Abstract
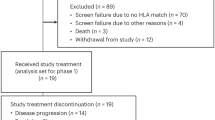
Based on the demonstrated clinical activity of immune-checkpoint blockade (ICB) in advanced dedifferentiated liposarcoma (DDLPS) and undifferentiated pleomorphic sarcoma (UPS), we conducted a randomized, non-comparative phase 2 trial (NCT03307616) of neoadjuvant nivolumab or nivolumab/ipilimumab in patients with resectable retroperitoneal DDLPS (n = 17) and extremity/truncal UPS (+ concurrent nivolumab/radiation therapy; n = 10). The primary end point of pathologic response (percent hyalinization) was a median of 8.8% in DDLPS and 89% in UPS. Secondary end points were the changes in immune infiltrate, radiographic response, 12- and 24-month relapse-free survival and overall survival. Lower densities of regulatory T cells before treatment were associated with a major pathologic response (hyalinization > 30%). Tumor infiltration by B cells was increased following neoadjuvant treatment and was associated with overall survival in DDLPS. B cell infiltration was associated with higher densities of regulatory T cells before treatment, which was lost upon ICB treatment. Our data demonstrate that neoadjuvant ICB is associated with complex immune changes within the tumor microenvironment in DDLPS and UPS and that neoadjuvant ICB with concurrent radiotherapy has significant efficacy in UPS.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The data supporting the findings of this study are available within the manuscript and its supplementary information files. RNA-seq data that support the findings of this study have been deposited in the Gene Expression Omnibus under accession code GSE202361. All other relevant de-identified data related to the current study are available from the corresponding author (C.L.R.) upon reasonable request (including compelling scientific rationale and preliminary data requiring validation through use of this cohort; these preliminary data should be presented to the authors) and will require the researcher to sign a data access agreement with The University of Texas MD Anderson Cancer Center after approval. Individual patient identifiable clinical data (such as dates) are not publicly available due to concerns with identification of patients.
The hg19 human genome can be found at https://www.ncbi.nlm.nih.gov/datasets/genome/GCF_000001405.13/.
Source data for all figures and extended data have been provided as Source Data files. Source data are provided with this paper.
References
Blay, J. Y. et al. Improved survival using specialized multidisciplinary board in sarcoma patients. Ann. Oncol. 28, 2852–2859 (2017).
Gronchi, A. et al. Histotype-tailored neoadjuvant chemotherapy versus standard chemotherapy in patients with high-risk soft-tissue sarcomas (ISG-STS 1001): an international, open-label, randomised, controlled, phase 3, multicentre trial. Lancet Oncol. 18, 812–822 (2017).
World Health Organization. WHO Classification of Tumours: Soft Tissue and Bone Tumours 5th edn, Vol 3 (International Agency for Research on Cancer, 2020).
Tawbi, H. A. et al. Pembrolizumab in advanced soft-tissue sarcoma and bone sarcoma (SARC028): a multicentre, two-cohort, single-arm, open-label, phase 2 trial. Lancet Oncol. 18, 1493–1501 (2017).
Burgess, M. A. et al. Clinical activity of pembrolizumab (P) in undifferentiated pleomorphic sarcoma (UPS) and dedifferentiated/pleomorphic liposarcoma (LPS): final results of SARC028 expansion cohorts. J. Clin. Oncol. 37, 11015 (2019).
D’Angelo, S. P. et al. Antitumor activity associated with prolonged persistence of adoptively transferred NY-ESO-1 (c259)T cells in synovial sarcoma. Cancer Discov. 8, 944–957 (2018).
Roulleaux Dugage, M. et al. Improving immunotherapy efficacy in soft-tissue sarcomas: a biomarker driven and histotype tailored review. Front. Immunol. 12, 775761 (2021).
Keung, E. Z. et al. Correlative analyses of the SARC028 trial reveal an association between sarcoma-associated immune infiltrate and response to pembrolizumab. Clin. Cancer Res. 26, 1258–1266 (2020).
Somaiah, N. et al. Durvalumab plus tremelimumab in advanced or metastatic soft tissue and bone sarcomas: a single-centre phase 2 trial. Lancet Oncol. 23, 1156–1166 (2022).
Petitprez, F. et al. B cells are associated with survival and immunotherapy response in sarcoma. Nature 577, 556–560 (2020).
