Abstract
Over the last decade, Canada has experienced a substantial increase in people dying from substance-related acute toxicity. Examining mortality rates by area-level characteristics can identify disproportionately affected populations and inform strategies to reduce substance-related acute toxicity deaths (ATDs). Using area-based methods, this study sought to examine substance-related acute toxicity mortality rates for varying community population sizes, levels of community remoteness, and indicators of deprivation in Canada from 2016 to 2017. Age-standardized mortality rates and rate ratios were calculated and disaggregated by sex. Mortality rates were highest in mid-sized urban communities with populations of 100,000 to 499,999 residents (15.9 per 100,000 population), followed by larger cities of 500,000 to 1,499,999 (15.1 per 100,000 population). The distribution of people who died also varied by community remoteness, with the highest mortality rates observed in accessible areas (14.9 per 100,000 population), followed by very remote areas (14.7 per 100,000 population). Neighbourhoods with the highest levels of deprivation, including high residential instability, economic dependency, and situational vulnerability, experienced 1.5 to 3.2 times more ATDs compared to neighbourhoods with the lowest levels of deprivation. Reported trends were similar among males and females, with higher mortality rates for males across all area-level characteristics. This study provides novel evidence on the context surrounding deaths to inform responses to reduce ATDs in Canada and serves as an important baseline that can be used to measure future progress.
Similar content being viewed by others
Introduction
Over the last decade, Canada has experienced a substantial rise in substance-related acute toxicity deaths (ATDs), sometimes referred to as “overdose” or “poisoning” deaths. Many of these deaths have been opioid-related with 38,514 people dying of apparent opioid toxicity in Canada between January 2016 and March 2023 (SAC, 2023). Much of the available evidence on substance-related ATDs in Canada has focused on opioid-related deaths, as the rise in ATDs was largely attributed to the presence of synthetic opioids in the unregulated drug supply. However, ATDs often involve multiple substances; for example, there has been a rise in opioid-related deaths that also involve stimulants or benzodiazepines (PHAC, 2022; Konefal et al., 2022), highlighting the polysubstance nature of deaths in Canada. The risk of acute toxicity may not depend only on the substances involved, but also on individual level factors as well as broader social and structural determinants.
In 2017, acute toxicity deaths in Canada occurred at substantially higher rates than those for motor-vehicle collisions and other leading causes of premature death (Fischer et al., 2019) and have contributed to a depreciation of overall gains in life expectancy between 2014 and 2016 (Orpana et al., 2019). This crisis has affected communities across North America but is most concentrated in neighbourhoods experiencing high levels of poverty, marginalization, and deprivation (Alsabbagh et al., 2022; Kurani et al., 2020; Pawer et al., 2021). Based on nationally representative survey data from Canada, the prevalence of illicit substance use appears higher in groups with lower income, compared to the highest income group, and lower in rural areas, compared to urban areas (Blair & Siddiqi, 2022). Disparities in ATD rates between communities have not been fully explained by substance use patterns, and instead might be a result of factors such as level of urbanicity, access to treatment and harm reduction services, socioeconomic inequities, and social determinants of health (Galea & Vlahov, 2002; Kurani et al., 2020; Pawer et al., 2021; Thomas, 2007; Young et al., 2022). For example, lower socioeconomic status is associated with chronic exposure to stressors, and more limited access to social and health supports and services, which can increase risks associated with substance use and related harms (Amaro et al., 2021; Pawer et al., 2021). Additionally, substance use can be related to a range of harms, including negative impacts on physical health, including acute toxicity, as well as mental health, employment, income, housing, and social connection (Carrière et al., 2018; Cohen et al., 2022). Substance-related harms can be amplified by experiences of stigma and create further barriers in accessing care for people who use substances (Cohen et al., 2022; Park et al., 2020; Thompson et al, 2023), emphasizing the complex interplay of health, social, and structural factors in increasing risk of substance-related ATDs.
Although current research suggests that ATD rates are higher in urban areas (Gomes et al., 2021; Hedegaard & Spencer, 2021; Spencer et al., 2022), the geographic distribution of deaths may differ between jurisdictions and may change over time. A report on hospitalizations due to opioid poisonings in Canada between 2016 and 2017 found that rates were highest in medium-sized urban centres with populations between 50,000 and 99,999 residents (CIHI, 2018). Provincial reports from across Canada indicate that the majority of substance-related ATDs have occurred among people who resided in large urban population centres, though many deaths also occurred on the perimeter of these urban centres (PHO, 2019; British Columbia Coroners Service, 2017; Alberta Health, 2019; Manitoba Health, 2017). For example, geographic analysis of people who died due to opioid-related acute toxicity in Ontario during the COVID-19 pandemic from March to December 2020 demonstrated considerable increases across regions of all population densities, with the largest absolute increases occurring in large urban centres (Gomes et al., 2021). However, significant increases in the relative rate of opioid-related deaths also occurred in the most rural and northern regions of the province (Gomes et al., 2021). Moreover, an analysis of acute toxicity events in British Columbia found that the likelihood of fatal acute toxicity was significantly higher in rural areas compared to large urban centres (Hu et al., 2022).
Deprivation, defined as the “inability for individuals and communities to attain basic resources and services” (Public Health Ontario (PHO), 2019) such as food, housing, employment, education or social support and connection, is a significant and often under-examined determinant of substance-related ATDs. In Ontario, ATDs occur across all socioeconomic groups; however, approximately one-third of people who died resided in the most materially deprived neighbourhoods (Public Health Ontario (PHO), 2019). A variety of structural and social neighbourhood characteristics have been linked to disproportionate levels of ATDs and are theorized to operate through a variety of mechanisms, both at the individual-level as well as systemically through the distribution of resources (Bradford & Bradford, 2020; Hollingsworth et al., 2017; Kurani et al., 2020; Pear et al., 2019). For example, neighbourhood-level income may influence substance use behaviours and the risk of experiencing harm through allocation of resources such as education, housing, employment and healthcare (Pawer et al., 2021). Moreover, people who have been periodically or chronically unhoused or living in unstable circumstances are overrepresented among those who died of acute toxicity in Canada (SAC, 2022).
