Abstract
A pragmatic double-blind randomized controlled trial was conducted in Barcelona to assess a telephone-based smoking cessation intervention’s effectiveness for individuals with mental health disorders post-discharge. Participants were divided into an intervention group (IG) and control group (CG) with a 2:1 allocation ratio. The IG received proactive motivational assistance, while the CG received brief advice. Biochemically validated past 7-day abstinence was the main outcome measure. Of 530 screened individuals, 294 were enrolled (200 IG, 94 CG). During follow-up, participants reported 97 episodes of ≥ 7-day abstinence (IG, 51; CG, 26). Overall abstinence probability was 30–35%, with no difference between groups at 1-year follow-up. However, intervention participants were more likely to report abstinence if they quit during hospitalization or were considering quitting. The intervention effectively supported smoking abstinence in motivated individuals. Combining this with clinical and community-based interventions holds promise for aiding smoking cessation in those with mental disorders. ClinicalTrials.gov Identifier: NCT03230955.
Similar content being viewed by others
Tobacco use is responsible for 13.5% of deaths worldwide (Reitsma et al., 2021), and although the World Health Organization (WHO) Framework Convention for Tobacco Control catapulted the progress in tobacco control (Chung-Hall et al., 2019), the prevalence of smoking among individuals with mental health disorders continues to be two to four-fold higher than in the general population (Ballbè et al., 2015; Guydish et al., 2016). The high prevalence of smoking in this group substantially impairs both their quality of life and life expectancy (Bandiera et al., 2015). Thus, smoking among individuals with mental health disorders represents an important source of health inequalities that need evidence-based solutions.
Hospitalization in smoke-free mental health centers offers a vital chance to disrupt nicotine addiction in vulnerable groups. Evidence shows that combining cognitive behavioral therapy and nicotine replacement therapy (NRT) during the stay boosts quit attempts, cuts daily cigarette use, and enhances smoking abstinence odds (Hickman et al., 2015; Metse et al., 2017). Contrary to fears that quitting smoking might worsen mental disorders or lead to relapse in other drug use, studies indicate that cessation lowers anxiety and depression, improves quality of life, and enhances success in quitting other drugs (Taylor et al., 2014; Taylor et al., 2021).
In Spain, smoking has been banned in acute psychiatric units since 2011 by a national law that has significantly impacted tobacco use in these services (Ballbe et al., 2013; Ley 42/2010). Given that three out of four hospital psychiatric inpatients are smokers (74.4%) (Ballbe et al., 2014), health professionals have frequently implemented various evidence-based interventions to mitigate nicotine withdrawal symptoms in patients hospitalized in Spanish hospitals and to promote serious quit attempts (Ballbè & Gual, 2012) such as providing pharmacotherapy and motivational and educational counseling (Taylor et al., 2021). Nevertheless, patients commonly resume smoking 2 weeks after discharge if cessation support is not provided (Bowman & Stockings, 2013; Wye et al., 2017). As such, one of the primary challenges of healthcare systems is to provide sustained cessation support in the transition between inpatient and outpatient care in an integrative and realistic way (Prochaska et al., 2017).
Among the population-level interventions to promote smoking cessation, quitlines have proven to be cost-effective (Stead et al., 2013; Taylor et al., 2014). However, quitlines are infrequently used by people with mental health disorders (Morris et al., 2009). A few randomized controlled trials (RCTs) have been conducted among this vulnerable population, but the ones that have been conducted show that counseling combined with NRT significantly increased the 7-day point prevalence abstinence rate at 6-month follow-up period and reduced the number of cigarettes consumed per day (Schwindt et al., 2017). In addition, interventions that provided a customized telephone multimodal approach obtained higher abstinence rates than telephone counseling alone (Schwindt et al., 2017). However, only a limited number of RCTs have examined strategies to enhance smoking abstinence after psychiatric hospitalization, such as referrals, and NRT upon discharge (Ortiz et al., 2013; Prochaska et al., 2004). Furthermore, only one study has evaluated a multi-component intervention that included telephone-based counseling after discharge (Brown et al., 2021).
To address this gap, we designed a telephone-based smoking cessation intervention that used the resources of an available regional quitline (called “061 CatSalut Respon”) to provide continued tobacco cessation support to people with psychiatric disorders who were discharged from smoke-free acute psychiatric units. The intervention consisted of proactively providing phone-based psychological educational support as well as pharmacological treatment advice, if required, for 12 months. The intervention was called 061 QuitMental, and its protocol has been published elsewhere (Ballbe et al., 2019).
This work aims to evaluate the effectiveness in terms of abstinence of the 061QuitMental intervention (phone-based psychological educational support over the phone with the recommendation of pharmacological treatment, when needed) compared to a control group that received brief advice over the phone among smokers with mental health disorders after discharge from adult inpatient acute psychiatric wards.
Methods
Design
This study was a multi-center pragmatic double-blind RCT with a 2:1 allocation ratio. The main reason for unequal allocation was to maximize the number of participants included in the intervention group (IG), as it was supposed to be beneficial for them. The study protocol was published elsewhere (Ballbe et al., 2019) and registered in ClinicalTrials.gov (NCT03230955). The reporting of the trial follows the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Participants
All participants had severe mental health disorders and were recruited from psychiatric wards of six acute care hospitals in the Barcelona province (Hospital Clinic i Provincial de Barcelona, Hospital de la Santa Creu i Sant Pau, Hospital Universitari Vall d’Hebron, Hospital Universitari de Bellvitge, and Hospital Hestia Duran i Reynals, Althaia Fundació) between May 2017 and December 2019.
