Abstract
Type 1 diabetes (T1D) is characterized by the destruction of pancreatic β-cells. Several observations have renewed the interest in β-cell RNA sensors and editors. Here, we report that N6-methyladenosine (m6A) is an adaptive β-cell safeguard mechanism that controls the amplitude and duration of the antiviral innate immune response at T1D onset. m6A writer methyltransferase 3 (METTL3) levels increase drastically in β-cells at T1D onset but rapidly decline with disease progression. m6A sequencing revealed the m6A hypermethylation of several key innate immune mediators, including OAS1, OAS2, OAS3 and ADAR1 in human islets and EndoC-βH1 cells at T1D onset. METTL3 silencing enhanced 2′-5′-oligoadenylate synthetase levels by increasing its mRNA stability. Consistently, in vivo gene therapy to prolong Mettl3 overexpression specifically in β-cells delayed diabetes progression in the non-obese diabetic mouse model of T1D. Mechanistically, the accumulation of reactive oxygen species blocked upregulation of METTL3 in response to cytokines, while physiological levels of nitric oxide enhanced METTL3 levels and activity. Furthermore, we report that the cysteines in position C276 and C326 in the zinc finger domains of the METTL3 protein are sensitive to S-nitrosylation and are important to the METTL3-mediated regulation of oligoadenylate synthase mRNA stability in human β-cells. Collectively, we report that m6A regulates the innate immune response at the β-cell level during the onset of T1D in humans.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
m6A-seq and RNA-seq data in human islets and EndoC-βH1 cells have been deposited with the National Center for Biotechnology Information Gene Expression Omnibus under accession code GSE228267. RNA-seq in NOD mouse β- and non-β-cells sorted by fluorescence-activated cell sorting have been deposited under the accession code GSE228219. RNA-seq data in EndoC-βH1 cells harbouring OAS overexpression have been deposited under the accession code GSE244273. Mass spectrometry data on METTL3 SNO have been deposited with Mass Spectrometry Interactive Visual Environment (MassIVE) under the accession code MSV000091547. Source data are provided with this paper. All other data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Crowl, J. T., Gray, E. E., Pestal, K., Volkman, H. E. & Stetson, D. B. Intracellular nucleic acid detection in autoimmunity. Annu. Rev. Immunol. 35, 313–336 (2017).
Lang, K. S., Burow, A., Kurrer, M., Lang, P. A. & Recher, M. The role of the innate immune response in autoimmune disease. J. Autoimmun. 29, 206–212 (2007).
Kallionpaa, H. et al. Innate immune activity is detected prior to seroconversion in children with HLA-conferred type 1 diabetes susceptibility. Diabetes 63, 2402–2414 (2014).
Carry, P. M. et al. Changes in the coexpression of innate immunity genes during persistent islet autoimmunity are associated with progression of islet autoimmunity: Diabetes Autoimmunity Study in the Young (DAISY). Diabetes 71, 2048–2057 (2022).
Apaolaza, P. S. et al. Islet expression of type I interferon response sensors is associated with immune infiltration and viral infection in type 1 diabetes. Sci. Adv. 7, eabd6527 (2021).
Lundberg, M., Krogvold, L., Kuric, E., Dahl-Jorgensen, K. & Skog, O. Expression of interferon-stimulated genes in insulitic pancreatic islets of patients recently diagnosed with type 1. Diabetes 65, 3104–3110 (2016).
Hornung, V., Hartmann, R., Ablasser, A. & Hopfner, K. P. OAS proteins and cGAS: unifying concepts in sensing and responding to cytosolic nucleic acids. Nat. Rev. Immunol. 14, 521–528 (2014).
Pedersen, K. et al. Genetic predisposition in the 2′-5′A pathway in the development of type 1 diabetes: potential contribution to dysregulation of innate antiviral immunity. Diabetologia 64, 1805–1815 (2021).
Field, L. L. et al. OAS1 splice site polymorphism controlling antiviral enzyme activity influences susceptibility to type 1 diabetes. Diabetes 54, 1588–1591 (2005).
Tessier, M. C. et al. Type 1 diabetes and the OAS gene cluster: association with splicing polymorphism or haplotype? J. Med. Genet. 43, 129–132 (2006).
Bonnevie-Nielsen, V., Buschard, K. & Dyrberg, T. Differential responsiveness to interferon-alpha in beta-cells and non-beta cells. Diabetes 45, 818–821 (1996).