There is limited national-level evidence available to describe the geographic, demographic, and socioeconomic circumstances of people who have died from substance-related acute toxicity in Canada. When information on individual-level indicators is unavailable or incomplete, area-based measures are commonly used to measure and track geographic and socioeconomic information (Pampalon et al., 2009). Understanding determinants and area-level characteristics of substance-related ATDs was identified as an important evidence gap among subject matter experts, including people with lived experience of substance use, who were involved in planning this study as this information will identify areas of unmet needs and help develop tailored interventions to reduce substance-related ATDs. To address this gap, this study linked data from coroner and medical examiner charts of people who have died from acute toxicity in Canada from 2016 to 2017 with area-level data sources to measure and compare mortality rates in urban and rural communities of different sizes and of different levels of metropolitan influence and remoteness. Additionally, we integrated data from four composite measures of neighbourhood-level deprivation to assess whether there were trends in ATD rates observed from the least deprived to most deprived neighbourhoods.
Methods
Data Sources
This retrospective observational study involved linking data from four sources. The first data source was a national chart review study of coroner and medical examiner files for all residents of Canada who died from substance-related acute toxicity between January 1, 2016, and December 31, 2017. This study included all individuals who, according to the death certificate, autopsy report or coroner or medical examiner report, died after an acute toxicity resulting from substance use where one or more of the substances were a drug or alcohol. Substances involved in deaths included illegal (unregulated), controlled and pharmaceutical drugs (including prescription and over-the counter products); alcohol and chemicals not intended for human use (e.g. veterinary drugs, non-pharmaceutical inhalants and household or industrial chemicals). An overview of the substances involved in deaths from the data source study has been previously published (PHAC, 2022). The study included deaths with an unintentional (accidental), intentional (suicide) or undetermined manner of death. The national chart review study includes data from all of Canada’s provinces and territories on demographic, socioeconomic and health characteristics of those who have died, the substances involved in the acute toxicity death and the circumstances surrounding the death (PHAC, 2022). Further details on the methods, limitations, substances involved and inclusion and exclusion criteria of the national chart review study have been previously reported (Rotondo et al., 2023).
Individual-level data from the chart review study were linked with Statistics Canada’s Postal Code Conversion File Plus (PCCF +) using the postal code of usual residence for each person who died. The PCCF + is a SAS control program developed by Statistics Canada in 2017 with a set of associated datasets from the Postal Code Conversion File and supplementary data (including population weights that assign standard geographic identifiers and areas based on postal code) (Statistics Canada, 2021a). Data were then linked with Statistics Canada’s Index of Remoteness (RI), which measures the geographic proximity of census subdivisions (CSD) to population centres, according to a given travel radius and population size (Statistics Canada, 2021b). The RI was linked to the national chart review dataset using the CSD unique identifier, which was obtained through the PCCF + linkage. Finally, chart review study data were linked to Statistic Canada’s Canadian Index of Multiple Deprivation (CIMD) using dissemination area (DA) unique identifiers. DAs have a population of approximately 400 to 700 residents and are the smallest standard geographical area for which all census data is collected in Canada (Statistics Canada, 2016). The CIMD is a validated, geographically based index of material and social deprivation consisting of four composite dimensions, including residential instability, economic dependency, ethno-cultural composition and situational vulnerability (Statistics Canada, 2019). The CIMD uses information from the 2016 Census to derive DA or neighbourhood–level indicators.
Study Variables
Demographic and Death Variables
Data on the age, sex (male or female), manner of death (intentional, unintentional or undetermined), postal code of usual residence and municipality of usual residence of people who died from acute toxicity were obtained from the chart review study of substance-related ATDs.
Community Population Size
Throughout this paper, we use the term community population size to refer to the variable community size and metropolitan influence zone (CSizeMIZ), derived from the PCCF + linkage to identify urban and rural community population sizes. CSizeMIZ classifies urban areas based on the 2016 Census population size of each Census Metropolitan Area (CMA: a population of at least 100,000 residents) and Census Agglomeration (CA: a population of at least 10,000 residents). Rural areas are identified by metropolitan influence zones according to the degree of influence of CMAs and CAs (strong, moderate, weak, or no influence), based on the percentage of the population who commute to work in a CMA or CA core. Of the 9414 cases in the chart review study dataset, 22.6% were missing postal code of residence or did not have a valid postal code (e.g. postal code contained errors or was incomplete) and were therefore excluded from PCCF + linkage. The records with missing data were reviewed for additional location information (including municipality of residence), and CSizeMIZ categories were imputed based on manually reviewed information where possible. For the community size analysis, an additional 17.9% were imputed. The final community size analysis excluded 4.7% of all records due to unavailable data, and a total of 8973 people were included.
Community Remoteness
The term community remoteness is used throughout this paper to refer to the variable derived from the RI, which assigns relative remoteness values to almost all Canadian CSDs on a scale of 0 to 1, where 0 is the most accessible community and 1 is the least accessible (or most remote) community. The continuous RI values are classified into five discrete categories: easily accessible areas (RI, < 0.1500); accessible areas (RI, 0.1500 to 0.2888); less accessible areas (RI, 0.2889 to 0.3898); remote areas (RI, 0.3899 to 0.5532) and very remote areas (RI, > 0.5532) (Subedi et al., 2020). For the analysis of community remoteness, records that could not be linked with the PCCF + (22.6%) were manually reviewed, as they were for the community size analysis, and an additional 17.9% of records were imputed from the available location data. The final community remoteness analysis excluded 4.7% of all records due to unavailable data and a total of 8,985 people were included.
Neighbourhood-Level Indicators of Deprivation
The term neighbourhood-level indicators of deprivation is used throughout this paper to denote the four composite dimensions of the CIMD described in Table 1. The CIMD assigns each DA in Canada a quintile ranking, where a value of 1 corresponds to DAs with the lowest level of deprivation or concentration for that dimension, and a value of 5 corresponds to DAs with the highest level of deprivation or concentration. The CIMD includes all provincial DAs with the exception of approximately 500 DAs with very small populations (less than 40) that were suppressed (Statistics Canada, 2019). A total of 23.2% of records were excluded from the CIMD analysis, which includes the records that could not be linked with the PCCF + (22.6% of all records). The CIMD contains DA-level data (a smaller level of geography than community size or remoteness), which could not be imputed based on the other location information available (e.g. municipality) among records that were missing postal code of residence. In addition, 0.6% of cases that were linked with the PCCF + were excluded due to suppression of very small DAs, as mentioned above. A total of 7230 people were included in the CIMD analysis.