Italiano, A. et al. PD1 inhibition in soft-tissue sarcomas with tertiary lymphoid structures: a multicenter phase II trial. J. Clin. Oncol. 39, 11507 (2021).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Schaefer, I.-M. et al. Histologic appearance after preoperative radiation therapy for soft tissue sarcoma: assessment of the European organization for research and treatment of cancer–soft tissue and bone sarcoma group response score. Int. J. Radiat. Oncol. Biol. Phys. 98, 375–383 (2017).
Rao, S. R. et al. Extent of tumor fibrosis/hyalinization and infarction following neoadjuvant radiation therapy is associated with improved survival in patients with soft‐tissue sarcoma. Cancer Med. 11, 194–206 (2021).
Toulmonde, M. et al. Use of PD-1 targeting, macrophage infiltration, and IDO pathway activation in sarcomas: a phase 2 clinical trial. JAMA Oncol. 4, 93–97 (2018).
McGranahan, N. & Swanton, C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell 168, 613–628 (2017).
Amaria, R. N. et al. Neoadjuvant immune checkpoint blockade in high-risk resectable melanoma. Nat. Med. 24, 1649–1654 (2018).
Cascone, T. et al. Neoadjuvant nivolumab or nivolumab plus ipilimumab in operable non-small cell lung cancer: the phase 2 randomized NEOSTAR trial. Nat. Med. 27, 504–514 (2021).
Ferrarotto, R. et al. Pilot phase II trial of neoadjuvant immunotherapy in locoregionally advanced, resectable cutaneous squamous cell carcinoma of the head and neck. Clin. Cancer Res. 27, 4557–4565 (2021).
Gross, N. D. et al. Neoadjuvant cemiplimab for stage II to IV cutaneous squamous-cell carcinoma. New Engl. J. Med. 387, 1557–1568 (2022).
Patel, S. P. et al. Neoadjuvant–adjuvant or adjuvant-only pembrolizumab in advanced melanoma. New Engl. J. Med. 388, 813–823 (2023).
Chalabi, M. et al. LBA7 Neoadjuvant immune checkpoint inhibition in locally advanced MMR-deficient colon cancer: the NICHE-2 study. Ann. Oncol. 33, S1389 (2022).
Keung, E. Z. et al. The rationale and emerging use of neoadjuvant immune checkpoint blockade for solid malignancies. Ann. Surg. Oncol. 25, 1814–1827 (2018).
Topalian, S. L., Taube, J. M. & Pardoll, D. M. Neoadjuvant checkpoint blockade for cancer immunotherapy. Science 367, eaax0182 (2020).
Keung, E. Z. et al. Analysis of the immune infiltrate in undifferentiated pleomorphic sarcoma of the extremity and trunk in response to radiotherapy: rationale for combination neoadjuvant immune checkpoint inhibition and radiotherapy. Oncoimmunology 7, e1385689 (2018).
Raut, C. P. et al. Predicting survival in patients undergoing resection for locally recurrent retroperitoneal sarcoma: a study and novel nomogram from TARPSWG. Clin. Cancer Res. 25, 2664–2671 (2019).
Bonvalot, S. et al. Preoperative radiotherapy plus surgery versus surgery alone for patients with primary retroperitoneal sarcoma (EORTC-62092: STRASS): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 21, 1366–1377 (2020).
Rodriguez-Ruiz, M. E. et al. Immunological impact of cell death signaling driven by radiation on the tumor microenvironment. Nat. Immunol. 21, 120–134 (2020).
Theelen, W. S. M. E. et al. Pembrolizumab with or without radiotherapy for metastatic non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Respir. Med. 9, 467–475 (2021).
Mowery, Y. M. et al. SU2C-SARC032: a phase II randomized controlled trial of neoadjuvant pembrolizumab with radiotherapy and adjuvant pembrolizumab for high-risk soft tissue sarcoma. J. Clin. Oncol. 36, TPS11588–TPS11588 (2018).
D’Angelo, S. P. et al. Nivolumab with or without ipilimumab treatment for metastatic sarcoma (Alliance A091401): two open-label, non-comparative, randomised, phase 2 trials. Lancet Oncol. 19, 416–426 (2018).
Stacchiotti, S. et al. High-grade soft-tissue sarcomas: tumor response assessment—pilot study to assess the correlation between radiologic and pathologic response by using RECIST and Choi criteria. Radiology 251, 447–456 (2009).
Taieb, S. et al. Comparison of response evaluation criteria in Solid Tumours and Choi criteria for response evaluation in patients with advanced soft tissue sarcoma treated with trabectedin: a retrospective analysis. Eur. J. Cancer 51, 202–209 (2015).