Li, M., Zheng, D. J., Field, L. L. & Bonnevie-Nielsen, V. Murine pancreatic beta TC3 cells show greater 2′, 5′-oligoadenylate synthetase (2′5′AS) antiviral enzyme activity and apoptosis following IFN-alpha or poly(I:C) treatment than pancreatic alpha TC3 cells. Exp. Diabetes Res. 2009, 631026 (2009).
Dan, M., Zheng, D., Field, L. L. & Bonnevie-Nielsen, V. Induction and activation of antiviral enzyme 2′,5′-oligoadenylate synthetase by in vitro transcribed insulin mRNA and other cellular RNAs. Mol. Biol. Rep. 39, 7813–7822 (2012).
Zeng, C. et al. RNase L contributes to experimentally induced type 1 diabetes onset in mice. J. Endocrinol. 223, 277–287 (2014).
Frye, M., Harada, B. T., Behm, M. & He, C. RNA modifications modulate gene expression during development. Science 361, 1346–1349 (2018).
Dominissini, D. et al. Topology of the human and mouse m6A RNA methylomes revealed by m6A-seq. Nature 485, 201–206 (2012).
Meyer, K. D. et al. Comprehensive analysis of mRNA methylation reveals enrichment in 3′ UTRs and near stop codons. Cell 149, 1635–1646 (2012).
Lee, J. H. et al. Enhancer RNA m6A methylation facilitates transcriptional condensate formation and gene activation. Mol. Cell 81, 3368–3385 e3369 (2021).
Lasman, L. et al. Context-dependent functional compensation between Ythdf m6A reader proteins. Genes Dev. 34, 1373–1391 (2020).
Zou, Z., Sepich-Poore, C., Zhou, X., Wei, J. & He, C. The mechanism underlying redundant functions of the YTHDF proteins. Genome Biol. 24, 17 (2023).
Wang, P., Doxtader, K. A. & Nam, Y. Structural basis for cooperative function of Mettl3 and Mettl14 methyltransferases. Mol. Cell 63, 306–317 (2016).
Du, Y. et al. SUMOylation of the m6A-RNA methyltransferase METTL3 modulates its function. Nucleic Acids Res. 46, 5195–5208 (2018).
Sun, H. L. et al. Stabilization of ERK-phosphorylated METTL3 by USP5 increases m6A methylation. Mol. Cell 80, 633–647 e637 (2020).
Winkler, R. et al. m(6)A modification controls the innate immune response to infection by targeting type I interferons. Nat. Immunol. 20, 173–182 (2019).
Terajima, H. et al. N6-methyladenosine promotes induction of ADAR1-mediated A-to-I RNA editing to suppress aberrant antiviral innate immune responses. PLoS Biol. 19, e3001292 (2021).
Gao, Y. et al. m6A modification prevents formation of endogenous double-stranded RNAs and deleterious innate immune responses during hematopoietic development. Immunity 52, 1007–1021 e1008 (2020).
Qiu, W. et al. N6-methyladenosine RNA modification suppresses antiviral innate sensing pathways via reshaping double-stranded RNA. Nat. Commun. 12, 1582 (2021).
Makino, S. et al. Breeding of a non-obese, diabetic strain of mice. Jikken Dobutsu 29, 1–13 (1980).
De Jesus, D. F. et al. m6A mRNA methylation regulates human beta-cell biology in physiological states and in type 2 diabetes. Nat. Metab. 1, 765–774 (2019).
Prochazka, M., Serreze, D. V., Frankel, W. N. & Leiter, E. H. NOR/Lt mice: MHC-matched diabetes-resistant control strain for NOD mice. Diabetes 41, 98–106 (1992).
Carrero, J. A., Calderon, B., Towfic, F., Artyomov, M. N. & Unanue, E. R. Defining the transcriptional and cellular landscape of type 1 diabetes in the NOD mouse. PLoS ONE 8, e59701 (2013).
Smelt, M. J., Faas, M. M., de Haan, B. J. & de Vos, P. Pancreatic beta-cell purification by altering FAD and NAD(P)H metabolism. Exp. Diabetes Res 2008, 165360 (2008).
Russell, M. A. et al. HLA class II antigen processing and presentation pathway components demonstrated by transcriptome and protein analyses of islet beta-cells from donors with type 1 diabetes. Diabetes 68, 988–1001 (2019).
Sledz, P. & Jinek, M. Structural insights into the molecular mechanism of the m6A writer complex. eLife 5, e18434 (2016).
Schneider, C. A., Rasband, W. S. & Eliceiri, K. W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 9, 671–675 (2012).