Statistical Analysis
We calculated the per cent distribution of people who died due to substance-related acute toxicity by sex, age, manner of death and by area-level characteristics. To protect privacy, all values less than 10 were suppressed, and all percentages were calculated using numbers that were randomly rounded to base three (Hundepool et al., 2010). For base three rounding, values that are a multiple of three remain unchanged, while values that are not a multiple of three have a two-thirds chance of rounding to the nearest multiple of three and a one-third chance of rounding to the second nearest multiple of three. Column percentage totals were also independently randomly rounded to base three and therefore may not always sum up to 100%.
Next, we calculated age-standardized mortality rates (ASMR) per 100,000 population for each category of community population size and community remoteness, and for each quintile of the CIMD. Mortality rates were adjusted by age using direct standardization to control for differences in age distributions across communities. The Canadian population from the 2016 Census was used as the standard population, with 10-year age categories for the rate denominator. Rate ratios (RRs) were computed to compare the mortality rates amongst groups by dividing the rate in one group by the rate of the comparison or reference group. For example, differences in ASMR by community population sizes were analysed by calculating RRs using the largest community population size (1,500,000 or more residents) as a reference category. Similarly, RRs of ASMR by community remoteness were calculated using the easily accessible area as the reference category. For neighbourhood-level indicators of deprivation, the RRs of ASMR were calculated using the least deprived or concentrated quintile (quintile 1) as the reference category. The corresponding 95% confidence intervals (CIs) were calculated for each RR to understand the statistical significance of these estimates. For example, if the CI of a RR crosses the null (i.e. 1.0), then the ASMR is not significantly different than the reference category (Tan & Tan, 2010). Lastly, we stratified the analyses by sex. All statistical analyses were conducted using SAS Enterprise Guide 7.1.
Results
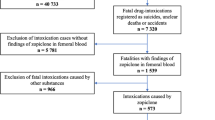
Of the 9414 people who died of a substance-related acute toxicity between January 1, 2016, and December 31, 2017, in Canada, 8973 people were included in the community size analysis, 8985 people were included in the community remoteness analysis, and 7230 people were included in the analysis of neighbourhood-level indicators of deprivation (Fig. 1). The per cent distribution of people who died of an acute toxicity event by community population size, community remoteness and neighbourhood-level indicators of deprivation by sex, age and manner of death is displayed in Table 2. Across all area-level characteristics presented in this report, the majority of deaths were unintentional and occurred more often in males and people aged 30 to 59 years (Table 2).
Community Population Size
Over 50% of people in Canada who died of acute toxicity between 2016 and 2017 lived in larger urban communities (CMAs) with 500,000 or more residents (Table 2). ASMRs, however, were highest in communities with a population of 100,000 to 499,999 residents (15.9 per 100,000 population), followed by communities with 500,000 to 1,499,999 (15.1 per 100,000 population) and 10,000 to 99,999 residents (14.6 per 100,000 population) (Table 3). These rates were significantly higher than those observed in the largest communities with 1,500,000 or more residents (RR ranged from 1.4 to 1.5) (Fig. 2). In rural communities with a strong metropolitan influence, the mortality rate (7.9 per 100,000 population) was significantly lower than the rate in the largest communities with 1,500,000 or more residents (RR, 0.7, 95% CI, 0.6, 0.9). There was little difference in mortality rates between rural communities with moderate or weak/no metropolitan influence and communities with 1,500,000 or more residents (Table 3). However, for females, ASMRs were significantly higher in rural communities with moderate or weak/no metropolitan influence compared to the largest communities of 1,500,000 or more residents (RR ranged from 1.4 to 1.8) (Table 3; Fig. 2).
Age-standardized mortality rate ratios (per 100,000 population) and corresponding 95% confidence intervals (CIs) of people who died of an acute toxicity in 2016 or 2017 by community population size (CSizeMIZ category) and sex. ASMR, age-standardized mortality rate; CI, confidence interval; MIZ, metropolitan influence zone. Rate ratios were calculated using the largest community population size (1,500,000 or more residents) as a reference category, which is represented by the red dashed line in the figure. Error bars display 95% confidence intervals. If the error bar crosses the red dotted line, then that category is not significantly different than the reference category
Community Remoteness
The majority of people who died of acute toxicity resided in accessible or easily accessible areas (83.2%), and 69.5% of these deaths were unintentional (Table 2). ASMRs were highest in accessible (14.9 per 100,000 population) and very remote areas (14.7 per 100,000 population) and lowest in easily accessible (12.7 per 100,000 population) and remote areas (12.7 per 100,000 population) (Table 4). There were negligible differences in ASMRs across levels of community remoteness, as rate ratios ranged from 1.0 to 1.2 with overlapping CIs (Table 4; Fig. 3). For females, the mortality rate in accessible areas was significantly higher than easily accessible areas (RR: 1.4, 95% CI, 1.3, 1.6). While the highest ASMR was observed in very remote areas (11.3 per 100,000 population), this rate did not significantly differ from the reference category (RR, 1.7; 95% CI, 1.0, 2.8) (Table 4; Fig. 3). For males, ASMRs ranged from 16.1 per 100,000 population in remote areas to 20.3 per 100,000 population in less accessible areas. Despite the high rates observed in males compared to females, there were no significant differences in rates across levels of community remoteness, with rate ratios ranging from 0.9 to 1.2 (Table 4; Fig. 3).
Age-standardized mortality rate ratios (per 100,000 population) of people who died of an acute toxicity in 2016 or 2017 by community remoteness and by sex. Rate ratios were calculated using the easily accessible area category as the reference category, which is represented by the red dashed line in the figure. Error bars display 95% confidence intervals. If the error bar crosses the red dotted line, then that category is not significantly different than the reference category
Neighbourhood-Level Indicators of Deprivation
There was variation in the distribution of people who died of acute toxicity across neighbourhood-level indicators of deprivation (Table 2) and when analysed by ASMR (Table 5). The proportion of people who died ranged from 7.2% in neighbourhoods of low residential instability (quintile 1) to 29.1% in neighbourhoods with the highest levels of residential instability (quintile 5). There were 7.2 to 12.4 more deaths per 100,000 population (2.3 to 3.2 times higher rates) in neighbourhoods with the highest levels of residential instability compared to the lowest (quintiles 4 and 5 versus quintile 1) (Fig. 4; Table 5). A similar pattern in residential instability was observed for both females and males, with higher rates observed among males.
