in Pediatrics, 5, 96.
David, S., Shani Levi, C., & Fahoum, L., et al. (2018). Revisiting the carrageenan controversy: do we really understand the digestive fate and safety of carrageenan in our foods? Food and Function Journal, 9, 1344–1352.
Liu, F., Hou, P., Zhang, H., Tang, Q., Xue, C., & Li, R. W. (2021). Food-grade carrageenans and their implications in health and disease. Comprehensive Reviews in Food Science and Food Safety, 20, 3918–3936.
Pogozhykh, D., Posokhov, Y., Myasoedov, V., et al. (2021). Experimental Evaluation of Food-Grade Semi-Refined Carrageenan Toxicity. International Journal of Molecular Sciences, 22, 11178.
Additives EPanel oF, Food NSat, Younes, M., et al. (2018). Re-evaluation of carrageenan (E 407) and processed Eucheuma seaweed (E 407a) as food additives. EFSA Journal, 16, e05238.
Weiner, M. L. (2014). Food additive carrageenan: Part II: A critical review of carrageenan in vivo safety studies. Critical Reviews in Toxicology, 44, 244–269.
McKim, Jr, J. M., Baas, H., Rice, G. P., Willoughby, Sr, J. A., Weiner, M. L., & Blakemore, W. (2016). Effects of carrageenan on cell permeability, cytotoxicity, and cytokine gene expression in human intestinal and hepatic cell lines. Food and Chemical Toxicology, 96, 1–10.
Guo, J., Shang, X., Chen, P., & Huang, X. (2023). How does carrageenan cause colitis? A review. Carbohydrate Polymers, 302, 120374.
Marques, D. M. C., Silva, J. C., Serro, A. P., Cabral, J. M. S., Sanjuan-Alberte, P., & Ferreira, F. C. (2022) 3D Bioprinting of Novel κ-Carrageenan Bioinks: An Algae-Derived Polysaccharide. Bioengineering (Basel) 9, 109.
Loukelis, K., Machla, F., Bakopoulou, A., & Chatzinikolaidou, M. (2023). Kappa-Carrageenan/Chitosan/Gelatin Scaffolds Provide a Biomimetic Microenvironment for Dentin-Pulp Regeneration. International Journal of Molecular Sciences, 24, 6465.
Yilmaz-Aykut, D., Torkay, G., Kasgoz, A., Shin, S. R., Bal-Ozturk, A., & Deligoz, H. (2023). Injectable and self-healing dual crosslinked gelatin/kappa-carrageenan methacryloyl hybrid hydrogels via host-guest supramolecular interaction for wound healing. Journal of Biomedical Materials Research, 111, 1921–1937.
Chen, Z., Yang, B., Yan, Z., Song, E., & Song, Y. (2022). Eryptosis is an indicator of hematotoxicity in the risk assessment of environmental amorphous silica nanoparticles exposure: The role of macromolecule corona. Toxicology Letters, 367, 40–47.
Tkachenko, A., Onishchenko, A., Myasoedov, V., Yefimova, S., & Havranek, O. (2023). Assessing regulated cell death modalities as an efficient tool for in vitro nanotoxicity screening: a review. Nanotoxicology, 17, 218–248.
Boulet, C., Doerig, C. D., & Carvalho, T. G. (2018). Manipulating Eryptosis of Human Red Blood Cells: A Novel Antimalarial Strategy? Frontiers in Cellular and Infection Microbiology 8, 419.
Boulet, C., Gaynor, T. L., & Carvalho, T. G. (2021). Eryptosis and Malaria: New Experimental Guidelines and Re-Evaluation of the Antimalarial Potential of Eryptosis Inducers. Frontiers in Cellular and Infection Microbiology, 11, 630812.
Scovino, A. M., Totino, P. R. R., & Morrot, A. (2022). Eryptosis as a New Insight in Malaria Pathogenesis. Frontiers in Immunology, 13, 855795.
Tkachenko, A., Kot, Y., Prokopyuk, V., et al. (2021). Food additive E407a stimulates eryptosis in a dose-dependent manner. Wien Med Wochenschr.
Peter, T., Bissinger, R., & Lang, F. (2016). Erythrocyte Shrinkage and Cell Membrane Scrambling after Exposure to the Ionophore Nonactin. Basic & Clinical Pharmacology and Toxicology, 118, 107–112.
