Abstract
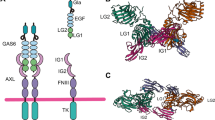
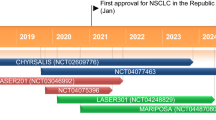
Lenvatinib is a multitargeted tyrosine kinase inhibitor capable of promoting apoptosis, suppressing angiogenesis, inhibiting tumor cell proliferation, and modulating the immune response. In multiple cancer types, lenvatinib has presented manageable safety and is currently approved as an effective first-line therapy. However, with the gradual increase in lenvatinib application, the inevitable progression of resistance to lenvatinib is becoming more prevalent. A series of recent researches have reported the mechanisms underlying the development of lenvatinib resistance in tumor therapy, which are related to the regulation of cell death or proliferation, histological transformation, metabolism, transport processes, and epigenetics. In this review, we aim to outline recent discoveries achieved in terms of the mechanisms and potential predictive biomarkers of lenvatinib resistance as well as to summarize untapped approaches available for improving the therapeutic efficacy of lenvatinib in patients with various types of cancers.
Graphical Abstract
This review focuses on current researches on the resistance mechanisms of lenvatinib, describes a series of potential biomarkers, outlines the current application status, and prospects of drugs used in combination with lenvatinib and summarizes ongoing clinical trials involving lenvatinib combination therapy.





Similar content being viewed by others
Data availability
Not applicable.
Abbreviations
- RTKs:
-
Receptor tyrosine kinases
- TKI:
-
Tyrosine kinase inhibitor
- VEGFR:
-
Vascular endothelial growth factor receptor
- HCC:
-
Hepatocellular carcinoma
- FGFR:
-
Fibroblast growth factor receptor
- PDGFR:
-
Platelet-derived growth factor receptor
- RET:
-
Proto-oncogenes rearranged during transfection
- KIT:
-
Stem cell factor receptor
- PLCγ:
-
Phospholipase-Cγ
- RAS:
-
Rat sarcoma
- RAF:
-
Extracellular signal-regulated kinase
- ERK:
-
Extracellular signal-regulated kinase
- PI3K:
-
Phosphatidylinositol 3-kinase
- AKT:
-
Ak strain transforming
- OS:
-
Overall survival
- DTC:
-
Differentiated thyroid cancer
- RECIST 1.1:
-
Response Evaluation Criteria in Solid Tumors RECIST Version 1.1
- RTKs:
-
Receptor tyrosine kinases
- ETS-1:
-
E26 transformation-specific sequence 1
- FGF:
-
Fibroblast growth factor
- HBV:
-
Hepatitis C virus
- MAPK:
-
Mitogen activated protein kinase
- HGF:
-
Hepatocyte growth factor
- c-MET:
-
C-mesenchymal-epithelial transition factor
- NF1:
-
Neurofibromin 1
- DUSP9:
-
Dual specificity phosphatase 9
- CRISPR:
-
Clustered regularly interspaced short palindromic repeats
- Cas9:
-
CRISPR-associated 9
- FOXO3:
-
Forkhead box O3
- gRNAs:
-
Guide RNAs
- EGFR:
-
Epidermal growth factor receptor
- IRF2:
-
Interferon regulatory factor 2
- PHGDH:
-
Phosphoglycerate dehydrogenase
- SSP:
-
Serine synthesis pathway
- ROS:
-
Reactive oxygen species
- α-KG:
-
α-Ketoglutarate
- ITGB8:
-
Integrin subunit beta 8
- EMT:
-
Epithelial–mesenchymal transition
- ZEB1:
-
Zinc-finger E-box binding protein 1
- CSCs:
-
Cancer stem cells
- GSK3β:
-
Glycogen synthase kinase 3β
- HNHA:
-
N-hydroxy-7-(2-naphthylthio) heptanomide
- HSCs:
-
Hepatic stellate cells
- ncRNAs:
-
Noncoding RNAs
- sncRNAs:
-
Short ncRNAs
- lncRNAs:
-
Long ncRNAs
- miRNAs:
-
MicroRNAs
- ceRNAs:
-
Competing endogenous RNAs
- circRNAs:
-
Circular RNAs
- circMED27:
-
CircRNA mediator complex subunit 27
- USP28:
-
Ubiquitin-specific peptidase 28
- pVEGFR 1–3:
-
Phosphorylated VEGFR 1–3
- CGIs:
-
CpG islands
- IGF1Rβ:
-
Insulin-like growth factor-1receptor β
- HIF1α:
-
Hypoxia-inducible factor 1-α
- HRE:
-
Hypoxia-responsive element
- Pink-1:
-
PTEN-induced kinase-1
- GSH:
-
Glutathione
- P-gp:
-
P-glycoprotein
- CRP:
-
C-reactive protein
- AFP:
-
Alpha-fetoprotein
- ORR:
-
Objective response rate
- mPFS:
-
Median progression-free survival
- Ang-2:
-
Angiopoietin-2
- TME:
-
Tumor microenvironment
- MDSCs:
-
Myeloid-derived suppressor cells
- eMDSCs:
-
Early-stage MDSCs
- PMN-MDSCs:
-
Polymorphonuclear MDSCs
- M-MDSCs:
-
Mononuclear MDSCs
- ATC:
-
Anaplastic thyroid cancer
- PD-1:
-
Programmed death receptor-1
- PAKs:
-
P21 activated kinases
- XPO1:
-
Exportin 1
- TEM:
-
Tie2-expressing macrophage
- RCC:
-
Renal cell carcinoma
- PTC:
-
Papillary thyroid cancer
- Tregs:
-
Regulatory T-cells
- IFN-γ:
-
Interferon-γ
- MAIT:
-
Mucosal-associated invariant T cells
- TNF:
-
Tumor necrosis factor
- PFS:
-
Progression-free survival
- FDA:
-
The US Food & Drug Administration
- MSI-H/dMMR:
-
Microsatellite instability-high or mismatch repair-deficient
- CNLC:
-
China liver cancer staging
- TACE/HAIC:
-
Transarterial chemoembolization/Hepatic artery infusion chemotherapy
- ICIs:
-
Immune check points inhibitors
- USP22:
-
Ubiquitin-specific protease 22
- PDX:
-
Patient-derived xenograft
- PDO:
-
Patient-derived organoid
References
Lemmon MA, Schlessinger J. Cell signaling by receptor tyrosine kinases. Cell. 2010;141(7):1117–34.