Age-standardized mortality rate ratios (per 100,000 population) of people who died of an acute toxicity in 2016 or 2017 by neighbourhood-level indicators of deprivation and by sex. Rate ratios were calculated using quintile 1 of each dimension as the reference category, which is represented by the red dashed line in the figure. Error bars display 95% confidence intervals. If the error bar crosses the red dotted line, then that category is not significantly different than the reference category
Neighbourhoods with the lowest levels of economic dependency had the highest proportion of people who died of acute toxicity (quintile 1, 17.6%) (Table 2), while the highest ASMR occurred in neighbourhoods with the highest economic dependency (quintile 5, 13.4 per 100,000 population). Higher ASMRs were observed in neighbourhoods with higher levels of economic dependency; however, this pattern was less pronounced than the pattern observed for the residential instability dimension (Table 5; Fig. 4). Again, this pattern was similar for both females and males, with rates ranging from 5.3 and 12.9 per 100,000 population in the neighbourhoods with the lowest economic dependency to 8.5 and 18.5 per 100,000 population in the neighbourhoods with the highest economic dependency for females and males, respectively.
While those living in neighbourhoods with the highest ethno-cultural composition concentrations had the highest proportion of people who died of acute toxicity (quintile 4 and quintile 5, 18.5%), the highest ASMRs occurred in neighbourhoods with a moderate concentration of ethno-cultural composition (quintile 3, 13.0 per 100,000 population). This rate was significantly higher than the ASMR in neighbourhoods with the lowest concentration of ethno-cultural composition (RR, 1.8; 95% CI, 1.6, 2.0) (Table 5; Fig. 4). This pattern remained the same with a rate of 18.3 per 100,000 population for males (RR, 1.9; 95% CI, 1.7, 2.2) and a rate of 7.9 for females (RR, 1.5; 95% CI, 1.2, 1.8) residing in neighbourhoods with a moderate concentration of ethno-cultural composition (quintile 3) (Table 5; Fig. 4).
Lastly, the greatest proportion of people who died resided in neighbourhoods with the highest levels of situational vulnerability (quintile 5, 28.2%) (Table 2). ASMRs increased gradually from neighbourhoods with low (6.8 per 100,000 population) to high (19.2 per 100,000 population) situational vulnerability, with 2.8 times higher rates in quintile 5 versus 1 (95% CI, 2.5, 3.1) (Table 5; Fig. 4). This pattern of increasing ASMRs with increasing levels of situational vulnerability was observed in both females and males (Table 5; Fig. 4).
Discussion
This study reveals several critical findings on the area-level characteristics of people who died due to substance-related acute toxicity in Canada in 2016 and 2017. First, ASMRs were highest among those living in communities with populations between 100,000 to 499,999 residents and 500,000 to 1,499,999 residents. Notably, rates among residents of rural communities (outside of CMAs and CAs with weak or no metropolitan influence) were significantly higher than those in the largest urban communities (populations over 1,500,000 residents). Second, while rates were highest in accessible areas, the second highest rates occurred in very remote areas. These findings demonstrate a pattern of geographic variation in ATDs, where disproportionate rates occurred in communities outside of the largest urban centres and outside of very accessible areas.
While both national-level information (Blair & Siddiqi, 2022) and provincial reports (Public Health Ontario (PHO), 2019; BC Coroners Service, 2017; Alberta Health, 2019; Manitoba Health, 2017) from Canada have shown that the prevalence of illicit substance use as well as ATDs is higher in larger urban centres, death rates have risen recently in mid-sized urban communities and rural areas (Gomes et al., 2021; Public Health Ontario (PHO), 2019; BC Coroners Service, 2017; Alberta Health, 2019; Manitoba Health, 2017; Friesen et al., 2021), and the likelihood of fatal acute toxicity was elevated in rural areas compared to urban centres in British Columbia (Hu et al., 2022). National-level studies conducted in the USA suggest that the largest increases in substance-related mortality since 1999 have occurred in rural areas, with deaths approaching rates observed in urban areas (Brady et al., 2017; Keyes et al., 2014; Mack et al., 2017). Increasing rates in relatively rural and remote communities may be attributable to geographic barriers, health care access and utilization and historical and structural determinants (Bardwell & Lappalainen, 2021). The precise reasons for the geographic variation observed in this present study are unclear and require further investigation, including an analysis of the types of substances involved in deaths across geographic areas. The impact of health care services availability and access on substance use and related harms in rural/remote communities is another area warranting further investigation. Such analyses should consider access not only to substance use care, but to other health services such as specialized care for chronic pain and mental health. In addition, virtual health care has recently expanded in many sectors across Canada, initially in response to the COVID-19 pandemic. Expanding access to virtual services and supports could serve as one mechanism to support rural and remote communities, but further evaluation of the quality and impact of these services in the context of substance use and related harms is needed.
The analysis of neighbourhood-level indicators of deprivation revealed that in general, the highest mortality rates were observed in neighbourhoods with the highest levels of deprivation, including high residential instability, economic dependency and situational vulnerability. Our results are consistent with previous studies showing that acute toxicity hospitalizations and deaths tend to cluster in neighbourhoods with higher levels of deprivation, including areas with overrepresentation of people with lower income, educational attainment and employment (Alsabbagh et al., 2022; Altekruse et al., 2020; Barboza et al., 2022; Bozorgi et al., 2021; Bradford & Bradford, 2020; Shiels et al., 2019; Ye et al., 2018). Moreover, the effects of criminalization, stigmatization and poor access to resources and treatments have been well documented to disproportionately affect marginalized populations (Park et al., 2020). These effects may also be more commonly experienced in neighbourhoods with higher levels of certain measures of deprivation and may contribute to the high rates of ATDs observed in those neighbourhoods. In addition, the distribution of ATDs was observed to be the highest in neighbourhoods with moderate ethno-cultural composition. Prior research has found that opioid poisoning hospitalization rates are lower among visible minority groups (excluding Indigenous populations) (Carrière et al., 2018), but there is limited information available beyond this to understand potential ethno-cultural protective or risk factors on acute toxicity mortality in Canada. Recent studies from the USA indicate that the incidence of substance-related harms is increasing in Black communities (Althoff et al., 2020; Forati et al., 2021; Hedegaard & Spencer, 2021; Lippold & Ali, 2020). A study focused on qualitatively understanding the experience of substance use among Black women at high risk of HIV found that structural barriers such as housing instability, lack of employment and racial and gender discrimination led to increased substance misuse (Nydegger & Claborn, 2020). Importantly, living in stable neighbourhoods with adequate access to healthcare was associated with lower ATD rates in Black and Hispanic communities (Forati et al., 2021). Better collection of race and ethnicity data in Canada, as well as community engagement and qualitative research, may enhance our understanding of observed disparities across populations and support community-informed approaches.