Eligible participants were both sexes, age 18–76 years, and smokers (either daily or occasionally of any kind of tobacco products: cigarettes, roll-you-own cigarettes, e-cigarettes, waterpipes), who had stayed in an acute or detoxification mental health unit for at least 24 h, with or without motivation to quit, who had access to a telephone (landline or mobile), and resided in the province of Barcelona. Participants non-motivated to quit but who wanted to be informed about tobacco reduction and cessation were eligible to participate. We aimed to include unmotivated smokers in our study, contrary to many other studies where unmotivated smokers are often neglected. Thus, our intervention was designed to be tailored to the participant’s motivational level to increase abstinence rates and motivation to quit. Participants were excluded when they were discharged from a psychiatric emergency room, had dementia or brain damage, did not speak or read Spanish or Catalan, were pregnant, had a hearing and/or speech deficit, were already attempting to quit smoking in another center or by themselves, had voluntarily requested discharge, were transferred to another inpatient unit after discharge, or had planned to move their household outside the province of Barcelona within the following 24 months.
Study clinicians of each participating hospital approached eligible patients and invited them to participate in the RCT, the day before or the same day of discharge. Clinicians informed smokers who met the inclusion criteria about the trial by informing them regarding the 12-month pro-active intervention and the fact that they did not need to be interested in quitting to participate. Clinicians invited them to participate using an information leaflet describing the study. Informed consent was completed before discharge. Participants’ basic information was registered in a software that was used for randomization and to transfer this information to the 061 CatSalut Respon (quitline), which contacted them 48 h after discharge. All baseline information was registered into the software during the hospital stay.
Randomization and Masking
Participants who gave informed consent were randomized to the intervention group (IG) or the control group (CG) by the software (randomization seed). The study was double blinded to prevent both clinicians and participants from knowing which condition patients were assigned to. The use of software ensured that allocation was concealed, and selection bias eliminated. The same software was used to combine the data from the baseline questionnaire and from participant follow-up assessments for 12 months.
Procedures
Intervention
Participants allocated to the IG were provided a telephone-based intervention that was proactively delivered by trained nurses from the regional quitline “061 CatSalut Respon.” The intervention was based on the existing quitline protocol, which incorporated the recommendations of the Catalan Network of Smoke-free Hospitals clinical intervention guidelines for smoking cessation in patients with mental disorders (Ballbè & Gual, 2012). The intervention was customized for each participant based on their smoking status and motivational level at each call. Nurses followed a protocol algorithm to facilitate the delivery of the intervention (fully explained elsewhere (Ballbe et al., 2019)). The primary goals of the intervention were the following: (a) increase motivation to quit, (b) achieve abstinence, (c) prevent relapses if abstinence was achieved, (d) reduce consumption, and (e) increase motivation to quit smoking for those who were not yet ready to quit.
All participants in the IG received eight phone calls over a year (at 48 h, 1 week, 15 days, 1 month, 3 months, 6 months, 9 months, and 12 months post-discharge). The intervention was provided irrespective of whether the participants continued smoking or not. The first phone call at 48 h was considered the starting point of the telephone-based smoking cessation intervention and the baseline point for all data recorded after discharge. The intervention continued until the 12-month follow-up unless the participant decided to discontinue the study.
Participants assigned to the CG were contacted within the first 48 h after discharge by non-clinical phone assistants. The phone assistants provided brief cessation advice during the first call and collected data for comparison at the following endpoints: 48 h, 1 month, 6 months, and 12 months after discharge. The investigators trained the phone assistants to conduct the interviews in a neutral tone, following the wording of each question and instructed them not to give health recommendations.
Outcome Measures
The primary outcome measure for this study was biochemically validated past 7-day abstinence from any tobacco product (Hughes et al., 2003; Piper et al., 2020). Participants who were abstinent at 1, 6, and 12 months in both groups (IG and CG) were invited to go to their hospital to verify their abstinence through the detection of exhaled carbon monoxide (CO) using a PiCo Smokerlyzer. The number of total abstinence days was recorded, as well as the number of abstinence events during the 12-month follow-up period.
The main independent variable was the assignment group, either IG or CG. In addition, we assessed:
-
(i)
Sociodemographic characteristics: sex (female/male), age, educational level (no primary education, incomplete primary education, primary education, secondary education, vocational education, and university), employment situation (working, unemployed, disabled/retired, other), household situation (living accompanied or alone), and if other household members smoked (yes/no)
-
(ii)
Clinical characteristics at baseline: primary psychiatric diagnosis (e.g., bipolar, depression, substance use, schizophrenia), number of mental health disorders (one, two, three, or more), type of substance consumed (alcohol, cocaine, heroin, etc.), psychotropic medication (antidepressants, anxiolytics/hypnotics, antipsychotics, mood stabilizers, others), discharge service after hospitalization (adult mental health outpatient clinic, hospital outpatient service, treatment center for drug addiction, day-hospital, others)
-
(iii)
Tobacco use at baseline: type of consumption (daily/occasional), type of tobacco (manufactured, rolling, pipe, cigar, electronic cigarette, tobacco combined with cannabis), cigarettes per day, age of smoking initiation, Heaviness Smoking Index (HSI) as a measure of nicotine dependence self-reported (low, 0–2 points; medium, 3–4 points; high, 5–6 points) (Chabrol et al., 2005), previous quit attempts (yes/no, and number), the longest period of abstinence ever (days), use of pharmacological aid during the hospitalization (yes/no), support of a health professional to quit during hospitalization (yes/no), abstinence during hospitalization (yes/no), willingness to quit was assessed according to the Prochaska and Di Clemente Stages of Change model (precontemplation, contemplation, action, and maintenance), considering to quit (using a Likert scale 0 = not at all, 10 = completely agree), intention to reduce consumption (using a Likert scale 0 = not at all, 10 = completely agree), and self-efficacy in quitting (using a Likert scale 0 = not at all, 10 = completely agree)
Statistical Analyses
At the outset, the plan was to recruit 501 participants to detect a 15-percentage point difference between the proportion of abstinence in both groups (IG, 20% and CG, 5%) after 12 months, assuming a risk of α = 0.05 and β = 0.10 and two-sized p-value of ≤ 0.05 (Ballbè et al., 2019). We planned to conduct a sub-analysis per group, considering the randomization ratio of 2:1; we aimed to recruit at least 334 participants in the IG arm and 167 in the CG.