Matsui J, Funahashi Y, Uenaka T, Watanabe T, Tsuruoka A, Asada M. Multi-kinase inhibitor E7080 suppresses lymph node and lung metastases of human mammary breast tumor MDA-MB-231 via inhibition of vascular endothelial growth factor-receptor (VEGF-R) 2 and VEGF-R3 kinase. Clin Cancer Res. 2008;14(17):5459–65.
Lenvatinib approved for certain thyroid cancers, Cancer Discov 5(4) (2015) 338
FDA approves drug combo for kidney cancer, Cancer Discov 6(7) (2016) 687–688.
Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng AL. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163–73.
Lee C-H, Shah AY, Rasco D, Rao A, Taylor MH, Di Simone C, Hsieh JJ, Pinto A, Shaffer DR, Girones Sarrio R, Cohn AL, Vogelzang NJ, Bilen MA, Gunnestad Ribe S, Goksel M, Tennøe ØK, Richards D, Sweis RF, Courtright J, Heinrich D, Jain S, Wu J, Schmidt EV, Perini RF, Kubiak P, Okpara CE, Smith AD, Motzer RJ. Lenvatinib plus pembrolizumab in patients with either treatment-naive or previously treated metastatic renal cell carcinoma (Study 111/KEYNOTE-146): a phase 1b/2 study. Lancet Oncol. 2021;22(7):946–58.
Al-Salama ZT, Syed YY, Scott LJ. Lenvatinib: a review in hepatocellular carcinoma. Drugs. 2019;79(6):665–74.
Zhao Y, Zhang Y-N, Wang K-T, Chen L. Lenvatinib for hepatocellular carcinoma: from preclinical mechanisms to anti-cancer therapy. Biochim Biophys Acta. 2020;1874(1): 188391.
Kimura T, Kato Y, Ozawa Y, Kodama K, Ito J, Ichikawa K, Yamada K, Hori Y, Tabata K, Takase K, Matsui J, Funahashi Y, Nomoto K. Immunomodulatory activity of lenvatinib contributes to antitumor activity in the Hepa1-6 hepatocellular carcinoma model. Cancer Sci. 2018;109(12):3993–4002.
Yi C, Chen L, Lin Z, Liu L, Shao W, Zhang R, Lin J, Zhang J, Zhu W, Jia H, Qin L, Lu L, Chen J. Lenvatinib targets FGF receptor 4 to enhance antitumor immune response of anti-programmed cell death-1 in HCC. Hepatology. 2021;74(5):2544–60.
Adachi Y, Kamiyama H, Ichikawa K, Fukushima S, Ozawa Y, Yamaguchi S, Goda S, Kimura T, Kodama K, Matsuki M, Miyano SW, Yokoi A, Kato Y, Funahashi Y. Inhibition of FGFR reactivates IFNγ signaling in tumor cells to enhance the combined antitumor activity of lenvatinib with anti-PD-1 antibodies. Cancer Res. 2022;82(2):292–306.
Zhang Q, Liu H, Wang H, Lu M, Miao Y, Ding J, Li H, Gao X, Sun S, Zheng J. Lenvatinib promotes antitumor immunity by enhancing the tumor infiltration and activation of NK cells. Am J Cancer Res. 2019;9(7):1382–95.
Kato Y, Tabata K, Kimura T, Yachie-Kinoshita A, Ozawa Y, Yamada K, Ito J, Tachino S, Hori Y, Matsuki M, Matsuoka Y, Ghosh S, Kitano H, Nomoto K, Matsui J, Funahashi Y. Lenvatinib plus anti-PD-1 antibody combination treatment activates CD8+ T cells through reduction of tumor-associated macrophage and activation of the interferon pathway. PLoS ONE. 2019;14(2): e0212513.
Matsuki M, Hoshi T, Yamamoto Y, Ikemori-Kawada M, Minoshima Y, Funahashi Y, Matsui J. Lenvatinib inhibits angiogenesis and tumor fibroblast growth factor signaling pathways in human hepatocellular carcinoma models. Cancer Med. 2018;7(6):2641–53.
Hoshi T, Watanabe Miyano S, Watanabe H, Sonobe RMK, Seki Y, Ohta E, Nomoto K, Matsui J, Funahashi Y. Lenvatinib induces death of human hepatocellular carcinoma cells harboring an activated FGF signaling pathway through inhibition of FGFR-MAPK cascades. Biochem Biophys Res Commun. 2019;513(1):1–7.
Deng H, Kan A, Lyu N, Mu L, Han Y, Liu L, Zhang Y, Duan Y, Liao S, Li S, Xie Q, Gao T, Li Y, Zhang Z, Zhao M. Dual vascular endothelial growth factor receptor and fibroblast growth factor receptor inhibition elicits antitumor immunity and enhances programmed cell death-1 checkpoint blockade in hepatocellular carcinoma. Liver Cancer. 2020;9(3):338–57.
