Abstract
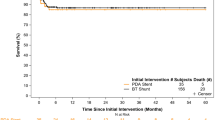
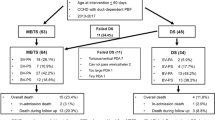
Surgical aortopulmonary shunting (SAPS) and ductal stenting (DS) are the main palliations in infants with cyanotic congenital heart diseases (CHD). We aimed to study the safety and efficacy of DS and to compare it with SAPS as a palliative procedure in infants with CHD and duct-dependent pulmonary circulation. Retrospective institutional clinical data review of consecutive infants aged < 3 months who underwent DS or SAPS over 5 years. The primary outcome was procedural success which was defined as event-free survival (mortality, need for re-intervention, procedural failure) at 30 days post-procedure. The secondary outcome was defined by a composite of death, major adverse cardiovascular events, or need for re-intervention at 6 months and on long-term follow-up. We included 102 infants (DS, n = 53 and SAPS, n = 49). The median age at DS and SAPS was 4 days (IQR 2.0–8.5) and 8 days (IQR 4.0–39.0), respectively. The median weight at intervention was 3.0 kg (IQR 3.0–3.0) and 3.0 kg (IQR 2.5–3.0) in the two respective arms. Tetralogy of Fallot with pulmonary atresia was the most common indication for DS and SAPS. The 30-day mortality was significantly higher in SAPS group as compared with DS group (p < 0.05). However, 30-day major adverse cardiac events (MACE) rates were similar in both groups (p = 0.29). DS was associated with shorter duration of mechanical ventilation, duration of stay in the intensive care and hospital stay than with SAPS. At 6 months, there was no significant difference in terms of mortality or event-free survival. Long-term MACE-free survival was also comparable (p = 0.13). DS is an effective and safer alternative to SAPS in infants with duct-dependent pulmonary circulation, offering reduced procedure-related mortality and morbidity than SAPS. Careful study of ductal anatomy is crucial to procedural success. However, long-term outcomes are similar in both procedures.


Similar content being viewed by others
Data Availability
The first author and the corresponding author have the dataset pertaining to this manuscript. Patient identity particulars have not been disclosed.
Code Availability
Not applicable.
Abbreviations
- CHD:
-
Congenital heart diseases
- DS:
-
Ductal stenting
- ICR:
-
Intra-cardiac repair
- MACE:
-
Major adverse cardiac events
- MBTTS:
-
Modified Blalock Taussig Thomas shunt
- PGE1:
-
Prostaglandin E1
- SAPS:
-
Surgical aortopulmonary shunt
References
Gibbs JL, Rothman MT, Rees MR et al (1992) Stenting of the arterial duct: a new approach to palliation for pulmonary atresia. Br Heart J 67:240–245. https://doi.org/10.1136/hrt.67.3.240
Garg G, Mittal DK (2018) Stenting of patent ductus arteriosus in low birth weight newborns less than 2 kg-procedural safety, feasibility and results in a retrospective study. Indian Heart J 70:709–712. https://doi.org/10.1016/j.ihj.2018.01.027
Aggarwal V, Petit CJ, Glatz AC et al (2019) Stenting of the ductus arteriosus for ductal-dependent pulmonary blood flow—current techniques and procedural considerations. Congenit Heart Dis 14:110–115. https://doi.org/10.1111/chd.12709
Alwi M, Choo KK, Latiff HA et al (2004) Initial results and medium-term follow-up of stent implantation of patent ductus arteriosus in duct-dependent pulmonary circulation. J Am Coll Cardiol 44:438–445. https://doi.org/10.1016/j.jacc.2004.03.066
Mahesh K, Kannan BRJ, Vaidyanathan B et al (2005) Stenting the patent arterial duct to increase pulmonary blood flow. Indian Heart J 57:704–708
Sagar P, Sivakumar K, Umamaheshwar KL et al (2021) Are early palliative procedures providing an adequate long-term benefit in young cyanotic infants from developing countries, despite advances in surgery and interventions? Cardiol Young 31:358–370. https://doi.org/10.1017/S1047951120003947
Bentham JR, Zava NK, Harrison WJ et al (2018) Duct stenting versus modified Blalock-Taussig shunt in neonates with duct-dependent pulmonary blood flow. Circulation 137:581–588. https://doi.org/10.1161/CIRCULATIONAHA.117.028972
Ratnayaka K, Nageotte SJ, Moore JW et al (2021) Patent ductus arteriosus stenting for all ductal-dependent cyanotic infants. Circ Cardiovasc Interv 14:e009520. https://doi.org/10.1161/CIRCINTERVENTIONS.120.009520
