Abstract
As outcomes from allogeneic bone marrow transplantation (BMT) have improved, prevention of long-term complications, such as fragility fractures, has gained importance. We aimed to assess areal bone mineral density (aBMD) and trabecular bone score (TBS) changes post BMT, and determine their relationship with fracture prevalence. Patients who attended the Royal Melbourne Hospital (RMH) BMT clinic between 2005–2021 were included. Patient characteristics and dual-energy X-ray absorptiometry (DXA) values were collected from the electronic medical record and a survey. TBS iNsight™ was used to calculate TBS for DXA scans performed from 2019 onwards. 337 patients with sequential DXAs were eligible for inclusion. Patients were primarily male (60%) and mean age ± SD was 45.7 ± 13.4 years. The annualised decline in aBMD was greater at the femoral neck (0.066g/cm2 (0.0038–0.17)) and total hip (0.094g/cm2 (0.013–0.19)), compared to the lumbar spine (0.049g/cm2 (− 0.0032–0.16)), p < 0.0001. TBS declined independently of aBMD T-scores at all sites. Eighteen patients (5.3%) sustained 19 fractures over 3884 person-years of follow-up post-transplant (median follow-up 11 years (8.2–15)). This 5.3% fracture prevalence over the median 11-year follow-up period is higher than what would be predicted with FRAX® estimates. Twenty-two patients (6.5%) received antiresorptive therapy, and 9 of 18 (50%) who fractured received or were on antiresorptive therapy. In BMT patients, aBMD and TBS decline rapidly and independently in the first year post BMT. However, FRAX® fracture probability estimates incorporating these values significantly underestimate fracture rates, and antiresorptive treatment rates remain relatively low.
Similar content being viewed by others
Introduction
As outcomes from allogeneic bone marrow transplantation (BMT) continue to improve, monitoring for longer-term complications becomes increasingly important. Decline in bone health post BMT is well-established [1], although the pathophysiology is multifactorial. BMT preparative chemotherapy and total body irradiation, glucocorticoids (short-term or prolonged for graft-versus-host disease (GVHD)), suboptimal nutrition and hypogonadism may all contribute [2]. Increased rates of infection due to poor graft function have been associated with reduction in areal bone mineral density (aBMD) in some studies, while other studies have associated infection with greater aBMD [3, 4].
There are limited longitudinal data in the BMT population to guide bone health assessment and timing of antiresorptive therapy. Probability of fracture is high, but currently available fracture probability calculators only have modest predictive ability in these patients and do not include BMT as a risk factor [5].
Antiresorptive therapies are efficacious to prevent bone loss post BMT, but the frequency of surveillance dual energy X-ray absorptiometry (DXA) and the trigger for treatment initiation are still to be determined [6]. Additional determinants of fracture risk in BMT have not been explored. Trabecular bone score (TBS) is a novel tool used to assess bone microarchitecture, which is a key component of bone quality that is not accounted for by DXA-derived aBMD alone. It is a grey-level textural measurement that is derived from the DXA lumbar spine image and can assess fracture risk in chronic kidney disease metabolic bone disease [7].
We aimed to assess aBMD and TBS changes post BMT and to determine their relationship with probability of fracture, in order to establish optimal timing for DXA screening and facilitate appropriate intervention with antiresorptive therapy.
Materials and Methods
We performed a retrospective cohort study of patients who underwent BMT at the Royal Melbourne Hospital (RMH) and had undergone sequential DXA scans pre and post BMT, or at least two DXA scans post BMT. Baseline, pre-BMT DXA readings were not available for some patients. In these cases, DXA scans pre-BMT were not performed or not available in the medical record. This was partly due to some transplants occurring as early as 1992, at the dawn of DXA in routine clinical practice. All patients with TBS data had a pre-BMT DXA scan available.
The cohort comprised two groups of patients; the first being all patients who attended the RMH BMT clinic from 2005–2018 and responded to an electronic or paper-based survey sent in 2022 (see Supplementary Appendix 1); the second consisted of BMT recipients who had a DXA scan performed after TBS software became available at RMH between 2019 − 2021. These two cohorts were combined to create the final patient population for analysis.
Patient characteristics including low-trauma fracture data and DXA values were collected in 2022 from the electronic medical record and surveys sent to consenting patients. TBS iNsightTM (Medimaps SA, France) was used to calculate TBS, and FRAX® and FRAX®-TBS were used to calculate probability of fracture.