Finn RS, Ikeda M, Zhu AX, Sung MW, Baron AD, Kudo M, Okusaka T, Kobayashi M, Kumada H, Kaneko S, Pracht M, Mamontov K, Meyer T, Kubota T, Dutcus CE, Saito K, Siegel AB, Dubrovsky L, Mody K, Llovet JM. Phase Ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J Clin Oncol. 2020;38(26):2960–70.
Motzer R, Alekseev B, Rha S-Y, Porta C, Eto M, Powles T, Grünwald V, Hutson TE, Kopyltsov E, Méndez-Vidal MJ, Kozlov V, Alyasova A, Hong S-H, Kapoor A, Alonso Gordoa T, Merchan JR, Winquist E, Maroto P, Goh JC, Kim M, Gurney H, Patel V, Peer A, Procopio G, Takagi T, Melichar B, Rolland F, De Giorgi U, Wong S, Bedke J, Schmidinger M, Dutcus CE, Smith AD, Dutta L, Mody K, Perini RF, Xing D, Choueiri TK. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N Engl J Med. 2021;384(14):1289–300.
Motzer RJ, Hutson TE, Glen H, Michaelson MD, Molina A, Eisen T, Jassem J, Zolnierek J, Maroto JP, Mellado B, Melichar B, Tomasek J, Kremer A, Kim H-J, Wood K, Dutcus C, Larkin J. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015;16(15):1473–82.
Niu L, Liu L, Yang S, Ren J, Lai PBS, Chen GG. New insights into sorafenib resistance in hepatocellular carcinoma: Responsible mechanisms and promising strategies. Biochem Biophys Acta. 2017;1868(2):564–70.
Khan HY, Ge J, Nagasaka M, Aboukameel A, Mpilla G, Muqbil I, Szlaczky M, Chaker M, Baloglu E, Landesman Y, Mohammad RM, Azmi AS, Sukari A. Targeting XPO1 and PAK4 in 8505C anaplastic thyroid cancer cells: putative implications for overcoming lenvatinib therapy resistance. Int J Mol Sci. 2019;21:1.
Fu R, Jiang S, Li J, Chen H, Zhang X. Activation of the HGF/c-MET axis promotes lenvatinib resistance in hepatocellular carcinoma cells with high c-MET expression. Med Oncol. 2020;37:4.
Chong CR, Janne PA. The quest to overcome resistance to EGFR-targeted therapies in cancer. Nat Med. 2013;19(11):1389–400.
Tohyama O, Matsui J, Kodama K, Hata-Sugi N, Kimura T, Okamoto K, Minoshima Y, Iwata M, Funahashi Y. Antitumor activity of lenvatinib (e7080): an angiogenesis inhibitor that targets multiple receptor tyrosine kinases in preclinical human thyroid cancer models. J Thyroid Res. 2014;2014: 638747.
Ullah R, Yin Q, Snell AH, Wan L. RAF-MEK-ERK pathway in cancer evolution and treatment. Semin Cancer Biol. 2021;85:123.
Jin H, Shi Y, Lv Y, Yuan S, Ramirez CFA, Lieftink C, Wang L, Wang S, Wang C, Dias MH, Jochems F, Yang Y, Bosma A, Hijmans EM, de Groot MHP, Vegna S, Cui D, Zhou Y, Ling J, Wang H, Guo Y, Zheng X, Isima N, Wu H, Sun C, Beijersbergen RL, Akkari L, Zhou W, Zhai B, Qin W, Bernards R. EGFR activation limits the response of liver cancer to lenvatinib. Nature. 2021;595(7869):730–4.
Zhao Z, Zhang D, Wu F, Tu J, Song J, Xu M, Ji J. Sophoridine suppresses lenvatinib-resistant hepatocellular carcinoma growth by inhibiting RAS/MEK/ERK axis via decreasing VEGFR2 expression. J Cell Mol Med. 2021;25(1):549–60.
Simons M, Gordon E, Claesson-Welsh L. Mechanisms and regulation of endothelial VEGF receptor signalling. Nat Rev Mol Cell Biol. 2016;17(10):611–25.
Zhao Z, Song J, Zhang D, Wu F, Tu J, Ji J. Oxysophocarpine suppresses FGFR1-overexpressed hepatocellular carcinoma growth and sensitizes the therapeutic effect of lenvatinib. Life Sci. 2021;264: 118642.
Scartozzi M, Faloppi L, SvegliatiBaroni G, Loretelli C, Piscaglia F, Iavarone M, Toniutto P, Fava G, De Minicis S, Mandolesi A, Bianconi M, Giampieri R, Granito A, Facchetti F, Bitetto D, Marinelli S, Venerandi L, Vavassori S, Gemini S, D’Errico A, Colombo M, Bolondi L, Bearzi I, Benedetti A, Cascinu S. VEGF and VEGFR genotyping in the prediction of clinical outcome for HCC patients receiving sorafenib: the ALICE-1 study. Int J Cancer. 2014;135(5):1247–56.
Zheng Y-B, Zhan M-X, Zhao W, Liu B, Huang J-W, He X, Fu S-R, Zhao Y, Li Y, Hu B-S, Lu L-G. The relationship of kinase insert domain receptor gene polymorphisms and clinical outcome in advanced hepatocellular carcinoma patients treated with sorafenib. Med Oncol. 2014;31(10):209.
Hu Q, Hu X, Zhang L, Zhao Y, Li L. Targeting Hedgehog signalling in CD133-positive hepatocellular carcinoma: improving Lenvatinib therapeutic efficiency. Med Oncol. 2021;38(4):41.
Liu L, Aleksandrowicz E, Schönsiegel F, Gröner D, Bauer N, Nwaeburu CC, Zhao Z, Gladkich J, Hoppe-Tichy T, Yefenof E, Hackert T, Strobel O, Herr I. Dexamethasone mediates pancreatic cancer progression by glucocorticoid receptor, TGFβ and JNK/AP-1. Cell Death Dis. 2017;8(10): e3064.