Descriptive analyses were summarized and stratified according to the assignment group (IG and GC) with differences between groups evaluated using a χ2 tests for categorical variables and the Mann Whitney U test for continuous variables.
We compared the abstinence rates of participants in each group at four endpoints (48 h, 1 month, 6 months, and 12 months follow-up). Analyses used an intention-to-treat approach.
The time difference between variables was assumed constant over the interval of time until the next follow-up. As multiple 7-day abstinence episodes could occur for the same participant during follow-up, these outcomes were analyzed with an extension of Cox’s regression model proposed by Andersen and Gill for multiple events (Andersen & Gill, 1982). This model assumes that the instantaneous risk of an event occurring at time t from the start of the study is independent of the predicted events (Andersen & Gill, 1982). This model has allowed us to estimate the hazards ratio (HR) of abstinence with a 95% confidence interval (CI) during the 12 months of follow-up. It was found that the effect of each variable is constant over time. The level of statistical significance was set at p < 0.05. The analyses were performed using RStudio version 4.0.3 with the survival package.
Results
Among the 530 inpatient smokers with severe mental health disorders who met the inclusion criteria (as shown in Fig. 1), 236 individuals (44.5%) declined to participate in the study. The reasons for accepting and declining have been described in detail elsewhere (Martínez et al., 2022), but as shown in Fig. 1, the most common reason was a lack of interest. As a result, 294 inpatients consented to participate in the study and were randomly assigned in a 2:1 ratio, with 200 participants in the intervention group (IG) and 94 in the control group (CG). Although the sample size was lower than expected, based on the recruited participants and the predicted difference in abstinence between groups, we obtained a power of 95.7%, which provided us with confidence in detecting differences if they existed and minimized the possibility of type II error. This power is higher than the proposed power of 90% (Myors & Murphy, 2023).
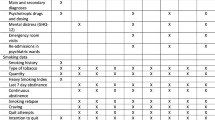
There were no differences in the sociodemographic and clinical characteristics differences between the two study groups at baseline (Table 1). The mean age of participants was 42.6 (SD = 12.5) years old, 55.2% were male, 36.7% had less than primary or primary education, and 34.3% were unemployed. Overall, 39.5% of participants had schizophrenia as their primary psychiatric disorder, 25.5% had a substance use disorder, and 44.9% had two or more psychiatric diagnostics (Table 1).
Nearly all participants were daily tobacco users (97%) with no differences in the distribution of the type of tobacco product consumed by the group (Table 2). Overall, the most frequent tobacco product used was manufactured cigarettes (53.2%), followed by roll-your-own cigarettes (16.3%) and a combination of both (8.2%). There were no differences in the number of cigarettes per day (CPD) between groups (mean CPD = 20.1, SD = 12.9). Dependence on cigarettes also did not differ by group (mean HSI = 3.16, SD = 1.75), and during hospitalization neither abstinence rates nor receiving smoking cessation pharmacological aid diverged by group. Nonetheless, participants in the IG started smoking at a younger age (16.9 years old, SD = 5.0) than those in the CG (18.5 years old, SD = 6.3) (p = 0.04) (Table 2).
From the 294 participants recruited, 11 were lost at the time of the first call post-discharge, because their number was disconnected or not in service (Fig. 1). Consequently, we followed up with 283 participants, 193 from the IG, and 90 from the CG. From them, 165 completed the follow-up surveys for all four endpoints (IG, 136; CG, 29), 59 three follow-up surveys (IG, 24; CG, 35), 34 two follow-up surveys (IG, 19; CG, 15), and 25 completed the survey only once (IG, 14; CG, 11).
All participants were intended to be followed up for 12 months. During this period, we gathered information on 930 occasions belonging to the four common endpoints in both groups. From all the records, we documented 97 episodes of ≥ 7-day abstinence (51 from the IG and 26 from the CG) that belonged to 53 participants (37 from the IG and 16 from the CG).
Figure 2 displays the estimated probability of experiencing an episode of ≥ 7-day abstinence, which was around 30 to 35%. The overall 1-year probability of having an ≥ 7-day abstinence episode did not differ significantly between the IG and the CG (HR = 1.09, CI 95% = 0.59–2.02). No differences in abstinence were found for sex, age, and psychiatric disorders groups. However, participants who were abstinent during hospital admission and those who were considering quitting within the next month at the beginning of the study had up to two- and threefold higher probability of achieving a 7-day abstinent episode during the follow-up (HR = 2.58, CI 95% = 1.47–4.53 and HR = 3.20, IC 95% = 1.65–6.21, respectively) (Table 3). When we analyzed the results per group, we observed that these two variables had a stronger and statistically significant effect on the IG (abstinence during hospitalization: HR = 3.38, 95% CI 1.85–6.17 and considering quitting in the next month: HR = 3.57, 95% CI 1.65–7.76) but not in the CG (Table 4).