Similar trends were observed for both males and females across the area-level characteristics presented in this paper. Males consistently had higher mortality rates across community population sizes, levels of community remoteness and all CIMD dimensions and quintiles. These findings align with prior research on the relationship between sex and substance-related harms, in which males account for the vast majority of acute toxicity events (Altekruse et al., 2020; Brady et al., 2017; Jiang et al., 2018; Pawer et al., 2021).
This study contributes novel, national-level evidence on the area-level characteristics of acute toxicity mortality in Canada during an important time period in this public health crisis. First, this analysis may serve as a baseline that future studies may be compared against as the study period (January 1, 2016, and December 31, 2017) is prior to (i) the introduction of many policies, programs, and interventions aimed at decreasing substance-related harms, particularly among the vulnerable and at-risk populations identified in this study; (ii) changes in available substances and an increase in the toxicity of the illicit drug supply, including the increase in acute-toxicity deaths that have involved fentanyl and analogues; and (iii) the COVID-19 pandemic, which saw a significant reduction in the availability of, and accessibility to, evidence-based local interventions, and changes in behavioural patterns of substance use (e.g. using alone). Second, our findings were strengthened by the use of two different variables to measure urban–rural variation in mortality rates through community population size and community remoteness. Although differences were small compared to the largest and most accessible communities, we were able to uncover high mortality rates in both rural (weak/no MIZ) and very remote areas. Third, our analysis demonstrates that the context surrounding ATDs is complex and multi-dimensional. Previous studies that have used a single indicator of socioeconomic status have found that the highest rates for all opioid-related outcomes (i.e. hospitalizations, emergency department visits and mortality) occurred in neighbourhoods with the lowest levels of income (Alsabbagh et al., 2022; Altekruse et al., 2020; Kariisa et al., 2022; Young et al., 2022). However, multi-dimensional measures of deprivation may allow for a more accurate investigation into intersecting inequalities. For example, our study found that the largest gaps occurred between the neighbourhoods with the highest compared to the lowest levels of residential instability and situational vulnerability. Residential instability captures low social connectedness and fluctuations in a neighbourhood’s population such as living alone, marital status, frequent moving and overcrowding, while situational vulnerability encompasses socio-demographic conditions including education, housing burden and the proportion of the population identifying as Indigenous (Statistics Canada, 2019). While our study did not directly measure mortality rates in Indigenous populations, other published studies have reported disproportionate ATD rates in Indigenous communities across Canada (Carrière et al., 2018; Firestone et al., 2015; Lavalley et al., 2018; Ponicki et al., 2018). The intergenerational effects of colonization, the residential school system and other historical, political, social and economic conditions have adversely affected the Indigenous population in Canada and may directly or indirectly contribute to higher substance-related ATD rates (PHN, 2018; Loppie & Wien, 2022). Moreover, constructing and utilizing area-based measures of Indigenous health and wellbeing that are culturally specific and relevant and that acknowledge structures of colonialism and racism may help us better understand existing inequities in this population (Fu et al., 2015).
The findings in this report are subject to several limitations. First, information collected from coroner and medical examiner charts is used to support death investigations and not for research purposes, and therefore, information abstracted into the study database was not always consistently available across individual files and regional offices. The provinces of British Columbia and Quebec had higher levels of missing postal code of residence data in the national chart review study due to data collection limitations. Cases where both the postal code and municipality of residence were not available could not be linked with the PCCF + , RI and CIMD and therefore were excluded from this analysis. Additionally, as with other ecological studies, area-based characteristics derived at the neighbourhood- or municipal-level are subject to certain biases, and findings do not apply to every individual within a neighbourhood or municipality. We did not investigate whether the relationships observed between mortality rates and community size, community remoteness and deprivation indexes are being influenced by other variables, nor did we explore interactions between measures outside of sex. Future multivariable analyses may address this gap. Moreover, while our study captures an important time period and provides a baseline where there was no national evidence previously available, further research is needed to investigate whether area-level characteristics have changed over time.
Conclusion
This study reveals that communities of all sizes, levels of remoteness and levels of deprivation have been affected by substance-related acute toxicity mortality in Canada. However, our findings underscore the disproportionate number of people dying due to substance-related acute toxicity in mid-size urban communities and neighbourhoods with high levels of deprivation. Recognizing continued increases in the number of people dying in Canada through 2022 (SAC, 2023), social and structural inequities may be exacerbating these increases, particularly in areas outside of large urban centres and in neighbourhoods with higher levels of deprivation. Evidence to better understand the circumstances surrounding these deaths and how communities are disproportionately affected can inform programs and policies aimed at reducing substance-related ATDs across Canada. These findings highlight the need for equity-focused public health responses to address the upstream drivers of substance-related ATDs, as well as further research on the factors that contribute to the disproportionate substance-related ATD rates observed.
Data availability
The national chart review of coroner and medical examiner files dataset generated and analysed for the current study are not publicly available due to provisions in the data use agreements with provincial and territorial data providers.
