Abstract
Background
Transcatheter edge-to-edge mitral valve repair (M-TEER) is often performed in general anesthesia, and postprocedural monitoring is usually warranted on an intensive or intermediate care unit (ICU/IMC). We evaluated the implications of a dedicated valve unit (VU) instead of an ICU/IMC for monitoring after M-TEER.
Methods and results
In total, 624 patients were retrospectively analyzed. A total of 312 patients were primarily transferred to either ICU or IMC following M-TEER, and 312 patients were scheduled for the VU in the absence of indications for ICU/IMC treatment. Hospital stay was significantly shorter in VU patients (median 6.0 days (interquartile range (IQR) 5.0 – 8.0) vs. 7.0 days (IQR 6.0 – 10.0), p < 0.001) and their risk for infections (2.9 vs. 7.7%, p = 0.008) and delirium (0.6 vs. 2.6%, p = 0.056) was substantially lower compared to ICU/IMC patients. In-hospital mortality was similar in both groups (0.6% vs. 1.3%, p = 0.41).
Fifty patients (16.0%) in the VU group had to cross over to unplanned ICU/IMC admission. The most frequent indication was prolonged need for catecholamines (52.0%). Patients with ICU/IMC crossover had more advanced stages of heart failure (LV-EF < 30% in 36.0 vs. 16.0%, p = 0.001; severe concomitant tricuspid regurgitation in 48.0 vs. 27.8%, p = 0.005) and an LV-EF < 30% was independently associated with unplanned ICU/IMC admission.
Conclusions
Following M-TEER postprocedural monitoring on a VU instead of an ICU/IMC is safe, reduces complications, and spares ICU capacities. Patients with advanced heart failure have a higher risk for unplanned ICU/IMC treatment after M-TEER.
Graphical abstract
Valve unit instead of intensive or intermediate care unit admission following transcatheter edge-to-edge mitral valve repair is safe and reduces postprocedural complications.

Similar content being viewed by others
Introduction
Percutaneous transcatheter edge-to-edge mitral valve repair (M-TEER) is well established for interventional treatment of moderate to severe mitral regurgitation (MR) in symptomatic patients with high surgical risk and favorable anatomy [1]. Due to the need of periinterventional guidance by transesophageal echocardiography and for reasons of patient safety, the procedure is mostly performed in general anesthesia (GA) [2]. However, avoidance of GA and even of conscious sedation can be a feasible option for high-risk patients [3, 4]. The optimal postprocedural care for patients after M-TEER has not yet been defined. Intensive care unit (ICU) or intermediate care unit (IMC) admission can be seen as a standard due to putatively better response to complications [2, 5]. Such complications may include bleeding or infection [6, 7]. However, the COVID-19 pandemic has demonstrated the importance of careful utilization of intensive care capacities [8]. In response to the shortage of ICU and IMC resources during the pandemic, our center has established a dedicated valve unit (VU), spatially integrated into the general cardiology ward, for patient monitoring before and after valve procedures such as transfemoral aortic valve replacement (TAVR) or M-TEER in the absence of indications for ICU/IMC treatment. This study analyzes the feasibility and safety of a VU and its implications on patient outcomes and length of hospital stay.
Methods
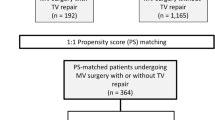
We retrospectively examined 624 consecutive patients who underwent M-TEER in GA at our center from March 2017 to March 2023. Until April 2020, all 312 included patients were admitted to the ICU or IMC following the procedure. From April 2020, the following 312 patients were monitored on the valve unit (VU) immediately after the valve procedure in the absence of indications for ICU or IMC treatment. Patients, which were initially planned for VU admittance but required postprocedural ICU/IMC therapy (crossover group) were transferred to the VU after appropriate stabilization. The postprocedural course was registered until discharge. An overview of the study design is shown in Fig. 1.