Prokopiuk, V., Yefimova, S., & Onishchenko, A., et al. (2023). Assessing the Cytotoxicity of TiO(2-x) Nanoparticles with a Different Ti(3+)(Ti(2+))/Ti(4+) Ratio. Biological Trace Element Research, 201, 3117–3130.
Alfhili, M. A., Nkany, M. B., Weidner, D. A., & Lee, M. H. (2019). Stimulation of eryptosis by broad-spectrum insect repellent N,N-Diethyl-3-methylbenzamide (DEET). Toxicology and Applied Pharmacology, 370, 36–43.
Alfhili, M. A., & Aljuraiban, G. S. (2021). Lauric Acid, a Dietary Saturated Medium-Chain Fatty Acid, Elicits Calcium-Dependent Eryptosis. Cells, 10, 3388.
Zangeneh, A. R., Takhshid, M. A., Ranjbaran, R., Maleknia, M., & Meshkibaf, M. H. (2021). Diverse Effect of Vitamin C and N-Acetylcysteine on Aluminum-Induced Eryptosis. Biochemistry Research International, 2021, 6670656.
Tkachenko, A., & Onishchenko, A. (2023). Casein kinase 1α mediates eryptosis: a review. Apoptosis, 28, 1–19.
Tietze, F. (1969). Enzymic method for quantitative determination of nanogram amounts of total and oxidized glutathione: Applications to mammalian blood and other tissues. Analytical Biochemistry, 27, 502–522.
Tupper, J., Tozer, G. M., & Dachs, G. U. (2004). Use of horseradish peroxidase for gene-directed enzyme prodrug therapy with paracetamol. British Journal of Cancer, 90, 1858–1862.
Carlberg, I., & Mannervik, B. (1975). Purification and characterization of the flavoenzyme glutathione reductase from rat liver. Journal of Biological Chemistry, 250, 5475–5480.
Paglia, D. E., & Valentine, W. N. (1967). Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. Journal of Laboratory and Clinical Medicine, 70, 158–169.
Warholm, M., Guthenberg, C., von Bahr, C., & Mannervik, B. (1985). Glutathione transferases from human liver. Methods in Enzymology, 113, 499–504.
Posokhov, Y. O., Kyrychenko, A., & Korniyenko, Y. (2018). Derivatives of 2,5-Diaryl-1,3-Oxazole and 2,5-Diaryl-1,3,4-Oxadiazole as Environment-Sensitive Fluorescent Probes for Studies of Biological Membranes. In C. D. Geddes (ed), Reviews in Fluorescence 2017 (pp. 199–230). Cham: Springer International Publishing.
Posokhov, Y., & Kyrychenko, A. (2018). Location of fluorescent probes (2’-hydroxy derivatives of 2,5-diaryl-1,3-oxazole) in lipid membrane studied by fluorescence spectroscopy and molecular dynamics simulation. Biophysical Chemistry, 235, 9–18.
Kurad, D., Jeschke, G., & Marsh, D. (2003). Lipid membrane polarity profiles by high-field EPR. Biophysical Journal, 85, 1025–1033.
Ho, C., Slater, S. J., & Stubbs, C. D. (1995). Hydration and order in lipid bilayers. Biochemistry, 34, 6188–6195.
Tkachenko, A., Onishchenko, A., Posokhov, Y., Roshal, A., Myasoedov, V., & Nakonechna, O. (2021). Changes in cell membranes of white blood cells treated with a common food additive E407a. Turkish Journal of Biochemistry, 46, 557–562.
Tkachenko, A. S., Kot, Y. G., & Kapustnik, V. A., et al. (2021). Semi-refined carrageenan promotes generation of reactive oxygen species in leukocytes of rats upon oral exposure but not in vitro. Wiener Medizinische Wochenschrift, 171, 68–78.
Ashawa, S. C., Kini, U. R., & Madhvanath, U. (1979). The aqueous coumarin system as a low range chemical dosimeter. The International Journal of Applied Radiation and Isotopes, 30, 7–10.
Maksimchuk, P. O., Yefimova, S. L., & Hubenko, K. O., et al. (2020). Dark Reactive Oxygen Species Generation in ReVO4:Eu3+ (Re = Gd, Y) Nanoparticles in Aqueous Solutions. The Journal of Physical Chemistry C, 124, 3843–3850.
Tao, Z., Wang, G., Goodisman, J., & Asefa, T. (2009). Accelerated Oxidation of Epinephrine by Silica Nanoparticles. Langmuir, 25, 10183–10188.
Pretorius, E., du Plooy, J. N., & Bester, J. (2016). A Comprehensive Review on Eryptosis. Cellular Physiology and Biochemistry, 39, 1977–2000.