Haddad RN, Hanna N, Charbel R et al (2019) Ductal stenting to improve pulmonary blood flow in pulmonary atresia with intact ventricular septum and critical pulmonary stenosis after balloon valvuloplasty. Cardiol Young 29:492–498. https://doi.org/10.1017/S1047951119000118
Alsoufi B, Gillespie S, Mori M et al (2016) Factors affecting death and progression towards next stage following modified Blalock-Taussig shunt in neonates. Eur J Cardiothorac Surg 50:169–177. https://doi.org/10.1093/ejcts/ezw017
Bauser-Heaton H, Qureshi AM, Goldstein BH et al (2022) Comparison of patent ductus arteriosus stent and Blalock-Taussig shunt as palliation for neonates with sole source ductal-dependent pulmonary blood flow: results from the congenital catheterization research collaborative. Pediatr Cardiol 43:121–131. https://doi.org/10.1007/s00246-021-02699-7
Ghaderian M, Behdad S, Mokhtari M, Salamati L (2023) Comparison of patent ductus arteriosus stenting and Blalock-Taussig shunt in ductal dependent blood flow congenital heart disease and decreased pulmonary blood flow. Heart Views 24:11–16. https://doi.org/10.4103/heartviews.heartviews_84_22
Tseng SY, Truong VT, Peck D et al (2022) Patent ductus arteriosus stent versus surgical aortopulmonary shunt for initial palliation of cyanotic congenital heart disease with ductal-dependent pulmonary blood flow: a systematic review and meta-analysis. J Am Heart Assoc 11:e024721. https://doi.org/10.1161/JAHA.121.024721
Alsagheir A, Koziarz A, Makhdoum A et al (2021) Duct stenting versus modified Blalock-Taussig shunt in neonates and infants with duct-dependent pulmonary blood flow: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 161:379-390.e8. https://doi.org/10.1016/j.jtcvs.2020.06.008
Boucek DM, Qureshi AM, Goldstein BH et al (2019) Blalock-Taussig shunt versus patent ductus arteriosus stent as first palliation for ductal-dependent pulmonary circulation lesions: a review of the literature. Congenit Heart Dis 14:105–109. https://doi.org/10.1111/chd.12707
Helal AM, Elmahrouk AF, Bekheet S et al (2022) Patent ductus arteriosus stenting versus modified Blalock-Taussig shunt for palliation of duct-dependent pulmonary blood flow lesions. J Card Surg 37:2571–2580. https://doi.org/10.1111/jocs.16692
Santoro G, Capozzi G, Caianiello G et al (2009) Pulmonary artery growth after palliation of congenital heart disease with duct-dependent pulmonary circulation: arterial duct stenting versus surgical shunt. J Am Coll Cardiol 54:2180–2186. https://doi.org/10.1016/j.jacc.2009.07.043
Shahanavaz S, Qureshi AM, Petit CJ et al (2021) Factors influencing reintervention following ductal artery stent implantation for ductal-dependent pulmonary blood flow: results from the congenital cardiac research collaborative. Circ Cardiovasc Interv 14:e010086. https://doi.org/10.1161/CIRCINTERVENTIONS.120.010086
Kurup HKN, Gopalakrishnan A, Sasikumar D, Krishnamoorthy KM (2023) Safety of drug-eluting stents for stenting patent arterial duct in neonates. Cardiol Young 33:437–443. https://doi.org/10.1017/S104795112200110X
Goldstein BH, O’Byrne ML, Petit CJ et al (2019) Differences in cost of care by palliation strategy for infants with ductal-dependent pulmonary blood flow. Circ Cardiovasc Interv 12:e007232. https://doi.org/10.1161/CIRCINTERVENTIONS.118.007232
Acknowledgements
Nil.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
The study was approved by the Institute Ethics Committee of Sree Chitra Tirunal Institute for Medical Sciences and Technology (IEC No. ECR/189/Inst/KL/2013) and was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its amendments.
Consent to Participate
Written informed consent was obtained from all the patients in the study in English or in their vernacular for participation in the study.
Consent for Publication
Written informed consent was obtained from all the patients in the study in English or in their vernacular for publication of the study results. Patient detail privacy has been taken care of and identity particulars have not been disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, G., Gopalakrishnan, A., Subramanian, V. et al. Early and Long-Term Clinical Outcomes of Ductal Stenting Versus Surgical Aortopulmonary Shunt Among Young Infants with Duct-Dependent Pulmonary Circulation. Pediatr Cardiol 45, 787–794 (2024). https://doi.org/10.1007/s00246-024-03415-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-024-03415-x