All patients included in the present study were symptomatic in terms of heart failure (New York Heart Association (NYHA) functional class ≥ II) despite guideline-directed medical therapy. Echocardiographic characteristics at baseline and after the procedure were available for all study patients. Severity of MR was classified in four degrees according to the latest EACVI/ESC recommendations for MR quantification [9]. Left ventricular (LV) ejection fraction (LV-EF) was measured using the biplane Simpson method. LV diameters were measured in the parasternal long-axis view. Postprocedural MR severity was assessed by 2D and 3D transesophageal echocardiography after final device placement and removal of the guide catheter. MR was semi-quantitatively assessed by visual estimation of MR jet area and by (biplane) determination of the vena contracta of the major MR jet. In addition to MR severity, mitral valve gradients and area by 3D technique were assessed before and after device deployment and after removal of the guide catheter.
Device success was defined as TEER with reduction of MR of at least one degree with no more than moderate residual MR and absence of major device or procedure-related serious adverse events [10].
Standard for anti-infective prophylaxis was a single-shot of cefazolin before the start of the procedure. In case of known penicillin allergy, a single dose of levofloxacin was administered. Procedural duration was counted from the first femoral incision until access site closure. Time of anesthesia was counted from the start of induction of narcosis until extubation or, in case of prolonged ventilation, until handover to the ICU/IMC.
Statistical analysis was performed using SPSS 28 software (IBM Corp., Armonk, USA). Categorical variables are expressed as counts and percentages and were compared by Chi-square test or McNemar test, as appropriate. Continuous parameters were analyzed for normal distribution using Kolmogorov–Smirnov test. Normally distributed variables are presented as the mean ± standard deviation and were compared with t-test. Variables without normal distribution are shown as the median and quartiles and were compared with the Kruskal–Wallis test.
To determine predictors of unplanned ICU admission, univariate logistic regression analysis was performed for all potential influential variables (p < 0.2). In multivariate regression analysis, a backward stepwise algorithm was applied to all potentially influential parameters. Correlation was tested using Pearson’s correlation coefficient, Spearman’s rho, or Eta2 as appropriate. Variables with significant correlation were excluded from multivariate analysis. Due to the large number of covariates, stricter cutoffs for significant correlation were chosen (p < 0.05 or Eta2 > 0.2). Correlation analysis is shown in the Supplemental material.
All tests were two-tailed and differences were considered statistically significant when p < 0.05.
The study was ethically approved by the ethics committee of the University of Ulm (Approval Number 435/16) and complied with the principles outlined in the Declaration of Helsinki (Br Med J 1964; ii: 177).
Results
The valve unit
The VU was spatially integrated into a general cardiology ward at our tertiary care medical center. Patients were admitted to the VU before and immediately after valve procedures such as M-TEER, transcatheter edge-to-edge tricuspid valve repair (T-TEER), or TAVR in the absence of indications for ICU or IMC treatment. Invasive or non-invasive ventilation as well as administration of catecholamines was not to be performed on the VU. However, patient monitoring was intensified and followed a dedicated protocol. Monitoring consisted of continuous telemetric three-lead ECG recording and assessment of peripheral oxygen saturation as well as periodical non-invasive blood pressure measurements, all connected to a central alarm system. Compared to a standard cardiology ward, surveillance was intensified: intervals between blood pressure measurements were set to 10 min for the first hour after postprocedural admittance to the VU. Subsequently, half-hourly measurements were taken for 4 h. Under stable conditions, blood pressure measurements and telemetric monitoring were terminated after 4 h. Checkups by nursing staff were carried out quarter-hourly in the first hour after M-TEER followed by visits at least every 2 h until the following day. A physician was available 24 h and all medical staff were trained for specific aspects of care following GA and valve interventions, specifically including access site bleeding and other vascular complications, pericardial effusion, renal failure, or neurologic events. Nursing staff recorded all measurements and clinical events on dedicated VU patient files. In case of an uneventful postprocedural course, patients were discharged directly from the VU.
Baseline characteristics and procedural details of the study subgroups
In total, 624 patients were analyzed consecutively. A total of 312 patients were transferred to the ICU/IMC following M-TEER, and 312 patients were scheduled for the VU. Apart from a lower prevalence of atrial fibrillation, there was no significant difference in demographics and comorbidities. Patients in the ICU/IMC era had larger left ventricles and more severe MR at baseline. Duration of the procedure and of anesthesia was significantly longer in these patients and device success was inferior compared to the VU era. Severe periinterventional complications were very rare and occurred equally in both groups. While in the ICU/IMC era the MitraClip platform (Abbott Cardiovascular) was used predominantly, procedures were performed in equal shares with both MitraClip and PASCAL (Edwards Lifesciences) platforms in the VU era. Median time spent on the ICU was 4.0 h in the ICU/IMC group while it was 0.0 h in the VU group. VU patients had a significantly shorter hospital stay.