Discussion
This study has demonstrated the effectiveness of a proactive, motivational telephone-based intervention delivered through an existing regional quitline. The intervention was designed to assist non-motivated smokers with mental health and drug abuse disorders who had recently been discharged from acute psychiatric hospitalization. Overall, the intervention was found to be well-received and feasible to implement. While it did not result in significantly higher rates of smoking abstinence compared to the CG, the intervention was effective in supporting abstinence among individuals who had been abstinent during hospitalization and were considering quitting at the time of recruitment.
Hospitals in Spain, including those that participated in our study in Barcelona, are required by law to be smoke-free. While smoking cessation interventions are frequently provided to hospitalized smokers, it is not mandatory, and in some cases, stabilized patients are permitted to leave the hospital, with the understanding that they may resume their tobacco use. The 061 QuitMental intervention was aimed at sustaining the benefits of being in a smoke-free environment and receiving any kind of tobacco cessation support, post-discharge, for smoking patients with severe mental health disorders that were admitted to acute psychiatric units. The intervention, which was envisioned as a strategy to provide support to maintain abstinence after discharge from psychiatric units, demonstrated that it could be introduced in the healthcare system due to its pragmatic nature. However, the non-inclusion of other components demonstrated to support smoking cessation, such as providing pharmacological aid or support through phone calls with intensive in-person visits, may have affected the effectiveness of the approach proposed.
People with severe psychiatric disorders require more intensive counseling and longer follow-up support to achieve smoking cessation (Schroeder, 2012) compared to the general population. Therefore, multiple strategies and longer periods of support are necessary to assist this population in the process of change toward cessation. Previous studies have demonstrated that tobacco quitlines are an available and feasible resource for reducing barriers in supporting smokers with mental and addiction problems (Carpenter et al., 2019; McClure et al., 2019). Although many callers to the general population national/regional quitlines report having mental disorders (Tedeschi et al., 2016), their percentage of successful quitting is up to 10 percentage points lower compared to callers without mental health conditions (Hart et al., n.d.; Schwindt et al., 2017; Tedeschi et al., 2016). Therefore, developing strategies that promote free access to quitlines, a higher number of calls, access to NRT, and support to make a quit attempt have been some of the approaches tested in this population (Parks & Kim, 2018). These tailored strategies have shown positive impacts such as an increase in smoking cessation rates and a reduction in CPD (Hart et al., n.d.; Schwindt et al., 2017; Vickerman et al., 2015), especially if they combine multiple strategies (Brown et al., 2021; Rigotti et al., 2022). Nonetheless, the interventions previously tested were addressed to motivated smokers or patients who were already abstinent, and only in one case were offered to smokers after discharge (Brown et al., 2021; Rigotti et al., 2022).
To our knowledge, the 061 QuitMental trial is the first study to provide an innovative approach to maintaining behavioral positive changes that began while being in an environment that supports quitting, in this case being admitted to a smoke-free psychiatric unit. The intervention included unique smoking cessation approaches that were previously taught to expert nurses in charge of the regional quitline. These nurses followed a protocol of eight proactive calls for 12 months (plus all the calls that each participant wanted to do on their own command), in which they provided the IG psychological and psychoeducational support, and NRT advice (if required) (Ballbe et al., 2019). The intervention followed a pragmatic approach. As NRT is not provided free of charge in the Spanish Health System, we tested our intervention without providing pharmacological treatment to participants. Although this may be seen as a weakness in the intervention, a recent study conducted among smokers motivated to quit that contacted quitline services in the USA showed that even after providing more robust therapeutical options (multiple calls vs individual services, non-NRT versus NRT, etc.), this approach does not always entail better quit rate results among this population (Hart et al., n.d.). Hart et al. suggest that people with mental health diagnoses may need several other therapeutical supports beyond the standard coaching and NRT (Hart et al., n.d.), and they suggest including other collaborative solutions such as digital-based quit tools—from online social communities to text message-based programs (Hart et al., n.d.).
The 061 QuitMental intervention was effective among smokers allocated to the IG who were abstinent during hospitalization and were thinking about quitting in the next 30 days at the time of recruitment. Healthcare systems should adopt this model to maintain and even trigger the quitting process of smokers with severe mental health conditions that have been admitted in a favorable setting for abstinence such as a smoke-free psychiatric ward (Martinez et al., 2015). With the current trend among mental health substance abuse hospitals and residential treatment programs to maintain smoke-free policy, indoors (Carpenter et al., 2019) and even outdoors (Campbell et al., 2022; Guydish et al., 2020), smoking cessation follow-up plans should be coordinated after discharge. In many cases, admission into a smoke-free hospital can provide a unique opportunity of abstinence to initiate a long-term change to reduce morbidity and mortality by quitting smoking (Parks & Kim, 2018). According to a systematic review and meta-analysis, behavioral and pharmacological support is effective in maintaining smoking abstinence following a stay in a smoke-free institution (Shoesmith et al., 2021). This continuity in the provision of smoking cessation support after discharge allows smokers, and especially those with a mental and substance use disorder, to tap into continuous support (Shoesmith et al., 2021). Thus, interventions that foster the gains obtained during hospitalization should be incorporated into routine care with the additional support of clinicians from outdoor services.