Yao CD, Haensel D, Gaddam S, Patel T, Atwood SX, Sarin KY, Whitson RJ, McKellar S, Shankar G, Aasi S, Rieger K, Oro AE. AP-1 and TGFß cooperativity drives non-canonical Hedgehog signaling in resistant basal cell carcinoma. Nat Commun. 2020;11(1):5079.
Pungsrinont T, Kallenbach J, Baniahmad A. Role of PI3K-AKT-mTOR pathway as a pro-survival signaling and resistance-mediating mechanism to therapy of prostate cancer. Int J Mol Sci. 2021;22:20.
Mendoza MC, Er EE, Blenis J. The Ras-ERK and PI3K-mTOR pathways: cross-talk and compensation. Trends Biochem Sci. 2011;36(6):320–8.
Murali I, Kasar S, Naeem A, Tyekucheva S, Khalsa JK, Thrash EM, Itchaki G, Livitz D, Leshchiner I, Dong S, Fernandes SM, Getz G, Johnson A, Brown JR. Activation of the MAPK pathway mediates resistance to PI3K inhibitors in chronic lymphocytic leukemia. Blood. 2021;138(1):44–56.
Lu Y, Shen H, Huang W, He S, Chen J, Zhang D, Shen Y, Sun Y. Genome-scale CRISPR-Cas9 knockout screening in hepatocellular carcinoma with lenvatinib resistance. Cell Death Discov. 2021;7(1):359.
Hou W, Bridgeman B, Malnassy G, Ding X, Cotler SJ, Dhanarajan A, Qiu W. Integrin subunit beta 8 contributes to lenvatinib resistance in HCC. Hepatol Commun. 2022;1:1.
Yi Y, Wu H, Gao Q, He H-W, Li Y-W, Cai X-Y, Wang J-X, Zhou J, Cheng Y-F, Jin J-J, Fan J, Qiu S-J. Interferon regulatory factor (IRF)-1 and IRF-2 are associated with prognosis and tumor invasion in HCC. Ann Surg Oncol. 2013;20(1):267–76.
Guo Y, Xu J, Du Q, Yan Y, Geller DA. IRF2 regulates cellular survival and Lenvatinib-sensitivity of hepatocellular carcinoma (HCC) through regulating beta-catenin. Transl Oncol. 2021;14(6): 101059.
Wei L, Lee D, Law CT, Zhang MS, Shen J, Chin DW, Zhang A, Tsang FH, Wong CL, Ng IO, Wong CC, Wong CM. Genome-wide CRISPR/Cas9 library screening identified PHGDH as a critical driver for Sorafenib resistance in HCC. Nat Commun. 2019;10(1):4681.
Su C-Y, Li J-Q, Zhang L-L, Wang H, Wang F-H, Tao Y-W, Wang Y-Q, Guo Q-R, Li J-J, Liu Y, Yan Y-Y, Zhang J-Y. The biological functions and clinical applications of integrins in cancers. Front Pharmacol. 2020;11: 579068.
Zhou P, Li B, Liu F, Zhang M, Wang Q, Liu Y, Yao Y, Li D. The epithelial to mesenchymal transition (EMT) and cancer stem cells: implication for treatment resistance in pancreatic cancer. Mol Cancer. 2017;16(1):52.
Zeisberg M, Neilson EG. Biomarkers for epithelial-mesenchymal transitions. J Clin Invest. 2009;119(6):1429–37.
Singh A, Settleman J. EMT, cancer stem cells and drug resistance: an emerging axis of evil in the war on cancer. Oncogene. 2010;29(34):4741–51.
Kim SY, Kim SM, Chang HJ, Kim BW, Lee YS, Park CS, Park KC, Chang HS. SoLAT (Sorafenib Lenvatinib alternating treatment): a new treatment protocol with alternating Sorafenib and Lenvatinib for refractory thyroid cancer. BMC Cancer. 2018;18(1):956.
Lee YS, Kim SM, Kim BW, Chang HJ, Kim SY, Park CS, Park KC, Chang HS. Anti-cancer effects of HNHA and lenvatinib by the suppression of EMT-mediated drug resistance in cancer stem cells. Neoplasia. 2018;20(2):197–206.
Janda E, Lehmann K, Killisch I, Jechlinger M, Herzig M, Downward J, Beug H, Grünert S. Ras and TGF[beta] cooperatively regulate epithelial cell plasticity and metastasis: dissection of Ras signaling pathways. J Cell Biol. 2002;156(2):299–313.
Pardal R, Clarke MF, Morrison SJ. Applying the principles of stem-cell biology to cancer. Nat Rev Cancer. 2003;3(12):895–902.
Ma XL, Hu B, Tang WG, Xie SH, Ren N, Guo L, Lu RQ. CD73 sustained cancer-stem-cell traits by promoting SOX9 expression and stability in hepatocellular carcinoma. J Hematol Oncol. 2020;13(1):11.
Suzuki H, Maruyama R, Yamamoto E, Niinuma T, Kai M. Relationship between noncoding RNA dysregulation and epigenetic mechanisms in cancer. Adv Exp Med Biol. 2016;927:109–35.
Wei L, Sun J, Zhang N, Zheng Y, Wang X, Lv L, Liu J, Xu Y, Shen Y, Yang M. Noncoding RNAs in gastric cancer: implications for drug resistance. Mol Cancer. 2020;19(1):62.
Wei L, Wang X, Lv L, Liu J, Xing H, Song Y, Xie M, Lei T, Zhang N, Yang M. The emerging role of microRNAs and long noncoding RNAs in drug resistance of hepatocellular carcinoma. Mol Cancer. 2019;18(1):147.