Le Lay, J. et al. irRECIST and iRECIST: the devil is in the details. Ann. Oncol. 28, 1676–1678 (2017).
Nishino, M. et al. Monitoring immune-checkpoint blockade: response evaluation and biomarker development. Nat. Rev. Clin. Oncol. 14, 655–668 (2017).
Bertucci, F. et al. PDL1 expression is a poor-prognosis factor in soft-tissue sarcomas. Oncoimmunology 6, e1278100 (2017).
Kim, C. et al. Prognostic implications of PD-L1 expression in patients with soft tissue sarcoma. BMC Cancer 16, 434 (2016).
Pollack, S. M. et al. T-cell infiltration and clonality correlate with programmed cell death protein 1 and programmed death-ligand 1 expression in patients with soft tissue sarcomas. Cancer 123, 3291–3304 (2017).
Kelly, C. M. et al. Objective response rate among patients with locally advanced or metastatic sarcoma treated with talimogene laherparepvec in combination with pembrolizumab. JAMA Oncol. 6, 402–408 (2020).
Wing, J. B. et al. A distinct subpopulation of CD25− T-follicular regulatory cells localizes in the germinal centers. Proc. Natl Acad. Sci. USA 114, E6400–E6409 (2017).
Eschweiler, S. et al. Intratumoral follicular regulatory T cells curtail anti-PD-1 treatment efficacy. Nat. Immunol. 22, 1052–1063 (2021).
Facciabene, A., Motz, G. T. & Coukos, G. T-regulatory cells: key players in tumor immune escape and angiogenesis. Cancer Res. 72, 2162–2171 (2012).
Kawakami, R. et al. Distinct Foxp3 enhancer elements coordinate development, maintenance, and function of regulatory T cells. Immunity 54, 947–961 (2021).
Hindley, J. P. et al. T-cell trafficking facilitated by high endothelial venules is required for tumor control after regulatory T-cell depletion. Cancer Res. 72, 5473–5482 (2012).
Joshi, N. S. et al. Regulatory T cells in tumor-associated tertiary lymphoid structures suppress anti-tumor T cell responses. Immunity 43, 579–590 (2015).
Italiano, A. et al. Pembrolizumab in soft-tissue sarcomas with tertiary lymphoid structures: a phase 2 PEMBROSARC trial cohort. Nat. Med. 28, 1199–1206 (2022).
Schulz, K. F., Altman, D. G. & Moher, D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Brit. Med. J. 340, c332 (2010).
Lin, D. Y., Wei, L.-J. & Ying, Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika 80, 557–572 (1993).
Levene, H. in Contributions to Probability and Statistics 278–292 (Stanford Univ. Press, 1960).
Wickham, H., François, R., Henry, L. & Müller, K. dplyr: A Grammar of Data Manipulation. R package v.1.1.4 https://dplyr.tidyverse.org (2022).
Kassambara, A. rstatix: Pipe-Friendly Framework for Basic Statistical Tests https://cran.r-project.org/web/packages/rstatix/index.html (2021).
Kassambara, A. ggplot2-Based Publication Ready Plots https://cran.r-project.org/web/packages/ggpubr/readme/README.html (2020).
Wickham, H. ggplot2: Elegant Graphics for Data Analysis (Springer, 2009).
Harris, P. A. et al. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
Harris, P. A. et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inform. 95, 103208 (2019).
Wardelmann, E. et al. Evaluation of response after neoadjuvant treatment in soft tissue sarcomas; the European Organization for Research and Treatment of Cancer–Soft Tissue and Bone Sarcoma Group (EORTC–STBSG) recommendations for pathological examination and reporting. Eur. J. Cancer 53, 84–95 (2016).
Parra, E. R. et al. Identification of distinct immune landscapes using an automated nine-color multiplex immunofluorescence staining panel and image analysis in paraffin tumor tissues. Sci. Rep. 11, 4530 (2021).
Parra, E. R. et al. Immuno-profiling and cellular spatial analysis using five immune oncology multiplex immunofluorescence panels for paraffin tumor tissue. Sci. Rep. 11, 8511 (2021).
Parra, E. R. et al. Procedural requirements and recommendations for multiplex immunofluorescence tyramide signal amplification assays to support translational oncology studies. Cancers 12, 255 (2020).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Liao, Y., Smyth, G. K. & Shi, W. featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30, 923–930 (2013).
Shugay, M. et al. Oncofuse: a computational framework for the prediction of the oncogenic potential of gene fusions. Bioinformatics 29, 2539–2546 (2013).