Although in this study the combination of providing discharge support of the main providers plus the tailored strategies tested through a proactive quitline service has not been tested, we believe it could be easily incorporated into the standard care delivery model in our context. Probably, as suggested by other studies, a holistic approach should be introduced in the health systems in which wider social support that involves mental health providers, smoking cessation specialists, together with peers and family members could increase smoking cessation quit attempts among these stigmatized population (Kagabo et al., 2020; Prochaska et al., 2017; Shoesmith et al., 2021). People with mental health and substance use disorders frequently face several social barriers to quitting smoking including living in a pro-smoking social environment or having low support from their network (including health providers, family members, peers, etc.) that interfere in the process of quitting (Aschbrenner et al., 2019). So, a more holistic approach that promotes a more supportive environment should be incorporated in future studies.
Our findings highlight the need to strengthen tobacco cessation services offered in psychiatric units to promote abstinence during and after hospitalization. It is also worth mentioning that the lack of effectiveness of the intervention may be due to the lack of retention in the study that affected both groups. Among 80% of smokers in the IG and 74% in the CG who were enrolled in the study and who accepted to participate in the follow-ups, only 39% and 28% completed the 6-month follow-up survey. These results are similar to the ones obtained in a study in which the effectiveness of a quitline addressed to the general population was evaluated, in which only 40% of smokers participated in the 7-month follow-up survey (meaning that 60% of participants dropped out or were not found at 7-month follow-up) (Nair et al., 2020). This underlines retention as a challenge in the provision of supportive strategies addressed to mentally ill smoker’s post-discharge. And, although proactive outreach is a promising approach to increasing access to tobacco cessation treatment (Rogers et al., 2016), attrition remains challenging in this population (Metse et al., 2018; Prochaska et al., 2017). Japuntich et al. found that participants in a RCT in which proactive outreach was addressed to veterans with mental health problems, participants in the IG were more likely to engage in telephone counseling (IG, 22% vs CG, 3%) and NRT (IG, 51% vs CG, 41%) than those in the CG, but the adherence to the intervention was limited (Japuntich et al., 2020).
Study Limitations
The main limitation of this study was the introduction of selection bias. Smokers who showed a strong desire to quit that were admitted in these hospitals were referred to an intensive smoking cessation program (Martínez et al., 2022), and thus, those patients were excluded from the present study. Therefore, the participants in this trial comprised unmotivated smokers and probably more reluctant to quit smoking and commit to the recommendations provided on the phone. This however could be considered an asset of our results. Moreover, as the intervention was offered from convenience hospitals, we could also have certain selection bias. However, the participating hospitals showed a high level of variability in tobacco control policy implementation, as we have reported elsewhere (Martínez et al., 2022). Furthermore, we included a variability of smokers with several conditions, although results have shown no differences in cessation rates by psychiatric diagnostic. Additionally, it is worth mentioning that the study primarily used a 7-day abstinence measure, common in mental health and substance abuse research, to evaluate smoking cessation. This method, while useful for comparability across studies and practical in populations with high relapse rates, has limitations. It fails to fully capture the goal of sustained smoking cessation, potentially overestimating long-term abstinence as it only considers the last 7 days and ignores any smoking outside this window. To address this, the study also monitored participants’ smoking behavior over a 12-month period, observing repeated point prevalence as an outcome (Piper et al., 2020). Additionally, abstinence was biochemically validated using carbon monoxide measurements, conducted 48–72 h after phone confirmation, to ensure accuracy and mitigate the risk of residual high CO levels affecting the results.
Finally, another limitation derived from the long-term telephone follow-up is a loss to follow-up. Although we have had losses in the study, these are comparable with previous studies in the field (Nair et al., 2020).
Conclusions
This study found that non-motivated smokers with severe mental health disorders who were discharged from acute smoke-free psychiatric units had abstained from smoking during hospitalization, and considered quitting smoking had a higher likelihood of successfully quitting with the help of a proactive regional quitline that incorporated a specific protocol to assist this particularly vulnerable group. The study demonstrated the acceptability and feasibility of this intervention and showed that tailored quitlines could be a community-level solution to promote the benefits of smoking abstinence introduced during hospitalization. Future studies should investigate whether quitlines can increase quit rates when combined with other clinical and community strategies that introduce a more supportive social environment.
Data Availability
Data is available under request.
References
Andersen, P. K., & Gill, R. D. (1982). Cox’s regression model for counting processes: A large sample study. The Annals of Statistics, 10(4), 1100–1120. https://doi.org/10.1214/aos/1176345976
Aschbrenner, K. A., Naslund, J. A., Gill, L., Hughes, T., O’Malley, A. J., Bartels, S. J., & Brunette, M. F. (2019). Qualitative analysis of social network influences on quitting smoking among individuals with serious mental illness. Journal of Mental Health, 28(5), 475–481. https://doi.org/10.1080/09638237.2017.1340600
Ballbe, M., Sureda, X., Martinez-Sanchez, J. M., Salto, E., Gual, A., & Fernandez, E. (2013). Second-hand smoke in mental healthcare settings: Time to implement total smoke-free bans? International Journal of Epidemiology, 42(3), 886–893. https://doi.org/10.1093/ije/dyt014
Ballbe, M., Martinez, C., Feliu, A., Torres, N., Nieva, G., Pinet, C., Raich, A., Mondon, S., Barrio, P., Hernandez-Ribas, R., Vicens, J., Costa, S., Vilaplana, J., Alaustre, L., Vilalta, E., Blanch, R., Subira, S., Bruguera, E., Suelves, J. M., & Fernandez, E. (2019). Effectiveness of a telephone-based intervention for smoking cessation in patients with severe mental disorders: Study protocol for a randomized controlled trial. Trials, 20(1), 38. https://doi.org/10.1186/s13063-018-3106-5
Ballbè, M., Sureda, X., Martínez-Sánchez, J. M., Fu, M., Saltó, E., Gual, A., & Fernández, E. (2015). Secondhand smoke in psychiatric units: Patient and staff misperceptions. Tobacco Control, 24(e3), e212–e220. https://doi.org/10.1136/tobaccocontrol-2014-051585
Ballbe, M., Sureda, X., Martinez-Sanchez, J. M., Fu, M., Salto, E., Gual, A., & Fernandez, E. (2014). Secondhand smoke in psychiatric units: Patient and staff misperceptions. Tobacco Control. tobaccocontrol-2014–051585 [pii].