References
Alberta Health. (2019). Opioid-related deaths in Alberta in 2017: review of medical examiner data [PDF format]. Edmonton: Alberta Health. [cited 2022 Jul 18]. Available from: https://open.alberta.ca/dataset/f9912915-bd4f-4b57–93bf-2a963cb99038/resource/a2857fb6–6663–491c-b9df-686e348bb456/download/070519-me-chart-review-final.pdf
Alsabbagh, M. W., Cooke, M., Elliott, S. J., Chang, F., Shah, N. U., & Ghobrial, M. (2022). Stepping up to the Canadian opioid crisis: a longitudinal analysis of the correlation between socioeconomic status and population rates of opioid-related mortality, hospitalization and emergency department visits (2000–2017). Health promotion and chronic disease prevention in Canada research, policy and practice, 42(6), 229–237. https://doi.org/10.24095/hpcdp.42.6.01
Altekruse, S. F., Cosgrove, C. M., Altekruse, W. C., Jenkins, R. A., & Blanco, C. (2020). Socioeconomic risk factors for fatal opioid overdoses in the United States: Findings from the mortality disparities in American communities study (MDAC). PLoS ONE, 15(1), e0227966. https://doi.org/10.1371/journal.pone.0227966
Althoff, K. N., Leifheit, K. M., Park, J. N., Chandran, A., & Sherman, S. G. (2020). Opioid-related overdose mortality in the era of fentanyl: Monitoring a shifting epidemic by person, place, and time. Drug and Alcohol Dependence, 216, 108321. https://doi.org/10.1016/j.drugalcdep.2020.108321
Amaro, H., Sanchez, M., Bautista, T., & Cox, R. (2021). Social vulnerabilities for substance use: Stressors, socially toxic environments, and discrimination and racism. Neuropharmacology, 188, 108518. https://doi.org/10.1016/j.neuropharm.2021.108518
Barboza, G., Angulski, K., Hines, L., & Brown, P. (2022). Variability in opioid-related drug overdoses, social distancing, and area-level deprivation during the COVID-19 pandemic: A Bayesian spatiotemporal analysis. Journal of Urban Health, 99(5), 873–886. https://doi.org/10.1007/s11524-022-00675-x
Bardwell, G., & Lappalainen, L. (2021). The need to prioritize research, policy, and practice to address the overdose epidemic in smaller settings in Canada. Canadian Journal of Public Health, 112(4), 733–736. https://doi.org/10.17269/s41997-021-00504-9
Blair, A., & Siddiqi, A. (2022). The social determinants of substance use associated with deaths of despair: individual risks and population impacts. Preventive Medicine, 107327–107327. https://doi.org/10.1016/j.ypmed.2022.107327
Bozorgi, P., Porter, D. E., Eberth, J. M., Eidson, J. P., & Karami, A. (2021). The leading neighborhood-level predictors of drug overdose: A mixed machine learning and spatial approach. Drug and Alcohol Dependence, 229, 109143. https://doi.org/10.1016/j.drugalcdep.2021.109143
Bradford, A. C., & Bradford, W. D. (2020). The effect of evictions on accidental drug and alcohol mortality. Health Services Research, 55(1), 9–17. https://doi.org/10.1111/1475-6773.13256
Brady, J. E., Giglio, R., Keyes, K. M., DiMaggio, C., & Li, G. (2017). Risk markers for fatal and non-fatal prescription drug overdose: A meta-analysis. Injury Epidemiology, 4(1), 1–24. https://doi.org/10.1186/s40621-017-0118-7
British Columbia Coroners Service. Statistical reports into BC fatalities: illicit drug overdose deaths in BC [PDF format]. Burnaby (BC): BC Coroners Service. 2017. [cited 2022 Jul 18]. Available from: http://www2.gov.bc.ca/assets/gov/public-safety-and-emergency-services/death-investigation/statistical/illicit-drug.pdf
Carrière, G., Garner, R., & Sanmartin, C. (2018). Social and economic characteristics of those experiencing hospitalizations due to opioid poisonings. Health Reports, 29(10), 23–28.
Cohen, A., Vakharia, S. P., Netherland, J., & Frederique, K. (2022). How the war on drugs impacts social determinants of health beyond the criminal legal system. Annals of Medicine, 54(1), 2024–2038. https://doi.org/10.1080/07853890.2022.2100926
Firestone, M., Tyndall, M., & Fischer, B. (2015). Substance use and related harms among Aboriginal people in Canada: A comprehensive review. Journal of Health Care for the Poor and Underserved, 26(4), 1110–1131. https://doi.org/10.1353/hpu.2015.0108
Fischer, B., Pang, M., & Tyndall, M. (2019). The opioid death crisis in Canada: Crucial lessons for public health. The Lancet Public Health, 4(2), e81–e82. https://doi.org/10.1016/S2468-2667(18)30232-9
Forati, A. M., Ghose, R., & Mantsch, J. R. (2021). Examining opioid overdose deaths across communities defined by racial composition: A multiscale geographically weighted regression approach. Journal of Urban Health, 98(4), 551–562. https://doi.org/10.1007/s11524-021-00554-x
Friesen, E. L., Kurdyak, P. A., Gomes, T., Kolla, G., Leece, P., Zhu, L., . . . Jüni, P. (2021). The impact of the COVID-19 pandemic on opioid-related harm in ontario. Science Briefs of the Ontario COVID-19 Science Advisory Table, 2(42). https://doi.org/10.47326/ocsat.2021.02.42.1.0
Fu, M., Exeter, D. J., & Anderson, A. (2015). “So, is that your ‘relative’ or mine?” A political-ecological critique of census-based area deprivation indices. Social Science & Medicine, 142, 27–36. https://doi.org/10.1016/j.socscimed.2015.07.036
Galea, S., & Vlahov, D. (2002). Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Reports (Washington, D.C.: 1974), 117(Suppl 1), 135–45.
Gomes, T., Kitchen, S. A., & Murray, R. (2021). Measuring the burden of opioid-related mortality in Ontario, Canada, during the COVID-19 pandemic. JAMA Network Open, 4(5), e2112865–e2112865. https://doi.org/10.1001/jamanetworkopen.2021.12865
Hedegaard, H., & Spencer, M. R. (2021). Urban–rural differences in drug overdose deaths rates, 1999–2019. National Centre for Health Statistics, Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/nchs/data/databriefs/db403-H.pdf
Hollingsworth, A., Ruhm, C. J., & Simon, K. (2017). Macroeconomic conditions and opioid abuse. Journal of Health Economics, 56, 222–233. https://doi.org/10.3386/w23192
Hu, K., Klinkenberg, B., Gan, W. Q., & Slaunwhite, A. K. (2022). Spatial-temporal trends in the risk of illicit drug toxicity death in British Columbia. BMC Public Health, 22(1), 1–11. https://doi.org/10.1186/s12889-022-14586-8
Hundepool, A., Domingo-Ferrer, J., Franconi, L., Giessing, S., Lenz, R., Longhurst, J., ... & Wolf, P. (2010). Handbook on statistical disclosure control. ESSNet SDC.