Yu T, Yu J, Lu L, Zhang Y, Zhou Y, Zhou Y, Huang F, Sun L, Guo Z, Hou G, Dong Z, Wang B. MT1JP-mediated miR-24-3p/BCL2L2 axis promotes Lenvatinib resistance in hepatocellular carcinoma cells by inhibiting apoptosis. Cell Oncol (Dordr). 2021;44(4):821–34.
Hardwick JM, Soane L. Multiple functions of BCL-2 family proteins. Cold Spring Harb Perspect Biol. 2013;5:2.
Hansen TB, Jensen TI, Clausen BH, Bramsen JB, Finsen B, Damgaard CK, Kjems J. Natural RNA circles function as efficient microRNA sponges. Nature. 2013;495(7441):384–8.
Zhang P, Sun H, Wen P, Wang Y, Cui Y, Wu J. circRNA circMED27 acts as a prognostic factor and mediator to promote lenvatinib resistance of hepatocellular carcinoma. Mol Ther Nucleic Acids. 2022;27:293–303.
Arechederra M, Bazai SK, Abdouni A, Sequera C, Mead TJ, Richelme S, Daian F, Audebert S, Dono R, Lozano A, Gregoire D, Hibner U, Allende DS, Apte SS, Maina F. ADAMTSL5 is an epigenetically activated gene underlying tumorigenesis and drug resistance in hepatocellular carcinoma. J Hepatol. 2021;74(4):893–906.
Huang S, Zhu P, Sun B, Guo J, Zhou H, Shu Y, Li Q. Modulation of YrdC promotes hepatocellular carcinoma progression via MEK/ERK signaling pathway. Biomed Pharmacother. 2019;114: 108859.
Guo J, Zhu P, Ye Z, Wang M, Yang H, Huang S, Shu Y, Zhang W, Zhou H, Li Q. YRDC mediates the resistance of lenvatinib in hepatocarcinoma cells via modulating the translation of KRAS. Front Pharmacol. 2021;12: 744578.
Shin DS, Zaretsky JM, Escuin-Ordinas H, Garcia-Diaz A, Hu-Lieskovan S, Kalbasi A, Grasso CS, Hugo W, Sandoval S, Torrejon DY, Palaskas N, Rodriguez GA, Parisi G, Azhdam A, Chmielowski B, Cherry G, Seja E, Berent-Maoz B, Shintaku IP, Le DT, Pardoll DM, Diaz LA, Tumeh PC, Graeber TG, Lo RS, Comin-Anduix B, Ribas A. Primary resistance to PD-1 blockade mediated by JAK1/2 mutations. Cancer Discov. 2017;7(2):188–201.
Chong CR, Jänne PA. The quest to overcome resistance to EGFR-targeted therapies in cancer. Nat Med. 2013;19(11):1389–400.
Guan Y, Wang Y, Li B, Shen K, Li Q, Ni Y, Huang L. Mitophagy in carcinogenesis, drug resistance and anticancer therapeutics. Cancer Cell Int. 2021;21(1):350.
Zheng Y, Huang C, Lu L, Yu K, Zhao J, Chen M, Liu L, Sun Q, Lin Z, Zheng J, Chen J, Zhang J. STOML2 potentiates metastasis of hepatocellular carcinoma by promoting PINK1-mediated mitophagy and regulates sensitivity to lenvatinib. J Hematol Oncol. 2021;14(1):16.
Chourasia AH, Boland ML, Macleod KF. Mitophagy and cancer. Cancer Metab. 2015;3:4.
Rudin CM, Yang Z, Schumaker LM, VanderWeele DJ, Newkirk K, Egorin MJ, Zuhowski EG, Cullen KJ. Inhibition of glutathione synthesis reverses Bcl-2-mediated cisplatin resistance. Cancer Res. 2003;63(2):312–8.
Backos DS, Franklin CC, Reigan P. The role of glutathione in brain tumor drug resistance. Biochem Pharmacol. 2012;83(8):1005–12.
Shumaker RC, Aluri J, Fan J, Martinez G, Thompson GA, Ren M. Effect of rifampicin on the pharmacokinetics of lenvatinib in healthy adults. Clin Drug Investig. 2014;34(9):651–9.
Wei G, Huang L, Jiang Y, Shen Y, Huang Z, Huang Y, Sun X, Zhao C. Lenvatinib-zinc phthalocyanine conjugates as potential agents for enhancing synergistic therapy of multidrug-resistant cancer by glutathione depletion. Eur J Med Chem. 2019;169:53–64.
Slack FJ, Chinnaiyan AM. The role of non-coding RNAs in oncology. Cell. 2019;179(5):1033–55.
Zhang P, Sun H, Wen P, Wang Y, Cui Y, Wu J. circRNA circMED27 acts as a prognostic factor and mediator to promote lenvatinib resistance of hepatocellular carcinoma. Mol Therapy. 2022;27:293–303.
Hayashi T, Shibata M, Oe S, Miyagawa K, Honma Y, Harada M. C-reactive protein can predict dose intensity, time to treatment failure and overall survival in HCC treated with lenvatinib. PLoS ONE. 2020;15(12): e0244370.
Liu B, Shang X, Shi J-Y, Cui G-Z, Li X, Wang N-Y. Early alpha-fetoprotein response is associated with survival in patients with HBV-related hepatocellular carcinoma receiving lenvatinib. Front Oncol. 2022;12: 807189.
Myojin Y, Kodama T, Maesaka K, Motooka D, Sato Y, Tanaka S, Abe Y, Ohkawa K, Mita E, Hayashi Y, Hikita H, Sakamori R, Tatsumi T, Taguchi A, Eguchi H, Takehara T. ST6GAL1 is a novel serum biomarker for lenvatinib-susceptible FGF19-driven hepatocellular carcinoma. Clin Cancer Res. 2021;27(4):1150–61.