Okonechnikov, K., Conesa, A. & Garcia-Alcalde, F. Qualimap 2: advanced multi-sample quality control for high-throughput sequencing data. Bioinformatics 32, 292–294, (2016).
Wang, Q., Jia, P. & Zhao, Z. VirusFinder: software for efficient and accurate detection of viruses and their integration sites in host genomes through next generation sequencing data. PLoS ONE 8, e64465 (2013).
Bhaduri, A. et al. Rapid identification of non-human sequences in high-throughput sequencing datasets. Bioinformatics 28, 1174–1175 (2012).
Charoentong, P. et al. Pan-cancer immunogenomic analyses reveal genotype-immunophenotype relationships and predictors of response to checkpoint blockade. Cell Rep. 18, 248–262 (2017).
Acknowledgements
We thank the patients and their families for participating in this study. We thank all the members of our regulatory, clinical, data coordination and translational research teams in the Departments of Surgical Oncology and Sarcoma Medical Oncology at The University of Texas MD Anderson Cancer Center for their support on this trial. The clinical aspects of the study were funded by Bristol-Myers Squibb (drug and funding). Presequencing processing work was carried out by the Moon Shots Platform Cancer Genomics Laboratory, The University of Texas MD Anderson Cancer Center Sheikh Khalifa Bin Zayed Al Nahyan Institute for Personalized Cancer Therapy. Sequencing and data generation was supported by a CA016672 (ATGC) grant from The University of Texas MD Anderson Cancer Center, Advanced Technology Genomics Core. This translational analysis was supported by the Rare Tumor Initiative, an MD Anderson Strategic Research Initiative Development Program Microbiome samples were processed by MD Anderson Cancer Center’s Program for Innovative Microbiome and Translational Research. Support for the study was also partially provided by the National Institutes of Health (NIH)/National Cancer Institute (NCI) P30 CA016672 Cancer Center Support Grant. J.A.W. is supported by the NIH (1 R01 CA219896-01A1), US–Israel Binational Science Foundation (201332), the Melanoma Research Alliance (4022024), American Association for Cancer Research Stand Up To Cancer (SU2C-AACR-IRG-19-17), Department of Defense (W81XWH-16-1-0121), MD Anderson Cancer Center Multidisciplinary Research Program Grant, Andrew Sabin Family Fellows Program and MD Anderson Cancer Center’s Melanoma Moon Shots Program. C.L.R. received support from NIH/NCI The Paul Calabresi K12 Career Development Award CA088084-16A1, The Society of Surgical Oncology Clinical Investigator Award and The American College of Surgeons Faculty Research Fellowship. E.F.N.H. received support from the LMS SPORE Career Enhancement Program, the QuadW foundation, Sarcoma Foundation of America, Fondation pour la Recherche Medicale and Fondation Nuovo-Soldati. E.Z.K. received grant support from the QuadW foundation, Sarcoma Foundation of America, Fondation pour la Recherche Medicale and the NCI Early Surgeon Scientist Program.
Author information
Authors and Affiliations
Contributions
C.L.R., E.Z.K., H.A.T., E.M.B., J.A.W., B.A.G., A.J.B. and N.S. designed the study. C.L.R. and N.S. were the principal investigators. E.Z.K. was a co-principal investigator. H.Y.L. conducted the statistical design and analyses. C.L.R., N.S., E.Z.K., A.P.C., R.R., M.A.Z. and J.A.L. recruited patients. B.A.G., A.J.B., K.K.H., K.E.T., B.W.F., C.P.S., V.O.L., J.E.B., R.R., D.A.J., M.A.Z., S.P., R.B., A.P.C., J.A.L., V.R., P.P.L., B.S.M., T.T., K.C. and R.L.S. treated patients. E.Z.K., A.J.L., W.L.W., E.R.P., K.W., D.I. and E.F.N.H. collected and analyzed the translational data. W.L.W., A.J.L., E.R.P., K.W., R.L., D.I., R.M. and C.F.L. performed pathologic evaluation, IHC staining and interpretation, mIF staining and interpretation. B.M. interpreted the imaging evaluations. M.C., C.C.W., M.M.M., R.A.C., J.Z., A.D., P.S., S.C., G.M., S.D., K.S., I.W., A.F. and N.A. collected, handled and analyzed samples for genomic analyses. E.F.N.H., C.L.R., E.Z.K. and N.S. wrote the manuscript. E.F.N.H., E.Z.K., C.L.R., S.N., H.Y.L. and N.S. had access to the data. E.F.N.H., E.Z.K. and C.L.R. accessed and verified the data. M.C., R.G.W., R.S.T. and B.C. edited the figures and the manuscript. All authors contributed to editing the manuscript and gave final approval for the article.