Föller, M., & Lang, F. (2020). Ion Transport in Eryptosis, the Suicidal Death of Erythrocytes. Frontiers in Cell and Developmental Biology, 8, 597.
Alghareeb, S. A., Alfhili M. A., & Fatima S. (2023). Molecular Mechanisms and Pathophysiological Significance of Eryptosis. International Journal of Molecular Sciences, 24, 5079.
Pan, X., Giustarini, D., Lang, F., et al. (2023). Desipramine induces eryptosis in human erythrocytes, an effect blunted by nitric oxide donor sodium nitroprusside and N-acetyl-L-cysteine but enhanced by Calcium depletion. Cell Cycle, 22, 1827–1853.
Waggiallah, H., & Alzohairy, M. (2011). The effect of oxidative stress on human red cells glutathione peroxidase, glutathione reductase level, and prevalence of anemia among diabetics. North American Journal of Medicine and Science, 3, 344–347.
van ‘t Erve, T. J., Wagner, B. A., Ryckman, K. K., Raife, T. J., & Buettner, G. R. (2013). The concentration of glutathione in human erythrocytes is a heritable trait. Free Radical Biology and Medicine, 65, 742–749.
Maurya, P. K., Kumar, P., & Chandra, P. (2015). Biomarkers of oxidative stress in erythrocytes as a function of human age. World Journal of Methodology, 5, 216–222.
Bhattacharyya, S., Dudeja, P. K., & Tobacman, J. K. (2008). Carrageenan-induced NFκB activation depends on distinct pathways mediated by reactive oxygen species and Hsp27 or by Bcl10. Biochimica et Biophysica Acta (BBA) - General Subjects, 1780, 973–982.
Barth, C. R., Funchal, G. A., Luft, C., de Oliveira, J. R., Porto, B. N., & Donadio, M. V. (2016). Carrageenan-induced inflammation promotes ROS generation and neutrophil extracellular trap formation in a mouse model of peritonitis. European Journal of Immunology, 46, 964–970.
Lopes, A. H., Silva, R. L., & Fonseca, M. D., et al. (2020). Molecular basis of carrageenan-induced cytokines production in macrophages. Cell Communication and Signaling, 18, 141.
McKim, J. M., Baas, H., Rice, G. P., Willoughby, J. A., Weiner, M. L., & Blakemore, W. (2016). Effects of carrageenan on cell permeability, cytotoxicity, and cytokine gene expression in human intestinal and hepatic cell lines. Food and Chemical Toxicology, 96, 1–10.
Sokolova, E. V., Karetin, Y., & Davydova, V. N., et al. (2016). Carrageenans effect on neutrophils alone and in combination with LPS in vitro. Journal of Biomedical Materials Research Part A, 104, 1603–1609.
Chen, H. M., Yan, X. J., Wang, F., Xu, W. F., & Zhang, L. (2010). Assessment of the oxidative cellular toxicity of a κ-carrageenan oxidative degradation product towards Caco-2 cells. Food Research International, 43, 2390–2401.
Reiter, R. J., Tan, D. X., & Galano, A. (2014). Melatonin reduces lipid peroxidation and membrane viscosity. Frontiers in Physiology, 5, 377.
Catalá, Á. (2014). Lipid peroxidation modifies the assembly of biological membranes “The Lipid Whisker Model”. Frontiers in Physiology, 5, 520.
Jensen, L. B., Burgess, N. K., & Gonda, D. D., et al. (2005). Mechanisms governing the level of susceptibility of erythrocyte membranes to secretory phospholipase A2. Biophysical Journal, 88, 2692–2705.
Lee, J. C., Simonyi, A., Sun, A. Y., & Sun, G. Y. (2011). Phospholipases A2 and neural membrane dynamics: implications for Alzheimer’s disease. Journal of Neurochemistry, 116, 813–819.
Pyrshev, K. A., Yesylevskyy, S. O., Mély, Y., Demchenko, A. P., & Klymchenko, A. S. (2017). Caspase-3 activation decreases lipid order in the outer plasma membrane leaflet during apoptosis: A fluorescent probe study. Biochimica et Biophysica Acta (BBA) - Biomembranes, 1859, 2123–2132.
da SilveiraCavalcante, L., Acker, J. P., & Holovati, J. L. (2015). Differences in Rat and Human Erythrocytes Following Blood Component Manufacturing: The Effect of Additive Solutions. Transfusion Medicine and Hemotherapy, 42, 150–157.