Eun JW, Yoon JH, Ahn HR, Kim S, Kim YB, Lim SB, Park W, Kang TW, Baek GO, Yoon MG, Son JA, Weon JH, Kim SS, Cho HJ, Cheong JY. Cancer-associated fibroblast-derived secreted phosphoprotein 1 contributes to resistance of hepatocellular carcinoma to sorafenib and lenvatinib. Cancer Commun (Lond). 2023;43(4):455–79.
Kudo M, Finn RS, Qin S, Han K-H, Ikeda K, Piscaglia F, Baron A, Park J-W, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng A-L. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet (London, England). 2018;391(10126):1163–73.
Raja A, Park I, Haq F, Ahn S-M. FGF19-signaling in hepatocellular carcinoma. Cells. 2019;8:6.
Yamauchi M, Ono A, Ishikawa A, Kodama K, Uchikawa S, Hatooka H, Zhang P, Teraoka Y, Morio K, Fujino H, Nakahara T, Murakami E, Miki D, Kawaoka T, Tsuge M, Hiramatsu A, Imamura M, Hayes CN, Fujita M, Nakagawa H, Yasui W, Aikata H, Chayama K. Tumor fibroblast growth factor receptor 4 level predicts the efficacy of lenvatinib in patients with advanced hepatocellular carcinoma. Clin Transl Gastroenterol. 2020;11(5): e00179.
Chuma M, Uojima H, Numata K, Hidaka H, Toyoda H, Hiraoka A, Tada T, Hirose S, Atsukawa M, Itokawa N, Arai T, Kako M, Nakazawa T, Wada N, Iwasaki S, Miura Y, Hishiki S, Nishigori S, Morimoto M, Hattori N, Ogushi K, Nozaki A, Fukuda H, Kagawa T, Michitaka K, Kumada T, Maeda S. Early changes in circulating FGF19 and Ang-2 levels as possible predictive biomarkers of clinical response to lenvatinib therapy in hepatocellular carcinoma. Cancers. 2020;12:2.
Finn RS, Kudo M, Cheng A-L, Wyrwicz L, Ngan RKC, Blanc J-F, Baron AD, Vogel A, Ikeda M, Piscaglia F, Han K-H, Qin S, Minoshima Y, Kanekiyo M, Ren M, Dairiki R, Tamai T, Dutcus CE, Ikezawa H, Funahashi Y, Evans TRJ. Pharmacodynamic biomarkers predictive of survival benefit with lenvatinib in unresectable hepatocellular carcinoma: from the phase III REFLECT study. Clin Cancer Res. 2021;27(17):4848–58.
Wu T, Dai Y. Tumor microenvironment and therapeutic response. Cancer Lett. 2017;387:61–8.
Bronte V, Brandau S, Chen S-H, Colombo MP, Frey AB, Greten TF, Mandruzzato S, Murray PJ, Ochoa A, Ostrand-Rosenberg S, Rodriguez PC, Sica A, Umansky V, Vonderheide RH, Gabrilovich DI. Recommendations for myeloid-derived suppressor cell nomenclature and characterization standards. Nat Commun. 2016;7:12150.
Gunda V, Gigliotti B, Ashry T, Ndishabandi D, McCarthy M, Zhou Z, Amin S, Lee KE, Stork T, Wirth L, Freeman GJ, Alessandrini A, Parangi S. Anti-PD-1/PD-L1 therapy augments lenvatinib’s efficacy by favorably altering the immune microenvironment of murine anaplastic thyroid cancer. Int J Cancer. 2019;144(9):2266–78.
L. Torrens, C. Montironi, M. Puigvehí, A. Mesropian, J. Leslie, P.K. Haber, M. Maeda, U. Balaseviciute, C.E. Willoughby, J. Abril-Fornaguera, M. Piqué-Gili, M. Torres-Martín, J. Peix, D. Geh, E. Ramon-Gil, B. Saberi, S.L. Friedman, D.A. Mann, D. Sia, J.M. Llovet, Immunomodulatory Effects of Lenvatinib Plus Anti-Programmed Cell Death Protein 1 in Mice and Rationale for Patient Enrichment in Hepatocellular Carcinoma, Hepatology (Baltimore, Md.) 74(5) (2021) 2652–2669.
Tang W, Chen Z, Zhang W, Cheng Y, Zhang B, Wu F, Wang Q, Wang S, Rong D, Reiter FP, De Toni EN, Wang X. The mechanisms of sorafenib resistance in hepatocellular carcinoma: theoretical basis and therapeutic aspects. Signal Transduct Target Ther. 2020;5(1):87.
Niu L, Liu L, Yang S, Ren J, Lai PBS, Chen GG. New insights into sorafenib resistance in hepatocellular carcinoma: responsible mechanisms and promising strategies. Biochim Biophys Acta Rev Cancer. 2017;1868(2):564–70.
Nakagawa T, Matsushima T, Kawano S, Nakazawa Y, Kato Y, Adachi Y, Abe T, Semba T, Yokoi A, Matsui J, Tsuruoka A, Funahashi Y. Lenvatinib in combination with golvatinib overcomes hepatocyte growth factor pathway-induced resistance to vascular endothelial growth factor receptor inhibitor. Cancer Sci. 2014;105(6):723–30.
Nakazawa Y, Kawano S, Matsui J, Funahashi Y, Tohyama O, Muto H, Nakagawa T, Matsushima T. Multitargeting strategy using lenvatinib and golvatinib: maximizing anti-angiogenesis activity in a preclinical cancer model. Cancer Sci. 2015;106(2):201–7.
Datta M, Via LE, Kamoun WS, Liu C, Chen W, Seano G, Weiner DM, Schimel D, England K, Martin JD, Gao X, Xu L, Barry CE, Jain RK. Anti-vascular endothelial growth factor treatment normalizes tuberculosis granuloma vasculature and improves small molecule delivery. Proc Natl Acad Sci U S A. 2015;112(6):1827–32.