Data were synthesised and analysed, and graphs created using R version 4.2.2 (R Project for Statistical Computing). The Shapiro–Wilk test was used to assess normality, with the Wilcoxon test used to analyse non-normally distributed continuous variables and the t-test for normally-distributed continuous variables. The Chi-squared test was used to analyse categorical variables and the Friedman’s test was used to analyse non-parametric dependent measures. Logistic regression was employed for multivariate analyses performed to predict the probability of fracture based on predictor variables. All models were assessed to be well-fit as per the Hosmer–Lemeshow goodness-of-fit test and there was no collinearity present between predictive variables in any of the models. Normally-distributed data were expressed as mean ± standard deviation (SD) and non-normally distributed data were expressed as median (interquartile range (IQR)).
Results
In total, 337 patients were eligible for inclusion, of whom 47 had sequential TBS available. Of the 337 patients, 245 patients (73%) had their first DXA scan completed prior to BMT. First DXA scans performed prior to BMT were performed a median (IQR) of 30 days (22–36) prior to transplant, and first DXA scans performed after BMT were performed a median (IQR) of 1.25 years (0.28–7.5) following BMT. Of the 287 patients sent a survey, 238 responded (83% response rate). Patients were followed for a median of 11 years (8.2–15) post BMT, totalling 3884 person-years of follow-up.
Patients had a mean age of 45.7 ± 13.4 years at the time of BMT, and they were primarily male (201/337, 59.6%). The median BMI was 25.8 kg/m2 (22.8–29.3). Characteristics of subjects who did or did not fracture are displayed in Table 1.
Vitamin D data were available for 244 of 337 (72%) patients. Among the 119 patients not on vitamin D supplementation, the mean (SD) 25-hydroxyvitamin D (25-OHD) level was 81nmol/L (26). Among the 125 patients on vitamin D supplementation, the median (IQR) 25-OHD level was 68nmol/L (55–87).
Admission data were available for 259 of 337 (77%) patients. The median (IQR) number of admissions was two (1–4) in the year following BMT, including the index admission for BMT. The median (IQR) number of days admitted to hospital in the year following BMT was 29 days (22–46). Of the 259 patients with admissions data, 193 had their second DXA performed in the first year post BMT. There was no correlation between days spent admitted to hospital in the first year post BMT and the annualised decline in aBMD at any site (no statistically-significant correlation using Spearman’s test).
First available DXA T-scores for aBMD were relatively preserved: median (IQR) T-score − 0.56 (− 1.40–0.48) at the lumbar spine, − 1.00 (− 1.79–0.02) at the femoral neck, and − 0.59 (− 1.39–0.39) at the total hip. Most patients had their second DXA scan performed in the first year post BMT (216/337, 64.1%). Comparing aBMD between the first and second DXA scans, there was a significant decline in bone density at all sites (Fig. 1). The percentage decline in aBMD between first and second DXA, and the median (IQR) annualised decline in aBMD was greater at the femoral neck (4.6%; 0.066g/cm2 (0.0038–0.17)) and total hip (4.7%; 0.094g/cm2 (0.013–0.19)), compared to the spine (3.2%; 0.049g/cm2 (− 0.0032–0.16)). There was greater annualised decline in aBMD within the first year post BMT comparative to follow-up DXA scans performed later in the follow-up period (see Table 2, p < 0.001 at all sites).
TBS declined significantly post BMT (Fig. 2) and independently of T-scores (no statistically-significant correlation using Spearman’s test). At baseline pre-BMT, mean TBS was 1.35 ± 0.10, while at the time of first follow-up DXA, mean TBS was 1.29 ± 0.11 (p = 0.006). While there is no established reference range for men, for postmenopausal women this would translate to a transition from normal to partially degraded microarchitecture following BMT.