Canadian Institute for Health Information (CIHI). Opioid-related harms in Canada, December 2018. Ottawa, ON: CIHI. 2018. [cited 2022 Jul 18]. Available from: https://www.cihi.ca/sites/default/files/document/opioid-related-harms-report-2018-en-web.pdf
Jiang, A., Smith, J., Rajabali, F., Zheng, A., Purssell, R., & Pike, I. (2018). Patterns in poisoning hospitalizations and deaths in British Columbia, 2008 to 2013. British Columbia Medical Journal, 60(10) 495–02. https://hdl.handle.net/2429/80426
Kariisa, M., Davis, N. L., Kumar, S., Seth, P., Mattson, C. L., Chowdhury, F., et al. (2022). Vital signs: drug overdose deaths, by selected sociodemographic and social determinants of health characteristics - 25 states and the District of Columbia, 2019–2020. MMWR Morbidity and Mortality Weekly Report, 71(29), 940–947. https://doi.org/10.15585/mmwr.mm7129e2
Keyes, K. M., Cerdá, M., Brady, J. E., Havens, J. R., & Galea, S. (2014). Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health, 104(2), e52–e59. https://doi.org/10.2105/AJPH.2013.301709
Konefal, S., Sherk, A., Maloney-Hall, B., Young, M., Kent, P., & Biggar, E. (2022). Polysubstance use poisoning deaths in Canada: an analysis of trends from 2014 to 2017 using mortality data. BMC Public Health, 22(1), 269. https://doi.org/10.1186/s12889-022-12678-z
Kurani, S., McCoy, R. G., Inselman, J., Jeffery, M. M., Chawla, S., Finney Rutten, L. J., Giblon, R., & Shah, N. D. (2020). Place, poverty and prescriptions: A cross-sectional study using Area Deprivation Index to assess opioid use and drug-poisoning mortality in the USA from 2012 to 2017. British Medical Journal Open, 10(5), e035376. https://doi.org/10.1136/bmjopen-2019-035376
Lavalley, J., Kastor, S., Valleriani, J., & McNeil, R. (2018). Reconciliation and Canada’s overdose crisis: responding to the needs of Indigenous Peoples. CMAJ : Canadian Medical Association journal= journal de l’Association medicale canadienne, 190(50), E1466–E1467. https://doi.org/10.1503/cmaj.181093
Lippold, K., & Ali, B. (2020). Racial/ethnic differences in opioid-involved overdose deaths across metropolitan and non-metropolitan areas in the United States, 1999–2017. Drug and Alcohol Dependence, 212, 108059. https://doi.org/10.1016/j.drugalcdep.2020.108059
Loppie, C., & Wien, F. (2022). Understanding Indigenous health inequalities through a social determinants model. Available from : https://www.nccih.ca/495/Understanding_Indigenous_Health_Inequalities_through_a_Social_Determinants_Model.nccih?id=10373
Mack, K. A., Jones, C. M., & Ballesteros, M. F. (2017). Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas−United states. American Journal of Transplantation, 17(12), 3241–3252. https://doi.org/10.1111/ajt.14555
Manitoba Health. (2017). Surveillance of opioid misuse and overdose in Manitoba: January 1-March 31, 2017 (Manitoba Health, Seniors and Active Living epi-report [PDF format]. Winnipeg: Government of Manitoba. [cited 2022 Jul 18]. Available from: https://www.manitoba.ca/health/publichealth/surveillance/docs/q1_opioid.pdf
Nydegger, L. A., & Claborn, K. R. (2020). Exploring patterns of substance use among highly vulnerable Black women at-risk for HIV through a syndemics framework: A qualitative study. PLoS ONE, 15(7), e0236247. https://doi.org/10.1371/journal.pone.0236247
Orpana, H. M., Lang, J. J., George, D., & Halverson, J. (2019). At-a-glance - the impact of poisoning-related mortality on life expectancy at birth in Canada, 2000 to 2016. Aperçu - Incidence de la mortalité par intoxication sur l’espérance de vie à la naissance au Canada (2000–2016). Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, 39(2), 56–60. https://doi.org/10.24095/hpcdp.39.2.03
Pampalon, R., Hamel, D., & Gamache, P. (2009). A comparison of individual and area-based socio-economic data for monitoring social inequalities in health. Health Reports, 20(4), 85–94.
Pan-Canadian Public Health Network (PHN). (2018). Key health inequalities in Canada: a national portrait. Ottawa: Public Health Agency of Canada. Available from: https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/science-research/key-health-inequalities-canada-national-portrait-executive-summary/key_health_inequalities_full_report-eng.pdf
Park, J. N., Rouhani, S., Beletsky, L., Vincent, L., Saloner, B., & Sherman, S. G. (2020). Situating the continuum of overdose risk in the social determinants of health: A new conceptual framework. The Milbank Quarterly, 98(3), 700–746. https://doi.org/10.1111/1468-0009.12470
Pawer, S., Rajabali, F., Zheng, A., Pike, I., Purssell, R., Zargaran, A., et al. (2021). Socioeconomic factors and substances involved in poisoning-related emergency department visits in British Columbia, Canada. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, 41(7–8), 211–221. https://doi.org/10.24095/hpcdp.41.7/8.02
Pear, V. A., Ponicki, W. R., Gaidus, A., Keyes, K. M., Martins, S. S., Fink, D. S., et al. (2019). Urban-rural variation in the socioeconomic determinants of opioid overdose. Drug and Alcohol Dependence, 195, 66–73. https://doi.org/10.1016/j.drugalcdep.2018.11.024
Ponicki, W. R., Henderson, J. A., Gaidus, A., Gruenewald, P. J., Lee, J. P., Moore, R. S., et al. (2018). Spatial epidemiology of alcohol‐and drug‐related health problems among northern plains American Indians: Nebraska and South Dakota, 2007 to 2012. Alcoholism: Clinical and Experimental Research, 42(3), 578–588. https://doi.org/10.1111/acer.13580
Public Health Agency of Canada (PHAC). (2022). Substance-related acute toxicity deaths in Canada from 2016 to 2017: a review of coroner and medical examiner files. Ottawa: Public Health Agency of Canada; Accessible at: https://www.canada.ca/en/health-canada/services/opioids/data-surveillance-research/substance-related-acute-toxicity-deaths-canada-2016-2017-review-coroner-medical-examiner-files.html
Public Health Ontario (PHO). (2019). Office of the Chief Coroner; Ontario Forensic Pathology Service; Ontario Drug Policy Research Network. Opioid mortality surveillance report: Analysis of opioid-related deaths in Ontario July 2017-June 2018 [PDF format]. Toronto: Public Health Ontario. [cited 2022 Jul 18]. Available from: https://www.publichealthontario.ca/-/media/documents/O/2019/opioid-mortality-surveillance-report.pdf
Rotondo, J., VanSteelandt, A., Kouyoumdjian, F., Bowes, M. J., Kakkar, T., Jones, G., … & Rees, E. E. (2023). Substance-related acute toxicity deaths in Canada from 2016 to 2017: a protocol for a retrospective chart review study of coroner and medical examiner files. JMIR Preprints. https://preprints.jmir.org/preprint/49981
Shiels, M. S., de González, A. B., Best, A. F., Chen, Y., Chernyavskiy, P., Hartge, P., et al. (2019). Premature mortality from all causes and drug poisonings in the USA according to socioeconomic status and rurality: An analysis of death certificate data by county from 2000–15. The Lancet Public Health, 4(2), e97–e106. https://doi.org/10.1016/S2468-2667(18)30208-1
Special Advisory Committee on the Epidemic of Opioid Overdoses (SAC). Homelessness and substance-related acute toxicity deaths: a descriptive analysis of a national chart review study of coroner and medical examiner data. Ottawa: Public Health Agency of Canada; June 2022. Available from: https://www.canada.ca/en/health-canada/services/opioids/data-surveillance-research/homelessness-substance-related-acute-toxicity-deaths.html
Special Advisory Committee on the Epidemic of Opioid Overdoses (SAC). Opioid- and stimulant-related harms in Canada [Internet]. Ottawa, ON: Public Health Agency of Canada. September 2023. Available from: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
Spencer, M. R., Garnett, M. F., & Miniño, A. M. (2022). Urban–rural differences in drug overdose death rates, 2020. NCHS Data Brief, National Center for Health Statistics. https://doi.org/10.15620/cdc:118601.