Baseline characteristics and procedural details are shown in Table 1.
Postprocedural complication rates in the ICU and the VU era
In an “intention-to-treat” analysis, the incidence of infections was significantly lower in the VU era compared to the ICU/IMC group (2.9 vs. 7.7%, p = 0.008). The incidence of postprocedural delirium was also considerably lower (0.6 vs. 2.6%, p = 0.056). In-hospital mortality overall was very rare and was similar in both groups (0.6% in the VU group, 1.3% in the ICU group, p = 0.41) (Fig. 2). These effects were even more pronounced in an “as-treated” analysis combining planned ICU/IMC admissions and crossovers: infections occurred in 7.2% of patients that were treated on the ICU/IMC compared to 2.7% of patients that had avoided the ICU (p = 0.013). Incidences of postprocedural delirium (2.8 vs. 0%, p = 0.007) and in-hospital mortality (1.7 vs. 0%, p = 0.037) were also significantly higher in these patients. Furthermore, duration of the procedure or anesthesia was similar in patients with and without development of infection or delirium (median procedural duration: 75.0 (65.0 – 112.0) vs. 83.0 min (63.0 – 103.0), p = 0.53; median anesthesia duration: 120.0 (105.0 – 165.0) vs. 120.0 min (100.0 – 145.0), p = 0.57).
Crossover to unplanned ICU admission in the VU era
Fifty patients (16.0%) that were scheduled to be relocated to the VU following M-TEER instead had to be transferred to the ICU/IMC (crossover group). The most frequent indication for ICU/IMC treatment in these patients was requirement of catecholamines (52.0%) followed by prolonged ventilation (32.0%) (Fig. 3). Patients in the crossover group (see Table 2) were younger and more often male and had significantly more pronounced heart failure signs: higher baseline New York Heart Association (NYHA) functional class, lower LV-EF, higher prevalence of dilatative cardiomyopathy, and severe concomitant tricuspid regurgitation (TR). Their LV diameters were significantly larger, and Troponin T and NT-proBNP significantly higher. A significantly higher EuroSCORE II reflected the higher overall morbidity. Furthermore, procedural duration was significantly longer in these patients. There was no relevant difference in pre-procedural MR grade or device success rate. Median duration of the unscheduled ICU stay was 20.0 h (IQR 5.0 – 29.3 h). Two patients died while in hospital (4.0%).
Multivariate logistic regression analysis identified an LV-EF of < 30% as an independent predictor of unscheduled ICU/IMC admission (hazard ratio 2.941, 95% confidence interval 1.409 – 6.140, p = 0.004, Table 3).
Discussion
With the growing importance of M-TEER and its establishment as a routine intervention in experienced heart centers, a standardization of postprocedural care is necessary. Routine ICU monitoring after M-TEER has been suggested and is commonly performed, at least after procedures in GA [2]. However, ICU and IMC capacities are a valuable resource and clinicians might encounter the dilemma of maintaining optimal patient safety on the one hand and mindful use of ICU and IMC structures as well as cost-effectiveness on the other. Our data show that implementation of a dedicated VU for post-interventional monitoring is a reasonable option.
Immediate admission to the VU instead of primary ICU/IMC treatment after M-TEER was associated with a significantly shorter hospital stay and a lower incidence of infections and delirium. Importantly, these complications occurred irrespective of procedural duration or duration of anesthesia. Both adverse events are known to occur more frequently in patients treated in an ICU [11, 12]. In a study by Körber et al., periinterventional delirium was associated with longer hospital stay and higher risk for bleeding and periprocedural infections in patients undergoing M-TEER or T-TEER [13]. In our study, avoidance of ICU/IMC admission has certainly streamlined the postprocedural course and therefore shortened the time spent in hospital and the exposure to risk factors for infections and delirium. However, longer procedural and anesthesia duration and inferior procedural success rates in the ICU/IMC era might have prolonged hospital stay in this group.