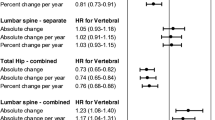
Eighteen patients (5.3%) sustained 19 fractures over 3884 person-years of follow-up post-transplant. These fractures occurred at the radius/ulna (8/19), spine (3/19), femur/hip (2/19), tibia (2/19), rib (2/19) and shoulder (2/19). The median (IQR) time to fracture post BMT was 7.4 years (2.9–12). This corresponds to a 5.3% prevalence of fractures over a median follow-up of 11 years and was significantly greater than predicted by the FRAX® fracture probability calculator even after adjustment for TBS, although glucocorticoid exposure data were limited and designated “no” if unknown. When FRAX® was adjusted for TBS, there was a non-significant increase in the 10-year estimated probability of fracture from 2.69% to 2.74% (p = 0.53) for major osteoporotic fracture, and 0.72% to 0.83% (p = 0.96) for hip fracture (Fig. 3). Females were significantly more likely to fracture than males (p = 0.036), and those who fractured were significantly older (p = 0.024). There was no difference in annualised aBMD decline between fracturing and non-fracturing groups on univariate (Table 1) or multivariate (Tables 3, 4 and 5) analyses. This lack of difference persisted even after narrowing the data to patients who had their second DXA scan in the first year post BMT only (Table 4), and when patients who received antiresorptive therapy were excluded (Table 5). There was no difference in annualised TBS decline between fracturing and non-fracturing groups.
FRAX® 10-year probability of fracture (%) with and without adjustment for TBS for major osteoporotic fracture and hip fracture (N = 47). Despite FRAX being validated for age above 40 years, the N of 47 includes two people aged 37 and 38 years-old who were included given they were close to 40 years of age
At the time of the second DXA scan (N = 337), 72 patients (21%) had osteoporosis and 156 (46%) had osteopenia. Only 109 patients (22%) had normal bone density at all sites. Twenty-two (6.5%) received antiresorptive therapy. Of the 18 patients who fractured, nine received antiresorptive treatment (mean T-score − 1.9 at the lumbar spine, − 2.0 at the femoral neck and − 1.2 at the total hip at the time of the second available DXA). Thirteen of the 319 patients who did not fracture also received antiresorptive therapy (mean T-score − 2.0 at the lumbar spine, median T-score − 2.2 at the femoral neck and − 2.0 at the total hip).
Discussion
To our knowledge, this is the first study to illustrate the bone loss, microarchitectural decay and increased fracture risk in BMT recipients over an extended follow-up period. In this group, there was rapid, significant bone loss post BMT, most pronounced in the first year following transplant, mirroring the timeline of glucocorticoid-induced osteoporosis [8]. Notably however, bone loss was greatest at the femoral neck, while glucocorticoid-induced osteoporosis predominantly affects the spine [9]. This is consistent with previous studies [3]. Decay in bone microarchitecture was also noted as evidenced by the decline in TBS post BMT. TBS decline was independent of T-score decline, as has previously been demonstrated in renal transplant recipients [10]; TBS and aBMD are therefore complementary methods for assessing bone quality.
Similar to previous studies of BMT recipients [11, 12], the femoral neck and hip sites had greater annualised bone loss than the lumbar spine. This may be partially explained by immobility-related bone loss, where demineralisation of the weight-bearing skeleton including the femur and tibia lead to reduced bone density and increased fracture risk at these sites [13, 14]. Exercise has been shown to improve function, quality of life and length of stay in BMT recipients [15]. In our study, BMT recipients were admitted for a median of one month in the year after transplant, however frequency of admission did not correlate with annualised decline in aBMD. Research into other pathophysiological mechanisms is warranted, including investigation of vitamin D status post BMT. Some studies have suggested vitamin D deficiency may be prevalent in BMT recipients [16], although this was not the case in our cohort.
This deterioration in bone health translates to an increased fracture risk. Of concern, these patients are fracturing despite relatively preserved aBMD and TBS at the time of first DXA scan. We recorded 19 fractures over 3884 person years of follow-up, which equates to a 5.3% probability of osteoporotic fracture over the median 11-year study period. Some studies have reported an even greater risk, with up to 8–10.6% of BMT recipients experiencing fragility fractures [17, 18]. This high probability of fracture in the BMT subpopulation is greater than that estimated by conventional fracture probability calculators including FRAX®, which do not include BMT as a risk factor. Glucocorticoids have been shown to increase fracture risk independent of aBMD [19], and similarly our study found fracture incidence was independent of annualised aBMD decline.
TBS is a novel and useful adjunct that can assist clinicians in predicting future fractures. FRAX®-TBS predicted a higher (although not significant) probability of fracture compared to FRAX® alone. TBS is known to improve fracture risk assessment in glucocorticoid-induced osteoporosis and, given that this is a factor in BMT recipients, further supports TBS utility in the BMT population [20].