Ballbè, M., Martínez, C., Feliu, A., Torres, N., Nieva, G., Pinet, C., Raich, A., Mondon, S., Barrio, P., Hernández-Ribas, R., Vicens, J., Costa, S., Vilaplana, J., Alaustre, L., Vilalta, E., Blanch, R., Subirà, S., Bruguera, E., Suelves, J. M., & Fernández, E. (2019). Effectiveness of a telephone-based intervention for smoking cessation in patients with severe mental disorders: Study protocol for a randomized controlled trial. Trials, 20(1). https://doi.org/10.1186/s13063-018-3106-5
Ballbè, M., & Gual, A. (2012). Guia d’intervenció clínica en el consum de tabac en pacients amb trastorn mental. Barcelona: Xarxa Catalana d’Hospitals sense Fum, Institut Català d’Oncologia, Departament de Salut de la Generalitat de Catalunya.
Bandiera, F. C., Anteneh, B., Le, T., Delucchi, K., & Guydish, J. (2015). Tobacco-related mortality among persons with mental health and substance abuse problems. PLoS ONE, 10(3), e0120581. https://doi.org/10.1371/journal.pone.0120581
Bowman, J., & Stockings, E. A. (2013). Smoking cessation for hospitalised patients: Intensive behavioural counselling started in hospital and continued after discharge increases quit rates; with additional benefit from adding nicotine replacement therapy. Evidence-Based Nursing, 16(1), 21–22. https://doi.org/10.1136/eb-2012-100890;10.1136/eb-2012-100890
Brown, R. A., Minami, H., Hecht, J., Kahler, C. W., Price, L. H., Kjome, K. L., Bloom, E. L., Levy, D. E., Carpenter, K. M., Smith, A., Smits, J. A. J., & Rigotti, N. A. (2021). Sustained care smoking cessation intervention for individuals hospitalized for psychiatric disorders: The Helping HAND 3 randomized clinical trial. JAMA Psychiatry. https://doi.org/10.1001/jamapsychiatry.2021.0707
Campbell, B. K., Le, T., McCuistian, C., Hosakote, S., Kapiteni, K., & Guydish, J. (2022). Implementing tobacco-free policy in residential substance use disorders treatment: Practice changes among staff. Drug and Alcohol Dependence Reports, 2(February), 100033. https://doi.org/10.1016/j.dadr.2022.100033
Carpenter, K. M., Nash, C. M., Vargas-Belcher, R. A., Vickerman, K. A., & Haufle, V. (2019). Feasibility and early outcomes of a tailored quitline protocol for smokers with mental health conditions. Nicotine and Tobacco Research, 21(5), 584–591. https://doi.org/10.1093/ntr/ntz023
Chabrol, H., Niezborala, M., Chastan, E., & de Leon, J. (2005). Comparison of the heavy smoking index and of the Fagerstrom test for nicotine dependence in a sample of 749 cigarette smokers. Addictive Behaviors, 30(7), 1474–1477. S0306–4603(05)00031–6 [pii].
Chung-Hall, J., Craig, L., Gravely, S., Sansone, N., & Fong, G. T. (2019). Impact of the WHO FCTC over the first decade: A global evidence review prepared for the impact assessment expert group. Tobacco Control, 28, S119–S128. https://doi.org/10.1136/tobaccocontrol-2018-054389
Guydish, J., Passalacqua, E., Pagano, A., Martinez, C., Le, T., Chun, J., Tajima, B., Docto, L., Garina, D., & Delucchi, K. (2016). An international systematic review of smoking prevalence in addiction treatment. Addiction, 111(2), 220–230. https://doi.org/10.1111/add.13099. (Abingdon, England).
Guydish, J., Wahleithner, J., Williams, D., & Yip, D. (2020). Tobacco-free grounds implementation in California residential substance use disorder (SUD) treatment programs. Journal of Addictive Diseases, 38(1), 55–63. https://doi.org/10.1080/10550887.2020.1713687
Hart, J. T., Boeckman, L. M., & Beebe, L. A. (n.d.). Unique cessation tools in the box : Quitline utilization and e ectiveness trends among a large sample of tobacco users reporting mental health disorders.
Hickman, N. J., III., Delucchi, K. L., & Prochaska, J. J. (2015). Treating tobacco dependence at the intersection of diversity, poverty, and mental illness: A randomized feasibility and replication trial. Nicotine & Tobacco Research, 17(8), 1012–1021. https://doi.org/10.1093/ntr/ntv034
Hughes, J. R., Keely, J. P., Niaura, R. S., Ossip-Klein, D. J., Richmond, R. L., & Swan, G. E. (2003). Measures of abstinence in clinical trials: Issues and recommendations. Nicotine & Tobacco Research : Official Journal of the Society for Research on Nicotine and Tobacco, 5(1), 13–25.