Most importantly, in-hospital mortality in our study was non-inferior in VU patients compared to the ICU/IMC group. Thus, a step down in postprocedural surveillance does not come at the prize of impaired patient safety.
To date, the adequate postprocedural monitoring of M-TEER patients has not been studied well. Efforts to streamline interventional and periinterventional processes have mainly been made in TAVR patients [14,15,16]. In the context of M-TEER, data by Di Prima et al. have shown that while all patients in their study were admitted to an ICU after the intervention, 18.5% left the ICU on the same day due to an uneventful postprocedural course and 68.5% could be transferred to a general ward the day after [5]. Our data now show for the first time that routine ICU/IMC treatment following M-TEER in GA is not required in the majority of patients. In fact, only 16.0% of patients had to be admitted to the ICU/IMC while 84.0% received adequate postprocedural care on the VU. According to our data, however, patients with reduced LV-EF should be monitored closely as they have a significantly higher risk to require ICU or IMC treatment compared to patients with better systolic function.
Notably, the most frequent causes for unscheduled ICU/IMC transfer after M-TEER in our cohort were prolonged need for catecholamines and protracted weaning from mechanical ventilation. Both factors are closely related to GA. However, avoidance of GA and mechanical ventilation has been shown to be a feasible option especially for patients at higher risk for anesthesia-associated complications [17, 18]. In a meta-analysis, Banga et al. reported a shorter ICU stay and a comparable rate of procedural success by using conscious or deep sedation compared to GA [19]. As crossover to ICU/IMC treatment occurred significantly more frequently in patients with advanced heart failure, preferring sedation to GA might be a feasible option to further reduce ICU admissions in these high-risk patients. Though our study cannot report on the course of patients receiving M-TEER using deep sedation only, an additional benefit of ICU/IMC avoidance in these patients is conceivable.
The main differences in patient characteristics in the ICU/IMC and the VU era were procedure-related. Lower device success rates and longer duration of the procedure and anesthesia might have influenced outcomes. The superior procedural results in the VU era are likely due to substantial technical advances of TEER devices which have improved TEER results in general [20]. Significant differences in the choice of the TEER device are owed to the later market introduction of the PASCAL device, which was not yet used broadly in our center in the ICU/IMC era.
Study limitations
Our data resemble a retrospective study and while we report on a substantially sized cohort our findings are limited to a single-center experience. Further external evaluation of strategies of ICU/IMC avoidance after M-TEER should be sought to validate our conclusions. Secondly, a potential bias may arise from the long period of time included in our analysis and the respective technical and procedural advancements in this era. Furthermore, certain important complications such as bleeding have not been routinely registered throughout the observation period and are therefore not included in this study.
Conclusions
Implementation of a VU for postprocedural monitoring after M-TEER instead of primary routine ICU/IMC admission maintains patient safety, reduces complications, and may even reduce hospital stay. Patients with advanced heart failure have a higher risk of unplanned crossover to ICU/IMC treatment and an LV-EF of < 30% is an independent predictor of ICU/IMC admission. Use of a VU as a standardized target structure for M-TEER patients may help to streamline the procedure, reduce healthcare costs, and spare ICU capacities.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J et al (2022) 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 43(7):561–632
Boekstegers P, Hausleiter J, Baldus S, von Bardeleben RS, Beucher H, Butter C et al (2014) Percutaneous interventional mitral regurgitation treatment using the Mitra-Clip system. Clin Res Cardiol 103(2):85–96
Ledwoch J, Matic P, Franke J, Gafoor S, Bertog S, Reinartz M (2016) Transcatheter mitral valve repair with the MitraClip(®) can be performed without general anesthesia and without conscious sedation. Clin Res Cardiol 105(4):297–306