Corresponding author
Ethics declarations
Competing interests
This study was supported by Bristol-Myers Squibb. A.J.L. has served on advisory boards and/or consulted for AbbVie, Adaptimmune, ArcherDX, AstraZeneca, Bayer, BMS, Deciphera Pharmaceuticals, Foghorn Therapeutics, Gothams, GSK, Guardant, Invitae, Illumina, Iterion Therapeutics, Merck, Novartis, Nucleai, Paige.AI, Pfizer, Roche/Genentech and Thermo Fisher. K.K.H. is on the medical advisory board for Armada Health and AstraZeneca and reports research funding to The MD Anderson Cancer Center from Cairn Surgical, Eli Lilly & Co. and Lumicell. D.A. receives research funding from Adaptimmune, GSK and Immatics. H.T. received grant or research support from BMS, Novartis, Merck, Genentech, GlaxoSmithKline, EMD Sereno, Eisai, Dragonfly Therapeutics, RAPT Therapeutics; and is a consultant for BMS, Genentech, Novartis, Merck, Boxer Capital, Karyopharm, Iovance, Eisai, Jazz Pharmaceuticals and Medicenna. R.G.W. is supported by the NIH T32 CA 009599 and The MD Anderson Cancer Center support grant P30 CA016672. J.Y.B. has received research support and honoraria from Roche, GlaxoSmithKline, BMS and MSD. W.H.F. is a consultant for Novartis, Adaptimmune, Anaveon, Catalym, OSE Immunotherapeutic, Oxford Biotherapeutics, Genenta and Parthenon. K.S. is a consultant for Guidepoint, GLG, BlueprintBiomedicines and Coleman and is on the editorial committee for a CSHP publication. I.W. has provided consulting or advisory roles for AstraZeneca/MedImmune, Bayer, Bristol-Myers Squibb, Genentech/Roche, GlaxoSmithKline, Guardant Health, HTG Molecular Diagnostics, Merck, MSD Oncology, OncoCyte, Jansen, Novartis, Flame and Pfizer; has received grants and personal fees from Genentech/Roche, Bristol-Myers Squibb, AstraZeneca/MedImmune, HTG Molecular, Merck and Guardant Health; has received personal fees from GlaxoSmithKline and Oncocyte, Daiichi Sankyo, Roche, AstraZeneca, Pfizer and Bayer; and has received research funding to his institution from 4D Molecular Therapeutics, Adaptimmune, Adaptive Biotechnologies, Akoya Biosciences, Amgen, Bayer, EMD Serono, Genentech, Guardant Health, HTG Molecular Diagnostics, Iovance Biotherapeutics, Johnson & Johnson, Karus Therapeutics, MedImmune, Merck, Novartis, OncoPlex Diagnostics, Pfizer, Takeda and Novartis. J.A.W. reports compensation for speaker’s bureau and honoraria from Imedex, Dava Oncology, Omniprex, Illumina, Gilead, PeerView, Physician Education Resource, MedImmune and Bristol-Myers Squibb; is on the advisory board as a consultant for Roche/Genentech, Novartis, AstraZeneca, GlaxoSmithKline, Bristol-Myers Squibb, Merck, Micronoma and Biothera Pharmaceuticals; and has stock options for Micronoma. N.S. is on the advisory board as a consultant for Deciphera, AADI Biosciences, Epizyme and Boehringer Ingelheim; receives research funding from Decipehra, Daiichi Sankyo, Karyopharm, AstraZeneca, Cogent Biosciences, Ascentage and GSK; and has an immediate family member with stock options from Pfizer and JNJ.
Peer review
Peer review information
Nature Cancer thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Maximum-Grade Treatment-Related Adverse Events.
Frequencies of maximum-grade treatment-related adverse events (TRAEs) in the whole cohort of patients in ascending shades of blue (nivolumab arms) and red (ipilimumab/nivolumab arms) for grades 1 to 3. There were no grade 4 or 5 TRAEs in this trial. All adverse events that were possibly or probably related to treatment are reported. All patients (n = 27) were included in this analysis.