Augustin HG, Koh GY, Thurston G, Alitalo K. Control of vascular morphogenesis and homeostasis through the angiopoietin-tie system. Nat Rev Mol Cell Biol. 2009;10(3):165–77.
Coffelt SB, Tal AO, Scholz A, De Palma M, Patel S, Urbich C, Biswas SK, Murdoch C, Plate KH, Reiss Y, Lewis CE. Angiopoietin-2 regulates gene expression in TIE2-expressing monocytes and augments their inherent proangiogenic functions. Cancer Res. 2010;70(13):5270–80.
Jacob A, Shook J, Hutson T. The implementation of lenvatinib/everolimus or lenvatinib/pembrolizumab combinations in the treatment of metastatic renal cell carcinoma. Expert Rev Anticancer Ther. 2021;21(4):365–72.
Tomonari T, Sato Y, Tanaka H, Tanaka T, Taniguchi T, Sogabe M, Okamoto K, Miyamoto H, Muguruma N, Takayama T. Sorafenib as second-line treatment option after failure of lenvatinib in patients with unresectable hepatocellular carcinoma. JGH Open. 2020;4(6):1135–9.
Tomonari T, Sato Y, Tanaka H, Tanaka T, Fujino Y, Mitsui Y, Hirao A, Taniguchi T, Okamoto K, Sogabe M, Miyamoto H, Muguruma N, Kagiwada H, Kitazawa M, Fukui K, Horimoto K, Takayama T. Potential use of lenvatinib for patients with unresectable hepatocellular carcinoma including after treatment with sorafenib: real-world evidence and assessment via protein phosphorylation array. Oncotarget. 2020;11(26):2531–42.
Terashima T, Yamashita T, Takata N, Takeda Y, Kido H, Iida N, Kitahara M, Shimakami T, Takatori H, Arai K, Kawaguchi K, Kitamura K, Yamashita T, Sakai Y, Mizukoshi E, Honda M, Kaneko S. Safety and efficacy of sorafenib followed by regorafenib or lenvatinib in patients with hepatocellular carcinoma. Hepatol Res. 2021;51(2):190–200.
Hiraoka A, Kumada T, Atsukawa M, Hirooka M, Tsuji K, Ishikawa T, Takaguchi K, Kariyama K, Itobayashi E, Tajiri K, Shimada N, Shibata H, Ochi H, Tada T, Toyoda H, Nouso K, Tsutsui A, Nagano T, Itokawa N, Hayama K, Imai M, Joko K, Koizumi Y, Hiasa Y, Michitaka K, Kudo M. Prognostic factor of lenvatinib for unresectable hepatocellular carcinoma in real-world conditions-multicenter analysis. Cancer Med. 2019;8(8):3719–28.
Xing R, Gao J, Cui Q, Wang Q. Strategies to improve the antitumor effect of immunotherapy for hepatocellular carcinoma. Front Immunol. 2021;12: 783236.
Zhou C, Sun B-Y, Zhou P-Y, Yang Z-F, Wang Z-T, Liu G, Gan W, Wang Z, Zhou J, Fan J, Yi Y, Ren N, Qiu S-J. MAIT cells confer resistance to Lenvatinib plus anti-PD1 antibodies in hepatocellular carcinoma through TNF-TNFRSF1B pathway. Clin Immunol. 2023;256: 109770.
Kim S-M, Park K-C, Jeon J-Y, Kim B-W, Kim H-K, Chang H-J, Choi S-H, Park C-S, Chang H-S. Potential anti-cancer effect of N-hydroxy-7-(2-naphthylthio) heptanomide (HNHA), a novel histone deacetylase inhibitor, for the treatment of thyroid cancer. BMC Cancer. 2015;15:1003.
Hou F-J, Guo L-X, Zheng K-Y, Song J-N, Wang Q, Zheng Y-G. Chelidonine enhances the antitumor effect of lenvatinib on hepatocellular carcinoma cells. Onco Targets Ther. 2019;12:6685–97.
Xu Q, Li Q, Yang Z, Huang P, Hu H, Mo Z, Qin Z, Xu Z, Chen T, Yang S. Lenvatinib and Cu2-xS nanocrystals co-encapsulated in poly(D,L-lactide-co-glycolide) for synergistic chemo-photothermal therapy against advanced hepatocellular carcinoma. J Mater Chem B. 2021;9(48):9908–22.
Xu Q, Hu H, Mo Z, Chen T, He Q, Xu Z. A multifunctional nanotheranostic agent based on Lenvatinib for multimodal synergistic hepatocellular carcinoma therapy with remarkably enhanced efficacy. J Colloid Interface Sci. 2023;638:375–91.
Zhang D, Jiang C, Zheng X, Lin Z, Zhuang Q, Xie H, Liang Y, Xu Y, Cui L, Liu X, Zeng Y. Normalization of tumor vessels by lenvatinib-based metallo-nanodrugs alleviates hypoxia and enhances calreticulin-mediated immune responses in orthotopic HCC and organoids. Small. 2023;19(29): e2207786.
Wu Y, Zhu R, Zhou M, Liu J, Dong K, Zhao S, Cao J, Wang W, Sun C, Wu S, Wang F, Shi Y, Sun Y. Homologous cancer cell membrane-camouflaged nanoparticles target drug delivery and enhance the chemotherapy efficacy of hepatocellular carcinoma. Cancer Lett. 2023;558: 216106.
Luo Y, Wang J, Xu L, Du Q, Fang N, Wu H, Liu F, Hu L, Xu J, Hou J, Zhong Y, Liu Y, Wang Z, Ran H, Guo D. A theranostic metallodrug modulates immunovascular crosstalk to combat immunosuppressive liver cancer. Acta Biomater. 2022;154:478–96.