Incebacak Eltemur, R. D., Nguyen, H. P., & Weber, J. J. (2022). Calpain-mediated proteolysis as driver and modulator of polyglutamine toxicity. Frontiers in Molecular Neuroscience, 15, 1020104.
Léger, C., Pitard, I., & Sadi, M., et al. (2022). Dynamics and structural changes of calmodulin upon interaction with the antagonist calmidazolium. BMC Biology, 20, 176.
Hoeflich, K. P., & Ikura, M. (2002). Calmodulin in action: diversity in target recognition and activation mechanisms. Cell, 108, 739–742.
Bogdanova, A., Makhro, A., Wang, J., Lipp, P., & Kaestner, L. (2013). Calcium in red blood cells-a perilous balance. International Journal of Molecular Sciences, 14, 9848–9872.
Lang, F., Lang, K. S., Lang, P. A., Huber, S. M., & Wieder, T. (2006). Mechanisms and significance of eryptosis. Antioxidants and Redox Signaling, 8, 1183–1192.
Humayun, S., Premarathna, A. D., & Rjabovs, V., et al. (2023). Biochemical Characteristics and Potential Biomedical Applications of Hydrolyzed Carrageenans. Marine Drugs 21, 269.
Setz, C., Große, M., & Fröba, M., et al. (2023). Iota-Carrageenan Inhibits Replication of the SARS-CoV-2 Variants of Concern Omicron BA.1, BA.2 and BA.5. Nutraceuticals, 3, 315–328.
Bhattacharyya, S., Gill, R., & Chen, M. L., et al. (2008). Toll-like receptor 4 mediates induction of the Bcl10-NFkappaB-interleukin-8 inflammatory pathway by carrageenan in human intestinal epithelial cells. Journal of Biological Chemistry, 283, 10550–10558.
Lam, L. K. M., Murphy, S., & Kokkinaki, D., et al. (2021). DNA binding to TLR9 expressed by red blood cells promotes innate immune activation and anemia. Science Translational Medicine, 13, eabj1008.
Ridone, P., Vassalli, M., & Martinac, B. (2019). Piezo1 mechanosensitive channels: what are they and why are they important. Biophysical Reviews, 11, 795–805.
Vaisey, G., Banerjee, P., North, A. J., Haselwandter, C. A., & MacKinnon, R. (2022). Piezo1 as a force-through-membrane sensor in red blood cells. Elife 11, e82621.
Funding
The study was supported by the Ministry of Health of Ukraine as a fragment of the research project entitled “Research on the Safety and Effectiveness of Food Additives Carrageenans (E407/E407a) and Their Oligosaccharide Fragments as Therapeutic Agents Capable of Modulating Programmed Cell Death, Namely Eryptosis, Necroptosis, Ferroptosis and Autophagy-Related Cell Death” (state registration number 0123U100179). The study of cell membranes using the fluorescent probe and flow cytometry was supported by the National Research Foundation of Ukraine under project No. 2021.01/0414.
Author information
Authors and Affiliations
Contributions
Conceptualization – A.T., methodology – A.T., A.O. V.P., Ye.P., L.T., T.G., O.N., Yu. K., K.K. P.M., data analysis – A.T., A.O., V.P., L.T., Ye.P., P.M., Yu. K., K.K. Investigation – A.O. V.P., T.G., P.M., Ye.P., Yu. K., K.K., L.T. resources – A.T., V.P., Writing - Original Draft – A.T., Ye.P., Yu.K., Writing - Review & Editing – A.T, A.O., Ye.P, O.N., visualization – A.O., Ye.P., Yu. K., A.T., funding – A.T., V.P., project administration – A.T.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethics Approval
All experiments with laboratory animals involved were carried out following the legislative requirements and ethical standards in agreement with the EU Directive 2010/63/EU on the protection of animals used for scientific purposes, which is based on the Council of Europe Convention for the Protection of Vertebrate Animals used for Experimental and other Scientific Purposes (ETS123). The experimental design was approved by the Commission on Ethics and Bioethics at Kharkiv National Medical University, Kharkiv, Ukraine (minutes No 5 dated September 17, 2019).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Prokopiuk, V., Onishchenko, A., Tryfonyuk, L. et al. Marine Polysaccharides Carrageenans Enhance Eryptosis and Alter Lipid Order of Cell Membranes in Erythrocytes. Cell Biochem Biophys (2024). https://doi.org/10.1007/s12013-024-01225-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12013-024-01225-9