Extended Data Fig. 2 Pathologic response evaluation by hyalinization and correlation with other response criteria.
a, Patient-level pathological data showing percent hyalinization, percent viable tumor, and percent necrosis of surgical specimens in the ITT population (n = 27) in DDLPS (left panels) and UPS (right panels) patients. Patient 29 had clinical progression with lung metastasis treated by chemotherapy, followed by surgery off trial. b, Correlation between percent viable tumor and percent hyalinization at surgery. Two-sided p-value is Spearman rank-order correlation test. Gray zone is 95% CI. c, Correlation between overall change in tumor size from baseline at least 14 days after last dose assessed by RECIST1.1 and percent hyalinization at surgery. Dots are in ascending size of percent viable tumor at surgery. Two-sided p-value is Spearman rank-order correlation test. Gray zone is 95% CI. d, Table reporting pathologic response and early relapse in patients treated in arm B, according to the dose of ipilimumab received. P values are two-sided. e, Table reporting pathologic response and early relapse in patients treated in arm D, according to the dose of ipilimumab received. P values are two-sided.
Extended Data Fig. 3 Survival outcomes and association with RECIST response, pathologic response, and resistance.
a, Kaplan-Meier curves of OS in DDLPS patients treated with nivolumab (n = 8) and ipilimumab/nivolumab (n = 9) from surgery (on-trial and off trial) to death. b, Kaplan-Meier curves of OS in UPS patients treated with nivolumab + RT (n = 6) and ipilimumab/nivolumab followed by nivolumab + RT (n = 4). c, Kaplan-Meier curves of RFS according to radiographic response (PD, SD, PR) as assessed by RECIST1.1 from baseline at least 14 days after last dose in DDLPS patients (left panel) and UPS patients (right panel). Two-sided p values indicate log-rank comparison. d, Kaplan-Meier curves of OS according to radiographic response (PD, SD, PR) as assessed by RECIST1.1 from baseline at least 14 days after last dose in DDLPS patients (left panels), and UPS patients (right panels). Two-sided p values indicate log-rank comparison. e, Kaplan-Meier curves of RFS according to dose of ipilimumab and nivolumab received in DDLPS patients (arm B; left panel) and UPS patients (arm D; right panel). Two-sided p values indicate log-rank comparison. f, Kaplan-Meier curves of OS according to dose of ipilimumab and nivolumab received in DDLPS patients (arm B; left panel) and UPS patients (arm D; right panel). Two-sided p values indicate log-rank comparison. g, Kaplan-Meier curves of RFS (left panel) and OS (right panel) according to disease status at initiation of treatment (primary versus recurrent) in DDLPS. Two-sided p values indicate log-rank comparison. h, Kaplan-Meier curves of RFS (left panel) and OS (right panel) according to focality at initiation of treatment in DDLPS patients. Two-sided p values indicate log-rank comparison.
Extended Data Fig. 4 Association of tumor PD-L1 expression by IHC in malignant cells with oncological outcomes and immune infiltration.
a, Number of samples with positive (≥1%) and negative (<1%) PD-L1 IHC staining on malignant cells by clone 28-8 at each time point in DDLPS (left panel) and UPS (right panel) patients. b, Table displaying oncological efficacy end points in DDLPS and UPS patients with baseline PD-L1 positive and negative tumors. PD-L1 positive tumors were defined as those with ≥1% on expression on malignant cells by IHC with clone 28-8. Two-sided p values are Wilcoxon rank-sum tests and Fisher’s exact tests. c, d, Kaplan-Meier curves of probability of RFS from surgery to relapse or death according to positivity of PD-L1 staining on tumor cells at baseline, in (c) DDLPS and (d) UPS patients. P values indicate log-rank comparison of survival curves. e, Kaplan-Meier curves of probability of RFS from surgery to relapse or death according to positivity of PD-L1 staining on tumor cells at baseline, in DDLPS patients with primary tumors (left panel) or recurrent tumors (right panel) at initiation of treatment. Two-sided p values indicate log-rank comparison of survival curves. f, Kaplan-Meier curves of probability of RFS from surgery to relapse or death according to positivity of PD-L1 staining on tumor cells at baseline, in DDLPS patients with unifocal (left panel) or multifocal tumors (right panel) at initiation of treatment. Two-sided p values indicate log-rank comparison of survival curves.