Makker V, Rasco D, Vogelzang NJ, Brose MS, Cohn AL, Mier J, Di Simone C, Hyman DM, Stepan DE, Dutcus CE, Schmidt EV, Guo M, Sachdev P, Shumaker R, Aghajanian C, Taylor M. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer: an interim analysis of a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2019;20(5):711–8.
Makker V, Colombo N, Casado Herráez A, Santin AD, Colomba E, Miller DS, Fujiwara K, Pignata S, Baron-Hay S, Ray-Coquard I, Shapira-Frommer R, Ushijima K, Sakata J, Yonemori K, Kim YM, Guerra EM, Sanli UA, McCormack MM, Smith AD, Keefe S, Bird S, Dutta L, Orlowski RJ, Lorusso D. Lenvatinib plus pembrolizumab for advanced endometrial cancer. N Engl J Med. 2022;386(5):437–48.
Kawazoe A, Fukuoka S, Nakamura Y, Kuboki Y, Wakabayashi M, Nomura S, Mikamoto Y, Shima H, Fujishiro N, Higuchi T, Sato A, Kuwata T, Shitara K. Lenvatinib plus pembrolizumab in patients with advanced gastric cancer in the first-line or second-line setting (EPOC1706): an open-label, single-arm, phase 2 trial. Lancet Oncol. 2020;21(8):1057–65.
Gaspar N, Venkatramani R, Hecker-Nolting S, Melcon SG, Locatelli F, Bautista F, Longhi A, Lervat C, Entz-Werle N, Casanova M, Aerts I, Strauss SJ, Thebaud E, Morland B, Nieto AC, Marec-Berard P, Gambart M, Rossig C, Okpara CE, He C, Dutta L, Campbell-Hewson Q. Lenvatinib with etoposide plus ifosfamide in patients with refractory or relapsed osteosarcoma (ITCC-050): a multicentre, open-label, multicohort, phase 1/2 study. Lancet Oncol. 2021;22(9):1312–21.
Llovet JM, Kudo M, Merle P, Meyer T, Qin S, Ikeda M, Xu R, Edeline J, Ryoo B-Y, Ren Z, Masi G, Kwiatkowski M, Lim HY, Kim JH, Breder V, Kumada H, Cheng A-L, Galle PR, Kaneko S, Wang A, Mody K, Dutcus C, Dubrovsky L, Siegel AB, Finn RS. Lenvatinib plus pembrolizumab versus lenvatinib plus placebo for advanced hepatocellular carcinoma (LEAP-002): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2023;24(12):1399–410.
Bedke J, Albiges L, Capitanio U, Giles RH, Hora M, Lam TB, Ljungberg B, Marconi L, Klatte T, Volpe A, Abu-Ghanem Y, Dabestani S, Pello SF, Hofmann F, Kuusk T, Tahbaz R, Powles T, Bex A. The 2021 updated European association of urology guidelines on renal cell carcinoma: immune checkpoint inhibitor-based combination therapies for treatment-naive metastatic clear-cell renal cell carcinoma are standard of care. Eur Urol. 2021;80(4):393–7.
Makker V, Colombo N, Herráez AC, Monk BJ, Mackay H, Santin AD, Miller DS, Moore RG, Baron-Hay S, Ray-Coquard I, Ushijima K, Yonemori K, Kim YM, Guerra Alia EM, Sanli UA, Bird S, Orlowski R, McKenzie J, Okpara C, Barresi G, Lorusso D. Lenvatinib plus pembrolizumab in previously treated advanced endometrial cancer: updated efficacy and safety from the randomized phase III study 309/KEYNOTE-775. J Clin Oncol. 2023;41(16):2904–10.
NIH, ClinicalTrials.gov. https://clinicaltrials.gov/ct2/home.
You Q. Supplementary files: a summary about ongoing clinical trials of lenvatinib in combination with different drugs/therapeutic methods. Mendeley Data V1. 2023. https://doi.org/10.17632/5c4b8f8yxh.1.
Cannarile MA, Gomes B, Canamero M, Reis B, Byrd A, Charo J, Yadav M, Karanikas V. Biomarker technologies to support early clinical immuno-oncology development: advances and interpretation. Clin Cancer Res. 2021;27(15):4147–59.
Huang A, Yang X-R, Chung W-Y, Dennison AR, Zhou J. Targeted therapy for hepatocellular carcinoma. Signal Transduct Target Ther. 2020;5(1):146.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Bioengineering Research Center Cultivation Platform (WW201905), the National Natural Science Foundation of China (81900597, 81802897, 81901943, 81770648, 81970567), the Science and Technology Program of Guangdong Province (2019B020236003), the Science and Technology Program of Guangzhou City (201803040005), the Natural Science Foundation of Guangdong Province (2019A1515011698, 2021A1515012136, 2021A1515011156, 2021A1515010571), the Guangdong Basic and Applied Basic Research Foundation (2021A1515111058), the Guangzhou Basic and Applied Basic Research Foundation (202102020237), the Major talent project cultivation plan project (P02093).
Author information
Authors and Affiliations
Contributions
QY and RL carried out the literature searches, prepared figures and tables, did writing and editing; JY and YCZ did writing and editing; QY, JYC, XS, CCX, JBZ, JQX, and HTC did the literature searches and data interpretation; YY and JZ conceptualized the paper, did writing and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors have no competing interests to declare.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
You, Q., Li, R., Yao, J. et al. Insights into lenvatinib resistance: mechanisms, potential biomarkers, and strategies to enhance sensitivity. Med Oncol 41, 75 (2024). https://doi.org/10.1007/s12032-023-02295-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-023-02295-0