There are few studies of TBS in BMT patients and they have contrasting findings. Pawlowska et al. [21] evaluated 137 patients to find that TBS declined significantly in women and patients treated with glucocorticoids. Conversely in 68 patients, Lim et al. [3] found no significant change in TBS from baseline to 12 months and from 12 to 24 months, although the sample size was small. Further study of TBS in the BMT population could assess its utility in guiding earlier appropriate antiresorptive treatment. Currently, there are no accepted thresholds for TBS alone to prompt antiresorptive therapy, although this may change in the future. Instead, its present utility is in augmenting fracture probability estimates, e.g. FRAX®-TBS, or qualitatively when considered in conjunction with aBMD.
Our study is limited by being a retrospective, single-centre cohort study. There were also limited glucocorticoid exposure data available, which may have contributed to an underestimate of FRAX fracture risk. The relatively younger age of individuals post BMT may have also contributed to an underestimated fracture risk, with younger BMT recipients less likely to fracture than older recipients [18]. The study is strengthened by a relatively large sample size with substantive longitudinal follow-up and the ability to assess fracture occurrence. While there were only 47 patients with sequential TBS available in our study, there are limited data on TBS in the BMT population and thus this represents a relatively sizeable population. There were a small number of patients who fractured, which may limit comparisons between the group of patients who did and did not fracture. For patients who did not respond to the survey, fracture data were collected from the medical record and this method may have missed some fractures that occurred in the community. However, this study provides a fresh perspective on fracture probability and TBS utility in this population that may be confirmed with future research endeavours.
Patients post BMT are vulnerable and experience long-term health consequences post-transplant. This includes a high risk of declining bone health and fracture, which is multifactorial. Recognising declining bone health early is paramount as it allows earlier institution of effective and well-tolerated antiresorptive therapies where appropriate. The FRAX algorithm was derived from patients older than forty years of age, and is therefore less applicable to BMT patients who are younger than other solid organ transplantation cohorts such as kidney transplant recipients [22].
Unlike solid organ transplant recipients who are often on lifelong glucocorticoids, BMT subjects are weaned off immunosuppressants. Therefore, fracture calculators underestimate absolute fracture risk because they do not register BMT recipients with additional risk factors either via prolonged high-dose glucocorticoids use or the presence of secondary osteoporosis with chronic conditions such as type 1 diabetes or chronic liver disease. An additional adjustment factoring BMT into fracture probability calculators may improve bone health assessment in the future. We propose a factor adjustment by at least 100–200% based on the 5.3% fracture prevalence in our study compared to the 2.69% FRAX estimate although this may be an underestimate due to limited glucocorticoid data. This may encourage earlier intervention with antiresorptive therapy where appropriate, thereby minimising preventable fractures.
The current recommendation post BMT is to assess aBMD using DXA at baseline and within one year post-transplant or at 3 months if there has been exposure to high-dose corticosteroids early post-transplant [6, 23]. Newer guidelines recommend antiresorptive therapy if DXA T-score < 1.5 [24]. The guidelines in solid organ recipients recommend antiresorptive therapy in those with osteopenic T-score to offset the rapid bone loss immediately post-transplantation. Our study demonstrated rapid aBMD decline in the first year post BMT independent of TBS decline, therefore we recommend a DXA scan with TBS at baseline and within one year post BMT with subsequent DXA scans guided by the clinical picture.
Akin to the current literature, prophylactic antiresorptive therapy was not administered to many patients with an indication for treatment. Eighty-four patients had clinically-defined osteoporosis, either having T-scores in the osteoporotic range or a low-trauma fracture plus osteopenic aBMD, providing an indication for antiresorptive therapy. Seventeen of these patients received antiresorptive, corresponding with a 20% treatment rate. In the BMT population, multidisciplinary collaboration and further research may improve fracture risk calculation and earlier antiresorptive therapy where appropriate.
Conclusion
In BMT patients, aBMD and TBS declined rapidly and independently during the first year post BMT; however, FRAX® fracture probability estimates incorporating these values significantly underestimate fracture rates and osteoporosis treatment rates remain low. It is recommended that patients undergo baseline DXA and follow-up DXA within 1-year post BMT, preferably incorporating TBS, to risk stratify for osteoporosis therapy. FRAX® fracture probability calculations should be considered underestimates. In the future, specific adjustments for BMT patients may enhance predictions of fracture risk and facilitate optimal use of osteoporosis therapies.