Extended Data Fig. 5 Association of immune cell densities with pathologic response.
a, Example of mIF images of T cells (CD3+), activated T cells (CD3 + Ki67+), CD8+ cells, activated cytotoxic T cells (CD3 + CD8 + Ki67+), PD-L1 positive cytotoxic T cells (CD3 + CD8 + PD-L1+), antigen-experienced T cells (CD3 + PD-1+), memory T cells (CD3 + CD45RO + CD8-), macrophages (CD68+), and PD-L1 positive macrophages (CD68 + PD-L1+). Scale shows 50 μm. b–d, Absolute densities (/mm2) of (b) tumor-associated macrophages (CD68+), (c) activated macrophages (CD68 + Ki67+), and PD-L1+ macrophages (CD68 + PD-L1+) in pathologic responders (≥30% hyalinization; blue dots and blue circles) and non-responders (red dots and red circles) at each time point (baseline, on-treatment, and surgery) in DDLPS (circles) and UPS (dots) patients. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Two-sided p values are Wilcoxon rank-sum test comparisons of densities of cells. e–g, Absolute densities (/mm2) of (b) tumor-associated macrophages (CD68+), (c) activated macrophages (CD68 + Ki67+), and PD-L1+ macrophages (CD68 + PD-L1+) in pathologic responders (≥30% hyalinization) and non-responders at each time point (baseline, on-treatment, and surgery) in DDLPS (top panels) and UPS (bottom panels) patients. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Two-sided p values are Wilcoxon rank-sum test comparisons of densities of cells.
Extended Data Fig. 6 Intratumor infiltrating cytotoxic T cells and T-regulatory cells in subgroups of DDLPS.
a, Kaplan-Meier curves of RFS, according to baseline intratumoral relative density of cytotoxic T cells (CD3 + CD8+) in primary (left panel) and recurrent (right panel) DDLPS patients. Two-sided p values indicate log-rank comparison. b, Absolute densities (/mm2) of cytotoxic T cells (CD3 + CD8+) in primary and recurrent DDLPS at each time point. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Two-sided p values are Wilcoxon rank-sum test comparisons. c, Kaplan-Meier curves of RFS, according to baseline intratumoral relative density of cytotoxic T cells (CD3 + CD8+) in unifocal (left panel) and multifocal (right panel) DDLPS patients. Two-sided p values indicate log-rank comparison. d, Absolute densities (/mm2) of intratumoral cytotoxic T cells (CD3 + CD8+) in unifocal and multifocal DDLPS at each time point. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Two-sided p values are Wilcoxon rank-sum test comparisons. e, Kaplan-Meier curves of RFS, according to baseline intratumoral relative density of T-regs (CD3+FoxP3 + CD8-) in primary (left panel) and recurrent (right panel) DDLPS patients. Two-sided p values indicate log-rank comparison. f, Absolute densities (/mm2) of intratumoral T-regs (CD3+FoxP3 + CD8-) in primary and recurrent DDLPS at each time point. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Two-sided p values are Wilcoxon rank-sum test comparisons. g, Kaplan-Meier curves of RFS, according to baseline intratumoral relative density of T-regs (CD3+FoxP3 + CD8-) in unifocal (left panel) and multifocal (right panel) DDLPS patients. Two-sided p values indicate log-rank comparison of survival curves. h, Absolute densities (/mm2) of intratumoral T-regs (CD3+FoxP3 + CD8-) in unifocal and multifocal DDLPS at each time point. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Two-sided p values are Wilcoxon rank-sum test comparisons.
Extended Data Fig. 7 Patterns of therapy-induced changes in intratumoral immune cells infiltration.
a, Absolute densities (/mm2) of intratumoral immune cells across treatment time points (baseline [BL], on-treatment [OT], and surgery [Surg]) in DDLPS and UPS patients. Dashed lines indicate paired samples. Colors indicate pathologic response. Two-sided p values are Kruskal–Wallis test for comparisons of immune densities across time points, adjusted for multiple comparison by FDR. b, c, Unsupervised hierarchical clustering of tumor specimens based on intratumoral immune densities of selected immune cell populations assessed by mIF at all time points in (b) DDLPS and (c) UPS patients. Absolute densities of immune cell populations have been scaled. Red shows higher densities of immune cells and blue indicates lower densities of immune cells. Annotations include early relapse status, presence of TLS features by IHC, and time point of tumor specimen collection.