Japuntich, S. J., Hammett, P. J., Rogers, E. S., Fu, S., Burgess, D. J., Shahawy, O. E. L., Melzer, A. C., Noorbaloochi, S., Krebs, P., & Sherman, S. E. (2020). Effectiveness of proactive tobacco cessation treatment outreach among smokers with serious mental illness. Nicotine and Tobacco Research, 22(9), 1433–1438. https://doi.org/10.1093/ntr/ntaa013
Kagabo, R., Gordon, A. J., & Okuyemi, K. (2020). Smoking cessation in inpatient psychiatry treatment facilities: A review. Addictive Behaviors Reports, 11(January), 100255. https://doi.org/10.1016/j.abrep.2020.100255
Ley 42/2010 de 26 de diciembre, de medidas sanitarias frente al tabaquismo y reguladora de la venta, el suministro, el consumo y la publicidad de los productos del tabaco. BOE número 318 de 31/12/2010, páginas 109188 a 109194B., por la que se modifica la L. 28/2005. No Title. http://www.boe.es/boe/dias/2010/12/31/pdfs/BOE-A-2010-20138.pdf
Martinez, C., Guydish, J., Le, T., Tajima, B., & Passalacqua, E. (2015). Predictors of quit attempts among smokers enrolled in substance abuse treatment. Addictive Behaviors, 40, 1–6. https://doi.org/10.1016/j.addbeh.2014.08.005
Martínez, C., Feliu, A., Torres, N., Nieva, G., Pinet, C., Raich, A., Mondon, S., Barrio, P., Andreu, M., Hernández-Ribas, R., Vicens, J., Costa, S., Suelves, J. M., Vilaplana, J., Enríquez, M., Alaustre, L., Vilalta, E., Subirà, S., Bruguera, E., & Ballbè, M. (2022). Acceptability and participation predictors for a pragmatic randomized controlled trial to test a smoking cessation intervention after discharge from mental health wards. Drug and Alcohol Dependence, 234(February), 1–6. https://doi.org/10.1016/j.drugalcdep.2022.109390
McClure, E., Tomko, R., Salazar, C., Akbar, S., Squeglia, L., Herrmann, E., Carpenter, M., & Peters, E. (2019). Tobacco and cannabis co-use: Drug substitution, quit interest, and cessation preferences. Experimental and Clinical Psychopharmacology, 27(3), 265–275. https://doi.org/10.1037/PHA0000244
Metse, A. P., Wiggers, J., Wye, P., Wolfenden, L., Freund, M., Clancy, R., Stockings, E., Terry, M., Allan, J., Colyvas, K., Prochaska, J. J., & Bowman, J. A. (2017). Efficacy of a universal smoking cessation intervention initiated in inpatient psychiatry and continued post-discharge: A randomised controlled trial. The Australian and New Zealand Journal of Psychiatry, 51(4), 366–381. https://doi.org/10.1177/0004867417692424
Metse, A. P., Hizam, N. A. N., Wiggers, J., Wye, P., & Bowman, J. A. (2018). Factors associated with retention in a smoking cessation trial for persons with a mental illness: A descriptive study. BMC Medical Research Methodology, 18(1), 1–8. https://doi.org/10.1186/s12874-018-0640-5
Morris, C. D., Tedeschi, G. J., Waxmonsky, J. A., May, M., & Giese, A. A. (2009). Tobacco quitlines and persons with mental illnesses: Perspective, practice, and direction. Journal of the American Psychiatric Nurses Association, 15(1), 32–40. https://doi.org/10.1177/1078390308330050
Myors, B., & Murphy, K. R. (2023). Statistical power analysis : A simple and general model for traditional and modern hypothesis tests (5th Editio). Routledge. https://doi.org/10.4324/9781003296225
Nair, U. S., Rabe, B., Brady, B. R., & Bell, M. L. (2020). Predictors of client retention in a state-based tobacco quitline. 67–75. https://doi.org/10.1017/jsc.2020.10
Ortiz, G., Schacht, L., & Lane, G. M. (2013). Smoking cessation care in state-operated or state-supported psychiatric hospitals: From policy to practice. Psychiatric Services, 64(7), 666–671. https://doi.org/10.1176/appi.ps.201200290
Parks, M. J., & Kim, S. (2018). Interpersonal communication in response to an intervention and its impact on smoking cessation within a low-income population. Health Education and Behavior, 45(4), 550–558. https://doi.org/10.1177/1090198117749258
Piper, M. E., Bullen, C., Krishnan-Sarin, S., Rigotti, N. A., Steinberg, M. L., Streck, J. M., & Joseph, A. M. (2020). Defining and measuring abstinence in clinical trials of smoking cessation interventions: An updated review. In Nicotine and Tobacco Research, 22(7):1098–1106. Oxford University Press. https://doi.org/10.1093/ntr/ntz110
Prochaska, J. J., Gill, P., & Hall, S. M. (2004). Treatment of tobacco use in an inpatient psychiatric setting. Psychiatric Services, 55(11), 1265–1270. https://doi.org/10.1176/appi.ps.55.11.1265. (Washington, D.C.).