Abbreviations
- aBMD:
-
Areal bone mineral density
- BMI:
-
Body mass index
- BMT:
-
Bone marrow transplant
- DXA:
-
Dual energy X-ray absorptiometry
- GVHD:
-
Graft-versus-host disease
- 25-OHD:
-
25-hydroxyvitamin D
- IQR:
-
Interquartile range
- RMH:
-
The Royal Melbourne Hospital
- SD:
-
Standard deviation
- TBS:
-
Trabecular bone score
References
Ebeling PR, Thomas DM, Erbas B, Hopper JL, Szer J, Grigg AP (1999) Mechanisms of bone loss following allogeneic and autologous hemopoietic stem cell transplantation. J Bone Miner Res 14(3):342–350. https://doi.org/10.1359/jbmr.1999.14.3.342
Kendler DL, Body JJ, Brandi ML, Broady R, Cannata-Andia J, Cannata-Ortiz MJ, El Maghraoui A, Guglielmi G, Hadji P, Pierroz DD, de Villiers TJ (2018) Bone management in hematologic stem cell transplant recipients. Osteoporos Int 29:2597–2610
Lim Y, Baek KH, Kim HJ, Lee S, Lee JW, Kang MI (2019) Changes in trabecular bone score and bone mineral density following allogeneic hematopoietic stem cell transplantation. Bone 124:40–46. https://doi.org/10.1016/j.bone.2019.04.004
Schyrr F, Wolfer A, Pasquier J, Nicoulaz AL, Lamy O, Naveiras O (2018) Correlation study between osteoporosis and hematopoiesis in the context of adjuvant chemotherapy for breast cancer. Ann Hematol 97:309–317. https://doi.org/10.1007/s00277-017-3184-6
Pundole X, Murphy WA, Ebede CC, Karim E, Manocha S, Don-Pedro D, Rondon G, Leung CH, Liu S, Du XL, Champlin RE (2018) Fracture risk prediction using FRAX in patients following hematopoietic stem cell transplantation. Arch Osteoporos 13:1–8. https://doi.org/10.1007/s11657-018-0453-5
McClune BL, Polgreen LE, Burmeister LA, Blaes AH, Mulrooney DA, Burns LJ, Majhail NS (2011) Screening, prevention and management of osteoporosis and bone loss in adult and pediatric hematopoietic cell transplant recipients. Bone Marrow Transplant 46(1):1–9. https://doi.org/10.1038/bmt.2010.198
Aleksova J, Ebeling PR, Milat F, Elder GJ (2022) DXA-derived advanced hip analysis and the trabecular bone score in end-stage kidney disease secondary to type 1 diabetes. Eur J Endocrinol 187(6):883–892. https://doi.org/10.1530/eje-22-0687
Staa TV, Staa TV, Staa TV, Leufkens HG, Cooper C (2002) The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 13:777–787. https://doi.org/10.1007/s001980200108
Buckley L, Humphrey MB (2018) Glucocorticoid-induced osteoporosis. N Engl J Med 379(26):2547–2556. https://doi.org/10.1056/NEJMcp1800214
Naylor KL, Lix LM, Hans D, Garg AX, Rush DN, Hodsman AB, Leslie WD (2016) Trabecular bone score in kidney transplant recipients. Osteoporos Int 27:1115–1121. https://doi.org/10.1007/s00198-015-3424-3
Yao S, McCarthy PL, Dunford LM, Roy DM, Brown K, Paplham P, Syta M, Lamonica D, Smiley S, Battiwalla M, Padmanabhan S (2008) High prevalence of early-onset osteopenia/osteoporosis after allogeneic stem cell transplantation and improvement after bisphosphonate therapy. Bone Marrow Transplant 41(4):393–398. https://doi.org/10.1038/sj.bmt.1705918
Kashyap A, Kandeel F, Yamauchi D, Palmer JM, Niland JC, Molina A, Fung H, Bhatia R, Krishnan A, Nademanee A, O’Donnell MR (2000) Effects of allogeneic bone marrow transplantation on recipient bone mineral density: a prospective study. Biol Blood Marrow Transplant 6(3):344–351. https://doi.org/10.1016/s1083-8791(00)70061-9
Maimoun L, Fattal C, Micallef JP, Peruchon E, Rabischong P (2006) Bone loss in spinal cord-injured patients: from physiopathology to therapy. Spinal Cord 44(4):203–210. https://doi.org/10.1038/sj.sc.3101832
Epstein S, Inzerillo AM, Caminis J, Zaidi M (2003) Disorders associated with acute rapid and severe bone loss. J Bone Miner Res 18(12):2083–2094. https://doi.org/10.1359/jbmr.2003.18.12.2083