Horn P, Hellhammer K, Minier M, Stenzel MA, Veulemans V, Rassaf T et al (2017) Deep sedation vs. general anesthesia in 232 patients undergoing percutaneous mitral valve repair using the MitraClip® system. Catheter Cardiovasc Interv 90(7):1212–9
Di Prima AL, Covello DR, Franco A, Gerli C, Lembo R, Denti P et al (2014) Do patients undergoing MitraClip implantation require routine ICU admission? J Cardiothorac Vasc Anesth 28(6):1479–1483
Schnitzler K, Hell M, Geyer M, Kreidel F, Münzel T, von Bardeleben RS (2021) Complications following MitraClip implantation. Curr Cardiol Rep 23(9):131
Körber MI, Silwedel J, Friedrichs K, Mauri V, Huntgeburth M, Pfister R et al (2018) Bleeding complications after percutaneous mitral valve repair with the MitraClip. Am J Cardiol 121(1):94–99
Arabi YM, Azoulay E, Al-Dorzi HM, Phua J, Salluh J, Binnie A et al (2021) How the COVID-19 pandemic will change the future of critical care. Intensive Care Med 47(3):282–291
Lancellotti P, Pibarot P, Chambers J, La Canna G, Pepi M, Dulgheru R et al (2022) Multi-modality imaging assessment of native valvular regurgitation: an EACVI and ESC council of valvular heart disease position paper. Eur Heart J Cardiovasc Imaging 23(5):e171-232
Stone GW, Adams DH, Abraham WT, Kappetein AT, Genereux P, Vranckx P et al (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 2: endpoint definitions: a consensus document from the Mitral Valve Academic Research Consortium. Eur Heart J 36(29):1878–1891
Mart MF, Williams Roberson S, Salas B, Pandharipande PP, Ely EW (2021) Prevention and management of delirium in the intensive care unit. Semin Respir Crit Care Med 42(1):112–126
Mazzeffi M, Galvagno S, Rock C (2021) Prevention of healthcare-associated infections in intensive care unit patients. Anesthesiology 135(6):1122–1131
Körber MI, Schäfer M, Vimalathasan R, Mauri V, Iliadis C, Metze C et al (2021) Periinterventional inflammation and blood transfusions predict postprocedural delirium after percutaneous repair of mitral and tricuspid valves. Clin Res Cardiol 110(12):1921–1929
Wong I, Chiang M, Chui ASF, Chan AKC, Chan KT, Lee MKY (2023) Simplified pacing-over-the-wire technique to streamline TAVR with sentinel cerebral protection device: the SENTIPACE approach. JACC Cardiovasc Interv 16(2):226–228
Leclerq F, Meunier PA, Gandet T, Macia JC, Delseny D, Gaudard P et al (2022) Simplified TAVR procedure: how far is it possible to go? J Clin Med 11(10):2793
Lauck SB, Sathananthan J, Park J, Achtem L, Smith A, Keegan P et al (2020) Post-procedure protocol to facilitate next-day discharge: results of the multidisciplinary, multimodality but minimalist TAVR study. Catheter Cardiovasc Interv 96(2):450–458
Teufel T, Steinberg DH, Wunderlich N, Doss M, Fichtlscherer S, Ledwoch J et al (2012) Percutaneous mitral valve repair with the MitraClip® system under deep sedation and local anaesthesia. EuroIntervention 8(5):587–590
Rassaf T, Balzer J, Zeus T, Rammos C, Shayganfar S, Hall SV et al (2014) Safety and efficacy of deep sedation as compared to general anaesthesia in percutaneous mitral valve repair using the MitraClip system. Catheter Cardiovasc Interv 84(4):E38-42
Banga S, Hafiz AM, Chami Y, Gumm DC, Banga P, Howard C et al (2020) Comparing sedation vs. general anaesthesia in transoesophageal echocardiography-guided percutaneous transcatheter mitral valve repair: a meta-analysis. Eur Heart J Cardiovasc Imaging 21(5):511–21
Orban M, Lüsebrink E, Braun D, Stocker TJ, Bagaev E, Hagl C et al (2020) Recent advances in patient selection and devices for transcatheter edge-to-edge mitral valve repair in heart failure. Expert Rev Med Devices 17(2):93–102
Acknowledgements
We thank Uta Dichristin for study coordination and data management.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
All patients included in this study provided written informed consent for scientific use of their data.
Conflict of interest
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gröger, M., Felbel, D., Paukovitsch, M. et al. Valve unit instead of intensive or intermediate care unit admission following transcatheter edge-to-edge mitral valve repair is safe and reduces postprocedural complications. Clin Res Cardiol (2024). https://doi.org/10.1007/s00392-024-02384-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-024-02384-8