Prochaska, J. J., Das, S., & Young-Wolff, K. C. (2017). Smoking, mental illness, and public health. Annual Review of Public Health, 38, 165–185. https://doi.org/10.1146/annurev-publhealth-031816-044618
Reitsma, M. B., Kendrick, P. J., Ababneh, E., Abbafati, C., Abbasi-Kangevari, M., Abdoli, A., Abedi, A., Abhilash, E. S., Abila, D. B., Aboyans, V., Abu-Rmeileh, N. M., Adebayo, O. M., Advani, S. M., Aghaali, M., Ahinkorah, B. O., Ahmad, S., Ahmadi, K., Ahmed, H., Aji, B., & Zuniga, Y. H. (2021). Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. The Lancet, 397(10292), 2337–2360. https://doi.org/10.1016/S0140-6736(21)01169-7
Rigotti, N. A., Kruse, G. R., Livingstone-Banks, J., & Hartmann-Boyce, J. (2022). Treatment of tobacco smoking: A review. JAMA - Journal of the American Medical Association, 327(6), 566–577. https://doi.org/10.1001/jama.2022.0395
Rogers, E. S., Smelson, D. A., Gillespie, C. C., Elbel, B., Poole, S., Hagedorn, H. J., Kalman, D., Krebs, P., Fang, Y., Wang, B., & Sherman, S. E. (2016). Telephone smoking-cessation counseling for smokers in mental health clinics: A patient-randomized controlled trial. American Journal of Preventive Medicine, 50(4), 518–527. https://doi.org/10.1016/j.amepre.2015.10.004
Schroeder, S. A. (2012). Smoking among hospitalized patients: Another opportunity to improve patients’ health. Archives of Internal Medicine, 172(21), 1675–1676. 1389240 [pii].
Schwindt, R., Hudmon, K. S., Knisely, M., Davis, L., & Pike, C. (2017). Impact of tobacco quitlines on smoking cessation in persons with mental illness: A systematic review. Journal of Drug Education, 47(1–2), 68–81. https://doi.org/10.1177/0047237918762104
Shoesmith, E., Huddlestone, L., Lorencatto, F., Shahab, L., Gilbody, S., & Ratschen, E. (2021). Supporting smoking cessation and preventing relapse following a stay in a smoke-free setting: A meta-analysis and investigation of effective behaviour change techniques. Addiction. https://doi.org/10.1111/add.15452
Stead, L. F., Hartmann-Boyce, J., Perera, R., & Lancaster, T. (2013). Telephone counselling for smoking cessation. The Cochrane Database of Systematic Reviews, 8, CD002850. https://doi.org/10.1002/14651858.CD002850.pub3
Taylor, G., McNeill, A., Girling, A., Farley, A., Lindson-Hawley, N., & Aveyard, P. (2014). Change in mental health after smoking cessation: Systematic review and meta-analysis. BMJ (Clinical Research Ed.), 348, g1151. https://doi.org/10.1136/bmj.g1151
Taylor, G. M. J., Lindson, N., Farley, A., Leinberger-Jabari, A., Sawyer, K., te Water Naudé, R., Theodoulou, A., King, N., Burke, C., & Aveyard, P. (2021). Smoking cessation for improving mental health. Cochrane Database of Systematic Reviews, 2021(3). https://doi.org/10.1002/14651858.CD013522.pub2
Tedeschi, G. J., Cummins, S. E., Anderson, C. M., Anthenelli, R. M., Zhuang, Y. L., & Zhu, S. H. (2016). Smokers with self-reported mental health conditions: A case for screening in the context of tobacco cessation services. PLoS ONE, 11(7), 1–12. https://doi.org/10.1371/journal.pone.0159127
Vickerman, K. A., Schauer, G. L., Malarcher, A. M., Zhang, L., Mowery, P., & Nash, C. M. (2015). Quitline use and outcomes among callers with and without mental health conditions: A 7-month follow-up evaluation in three states. BioMed Research International, 2015, 817298. https://doi.org/10.1155/2015/817298
Wye, P. M., Stockings, E. A., Bowman, J. A., Oldmeadow, C., & Wiggers, J. H. (2017). Effectiveness of a clinical practice change intervention in increasing the provision of nicotine dependence treatment in inpatient psychiatric facilities: An implementation trial. BMC Psychiatry, 17(1), 1–12. https://doi.org/10.1186/s12888-017-1220-7
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This project has been financed by the Instituto Carlos III (ISCIII) (Grant: PI15/00875) Fondo Europeo de Desarrollo Regional (FEDER) “Una manera de hacer Europa. The Tobacco Control Research Group is partly supported by the Ministry of Universities and Research from the Government of Catalonia [2017SGR319] and by Instituto de Salud Carlos III, Government of Spain (CIBERES CB19/06/00004). EF was also supported by the Instituto de Salud Carlos III, Government of Spain, co-funded by the European Regional Development Fund (FEDER) [INT16/00211 and INT17/00103]. CM was also supported by the Instituto de Salud Carlos III, Government of Spain, co-funded by the European Regional Development Fund (FEDER) [INT17/00116] and Ministry of Health from the Government of Catalonia [PERIS No 9015-586920/2017]. We thank CERCA Programme/Generalitat de Catalunya for institutional support.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Esteve Fernández and Montse Ballbè are both senior authors.
Highlights
• A telephone-based proactive motivational smoking cessation intervention was effective for individuals with mental health disorders who were abstinent during hospitalization and had considered quitting at the recruitment stage.
• Practical interventions should be designed for individuals with mental health disorders who are discharged from smoke-free hospitals to support abstinence.
• Combining telephone-based interventions with clinical and community-based interventions that foster social support could be a promising approach for smoking cessation among this vulnerable population.
• Additional research is required to identify effective strategies for promoting smoking cessation among individuals with mental health disorders who have lower levels of motivation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martínez, C., Feliu, A., Saura, J. et al. Effectiveness of a Post-discharge Phone-Based Smoking Cessation Intervention for Patients with Severe Mental Health Disorders: The 061 Quitmental Randomized Controlled Clinical Trial. Int J Ment Health Addiction (2024). https://doi.org/10.1007/s11469-024-01254-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-024-01254-8