Extended Data Fig. 8 Association of intratumoral T-cell and macrophage densities with presence of intratumoral TLS and survival outcomes.
a, Absolute densities (/mm2) of intratumoral T cells and macrophages in samples displaying B cell aggregates with TLS features by CD20 and CD21 IHC (blue circles and blue dots) and samples without B cell and TLS features by IHC (red dots and red circles), at each time point (baseline, on-treatment, and surgery). Data are presented as minima from maxima, and solid line in the violin plot indicates median. Empty circles indicate DDLPS, solid dots indicate UPS. Two-sided p values are Wilcoxon rank-sum test comparisons of densities of cells between samples with or without TLS, adjusted for multiple comparison by FDR. b, Kaplan-Meier curves of probability of RFS (left panels) and OS from surgery to death (right panel) according to presence of B cell aggregates with TLS features by CD20 and CD21 IHC in tumor specimens of DDLPS patients at baseline. Two-sided p values indicate log-rank comparison of survival curves. c,d, Kaplan-Meier curves of probability of RFS (left panels) and overall survival from surgery to death (right panels) according to high (top quartile) or low (remaining quartiles) RNA-seq ssGSEA signature scores of TLS in baseline tumor specimens of (c) DDLPS and (d) UPS patients. Two-sided p values indicate log-rank comparison of survival curves.
Extended Data Fig. 9 Intratumoral B cells and TLS subgroup analyses and intratumor heterogeneity.
a, Proportion of tumor specimens showing presence of B cell aggregates with TLS features assessed by CD20 and CD21 IHC at each time point in DDLPS patients with primary (top panels) and recurrent tumors (bottom panels). Samples which did not pass quality control for analysis by IHC are not represented. b, Proportion of tumor specimens showing presence of TLS features assessed by CD20 and CD21 IHC at each time point in DDLPS patients with unifocal (top panels) and multifocal tumors (bottom panels). Samples which did not pass quality control for analysis by IHC are not represented. c–f, Kaplan-Meier curves of OS according to presence of TLS features by CD20 and CD21 IHC in tumor specimens of DDLPS patients at surgery in (c) primary, (d) recurrent, (e) unifocal, and (f) multifocal tumors. Two-sided p values indicate log-rank comparison. g, Mean number of lymphoid aggregates by H&E per slide at surgery in patients with (blue dots and blue circles; n = 5) and without (red dots and red circles; n = 12) positive evaluation of TLS features by CD20/CD21 IHC. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Empty circles indicate DDLPS (n = 9), solid dots indicate UPS (n = 9). Two-sided p values are Wilcoxon rank-sum test comparisons of densities of cells between samples with or without TLS. h, Patient-level representation of the number of lymphoid aggregates by H&E per slide for each block of the surgical resection in patients with (blue dots; n = 5) and without (red dots; n = 12) positive evaluation of TLS features by CD20/CD21 IHC. Data are presented as minima from maxima, and solid line in the violin plot indicates median. Two-sided p values are Levene’s test for homogeneity of variance.
Supplementary information
Supplementary Information
Supplementary Methods Tables 1 and 2.
Supplementary Data 1
CONSORT checklist.
Supplementary Data 1
Clinical trial protocol.
Source data
Source Data Fig. 3
Statistical Source Data.
Source Data Fig. 3
Representative images of CT scans, MRIs and pathology evaluation of patients on trial before and after treatment.
Source Data Fig. 4
Statistical Source Data.
Source Data Fig. 4
Representative images of CT scans, MRIs and pathology evaluation of patients on trial before and after treatment.
Source Data Fig. 5
Statistical Source Data.
Source Data Fig. 5
Representative images of CT scans, MRIs and pathology evaluation of patients on trial before and after treatment.
Source Data Fig. 6
Statistical Source Data.
Source Data Fig. 6
Representative images of CT scans, MRIs and pathology evaluation of patients on trial before and after treatment.
Source Data Extended Data Fig. 1
Statistical Source Data.
Source Data Extended Data Fig. 2
Statistical Source Data.
Source Data Extended Data Fig. 3
Statistical Source Data.
Source Data Extended Data Fig. 4
Statistical Source Data.
Source Data Extended Data Fig. 5
Statistical Source Data.
Source Data Extended Data Fig. 5
Representative images of CT scans, MRIs and pathology evaluation of patients on trial before and after treatment.
Source Data Extended Data Fig. 6
Statistical Source Data.
Source Data Extended Data Fig. 7
Statistical Source Data.
Source Data Extended Data Fig. 8
Statistical Source Data.
Source Data Extended Data Fig. 9
Statistical Source Data.
Source Data Extended Data Table 1
Statistical Source Data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roland, C.L., Nassif Haddad, E.F., Keung, E.Z. et al. A randomized, non-comparative phase 2 study of neoadjuvant immune-checkpoint blockade in retroperitoneal dedifferentiated liposarcoma and extremity/truncal undifferentiated pleomorphic sarcoma. Nat Cancer 5, 625–641 (2024). https://doi.org/10.1038/s43018-024-00726-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-024-00726-z