Statistics Canada. (2016). Statistical Area Classification - variant of SGC 2016. Ottawa: Statistics Canada. Available from: https://www23.statcan.gc.ca/imdb/p3VD.pl?Function=getVD&TVD=314312.
Statistics Canada. (2019). The Canadian Index of Multiple Deprivation. Ottawa (ON): StatCan. [cited 2022 Jul 18]. Available from: https://www150.statcan.gc.ca/n1/en/catalogue/45200001
Statistics Canada. (2021a). Postal CodeOM Conversion File Plus (PCCF+). Ottawa (ON): StatCan. [cited 2022 Jul 18]. Available from: https://www150.statcan.gc.ca/n1/en/catalogue/82F0086X
Statistics Canada. (2021b). Index of Remoteness. Ottawa (ON): StatCan. [cited 2022 Jul 18]. Available from: https://www150.statcan.gc.ca/n1/pub/17-26-0001/172600012020001-eng.htm
Subedi, R., Roshanafshar, S., & Greenberg, T. L. (2020). Developing meaningful categories for distinguishing levels of remoteness in Canada. Ottawa: Statistics Canada. Available from: https://epe.lac-bac.gc.ca/100/201/301/weekly_acquisitions_list-ef/2020/20-33/publications.gc.ca/collections/collection_2020/statcan/11-633-x/11-633-x2020002-eng.pdf
Tan, S. H., & Tan, S. B. (2010). The correct interpretation of confidence intervals. Proceedings of Singapore Healthcare, 19(3), 276–278.
Thomas, Y. F. (2007). The social epidemiology of drug abuse. American Journal of Preventive Medicine, 32(6), S141–S146. https://doi.org/10.1016/j.amepre.2007.03.007
Thompson, T., Rotondo, J., Enns, A., Leason, J., Halverson, J., Huyer, D., Kuo, M., Lapointe, L., May-Hadford, J., & Orpana, H. (2023). Exploring the contextual risk factors and characteristics of individuals who died from the acute toxic effects of opioids and other illegal substances: listening to the coroner and medical examiner voice. Exploration des facteurs de risque contextuels et des caractéristiques des personnes décédées des effets toxiques aigus d’opioïdes et d’autres substances illégales : prise en compte de l’avis des coroners et des médecins légistes. Health promotion and chronic disease prevention in Canada : research, policy and practice, 43(2), 51–61. https://doi.org/10.24095/hpcdp.43.2.01
Ye, X., Sutherland, J., Henry, B., Tyndall, M., & Kendall, P. R. W. (2018). At-a-glance - impact of drug overdose-related deaths on life expectancy at birth in British Columbia. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, 38(6), 248–251. https://doi.org/10.24095/hpcdp.38.6.05
Young, S., Kolla, G., McCormack, D., Campbell, T., Leece, P., Strike, C., et al. (2022). Characterizing safer supply prescribing of immediate release hydromorphone for individuals with opioid use disorder across Ontario. Canada. International Journal of Drug Policy, 102, 103601. https://doi.org/10.1016/j.drugpo.2022.103601
Acknowledgements
We would like to acknowledge our collaborators at the offices of chief coroners and chief medical examiners across Canada for providing access to their death investigation files and the co-investigator team Erin Rees, Matthew Bowes, Songul Bozat-Emre, Jessica Halverson, Dirk Huyer, Beth Jackson, Graham Jones, Jennifer Leason, and Regan Murray for their contributions to developing the national chart review study on drug and alcohol-related drug toxicity deaths. Opinions and conclusions in this report are the authors’ own and are not endorsed or approved by data providers or funders.
Funding
Open access funding provided by Public Health Agency of Canada library. This study was funded by the Public Health Agency of Canada.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data preparation, manipulation and analysis were performed by Richelle Baddeliyanage and Aganeta Enns. The first draft of the manuscript was written by Richelle Baddeliyanage, and all authors commented on previous versions of the manuscript. All authors read, critically reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study was conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments. This study was reviewed and approved by the Public Health Agency of Canada Research Ethics Board, the University of Manitoba Health Research Ethics Board, and Newfoundland and Labrador Health Research Ethics Board.
Competing interests
The authors declare no competing interests.
Disclaimer.
This report is based on data and information compiled and provided by the offices of chief coroners and chief medical examiners across Canada. However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of the data providers.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baddeliyanage, R., Enns, A., Vansteelandt, A. et al. Substance-Related Acute Toxicity Deaths by Area-Based Characteristics: A Descriptive Analysis of a National Chart Review Study of Coroner and Medical Examiner Data. Int J Ment Health Addiction (2024). https://doi.org/10.1007/s11469-024-01259-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-024-01259-3