Abo S, Denehy L, Ritchie D, Lin KY, Edbrooke L, McDonald C, Granger CL (2021) People with hematological malignancies treated with bone marrow transplantation have improved function, quality of life, and fatigue following exercise intervention: a systematic review and meta-analysis. Phys Ther. https://doi.org/10.1093/ptj/pzab130
Sproat L, Bolwell B, Rybicki L, Dean R, Sobecks R, Pohlman B, Andresen S, Sweetenham J, Copelan E, Kalaycio M (2011) Vitamin D level after allogeneic hematopoietic stem cell transplant. Biol Blood Marrow Transplant 17(7):1079–1083. https://doi.org/10.1016/j.bbmt.2010.12.704
Stern JM, Sullivan KM, Ott SM, Seidel K, Fink JC, Longton G, Sherrard DJ (2001) Bone density loss after allogeneic hematopoietic stem cell transplantation: a prospective study. Biol Blood Marrow Transplant 7(5):257–264. https://doi.org/10.1053/bbmt.2001.v7.pm11400947
Pundole XN, Barbo AG, Lin H, Champlin RE, Lu H (2015) Increased incidence of fractures in recipients of hematopoietic stem-cell transplantation. J Clin Oncol 33(12):1364–1370. https://doi.org/10.1200/jco.2014.57.8195
Kanis JA, Johansson H, Oden A, Johnell O, De Laet C, Melton LJ III, Tenenhouse A, Reeve J, Silman AJ, Pols HA, Eisman JA (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19(6):893–899. https://doi.org/10.1359/jbmr.040134
Florez H, Hernández-Rodríguez J, Muxi A, Carrasco JL, Prieto-González S, Cid MC, Espinosa G, Gómez-Puerta JA, Monegal A, Guañabens N, Peris P (2020) Trabecular bone score improves fracture risk assessment in glucocorticoid-induced osteoporosis. Rheumatology 59(7):1574–1580. https://doi.org/10.1093/rheumatology/kez464
Pawlowska M, Yang Q, Hamata B, Kendler DL, Broady R (2016) Early changes in bone mineral density and trabecular bone score following allogeneic stem cell transplant. Bone Marrow Transplant 51(5):738–740. https://doi.org/10.1038/bmt.2015.329
Hall EC, Pfeiffer RM, Segev DL, Engels EA (2013) Cumulative incidence of cancer after solid organ transplantation. Cancer 119(12):2300–2308. https://doi.org/10.1002/cncr.28043
Bar M, Ott SM, Lewiecki EM, Sarafoglou K, Wu JY, Thompson MJ, Vaux JJ, Dean DR, Saag KG, Hashmi SK, Inamoto Y (2020) Bone health management after hematopoietic cell transplantation: an expert panel opinion from the american society for transplantation and cellular therapy. Biol Blood Marrow Transplant 26(10):1784–1802
Kendler DL, Body JJ, Brandi ML, Broady R, Cannata-Andia J, Cannata-Ortiz MJ, El Maghraoui A, Guglielmi G, Hadji P, Pierroz DD, de Villiers TJ (2021) Osteoporosis management in hematologic stem cell transplant recipients: Executive summary. J Bone Oncol 28:100361. https://doi.org/10.1016/j.jbo.2021.100361
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
JDW, DR, CJY and CC: conceived the idea for this study. All authors contributed to data acquisition. JYG: cleaned and analysed the data, and drafted the manuscript. All authors reviewed and revised the manuscript, approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JYG and CJY: are guarantors.
Corresponding author
Ethics declarations
Conflict of interest
Joanna Y. Gong, Cherie Chiang, John D. Wark, David Ritchie, Yvonne Panek-Hudson, Minh V. Le, Lydia Limbri, Nicolo Fabila, Spiros Fourlanos, Christopher J. Yates certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Human and Animal Rights and Informed Consent
This study has been approved by the Royal Melbourne Hospital Human Research Ethics Committee, an institutional ethics committee (QA2022055).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gong, J.Y., Chiang, C., Wark, J.D. et al. Bone Density and Trabecular Bone Score Decline Rapidly in the First Year After Bone Marrow Transplantation with a Marked Increase in 10-Year Fracture Risk. Calcif Tissue Int 114, 377–385 (2024). https://doi.org/10.1007/s00223-024-01189-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-024-01189-1