Dirice, E. et al. Increased beta-cell proliferation before immune cell invasion prevents progression of type 1 diabetes. Nat. Metab. 1, 509–518 (2019).
Eisenbarth, G. S. Type I diabetes mellitus. A chronic autoimmune disease. N. Engl. J. Med. 314, 1360–1368 (1986).
Ramos-Rodriguez, M. et al. The impact of proinflammatory cytokines on the beta-cell regulatory landscape provides insights into the genetics of type 1 diabetes. Nat. Genet. 51, 1588–1595 (2019).
Eizirik, D. L. et al. The human pancreatic islet transcriptome: expression of candidate genes for type 1 diabetes and the impact of pro-inflammatory cytokines. PLoS Genet. 8, e1002552 (2012).
Benazra, M. et al. A human beta cell line with drug inducible excision of immortalizing transgenes. Mol. Metab. 4, 916–925 (2015).
York, I. A., Brehm, M. A., Zendzian, S., Towne, C. F. & Rock, K. L. Endoplasmic reticulum aminopeptidase 1 (ERAP1) trims MHC class I-presented peptides in vivo and plays an important role in immunodominance. Proc. Natl Acad. Sci. USA 103, 9202–9207 (2006).
Thomaidou, S. et al. β-Cell stress shapes CTL immune recognition of preproinsulin signal peptide by posttranscriptional regulation of endoplasmic reticulum aminopeptidase 1. Diabetes 69, 670–680 (2020).
Szymczak, F. et al. ADAR1-dependent editing regulates human β cell transcriptome diversity during inflammation. Front. Endocrinol. 13, 1058345 (2022).
Hu, S.-B. et al. ADAR1p150 prevents MDA5 and PKR activation via distinct mechanisms to avert fatal autoinflammation. Mol. Cell 83, 3869–3884.e3867 (2023).
Li, X., Chen, H. & Epstein, P. N. Metallothionein protects islets from hypoxia and extends islet graft survival by scavenging most kinds of reactive oxygen species. J. Biol. Chem. 279, 765–771 (2004).
Bensellam, M., Laybutt, D. R. & Jonas, J.-C. Emerging roles of metallothioneins in beta cell pathophysiology: beyond and above metal homeostasis and antioxidant response. Biology 10, 176 (2021).
Dor, Y., Brown, J., Martinez, O. I. & Melton, D. A. Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature 429, 41–46 (2004).
Rui, J. et al. Tet2 controls the responses of beta cells to inflammation in autoimmune diabetes. Nat. Commun. 12, 5074 (2021).
Kulkarni, A. et al. 12-Lipoxygenase governs the innate immune pathogenesis of islet inflammation and autoimmune diabetes. JCI Insight 6, e147812 (2021).
Nelson, A. S. et al. Oral therapy with colonization factor antigen I prevents development of type 1 diabetes in non-obese diabetic mice. Sci. Rep. 10, 6156 (2020).
Robinson, C. P., Yamamoto, H., Peck, A. B. & Humphreys-Beher, M. G. Genetically programmed development of salivary gland abnormalities in the NOD (nonobese diabetic)-scid mouse in the absence of detectable lymphocytic infiltration: a potential trigger for sialoadenitis of NOD mice. Clin. Immunol. Immunopathol. 79, 50–59 (1996).
Elkhateeb, E. et al. The role of mouse 2′,5′-oligoadenylate synthetase 1 paralogs. Infect. Genet. Evol. 45, 393–401 (2016).
Chen, J., Stimpson, S. E., Fernandez-Bueno, G. A. & Mathews, C. E. Mitochondrial reactive oxygen species and type 1 diabetes. Antioxid. Redox Signal 29, 1361–1372 (2018).
Kim, Y. K., Sussel, L. & Davidson, H. W. Inherent beta cell dysfunction contributes to autoimmune susceptibility. Biomolecules 11, 512 (2021).
Tersey, S. A. et al. Islet beta-cell endoplasmic reticulum stress precedes the onset of type 1 diabetes in the nonobese diabetic mouse model. Diabetes 61, 818–827 (2012).
Mallone, R. & Eizirik, D. L. Presumption of innocence for beta cells: why are they vulnerable autoimmune targets in type 1 diabetes? Diabetologia 63, 1999–2006 (2020).
Wang, X. et al. N6-methyladenosine-dependent regulation of messenger RNA stability. Nature 505, 117–120 (2014).
Rubio, R. M., Depledge, D. P., Bianco, C., Thompson, L. & Mohr, I. RNA m6A modification enzymes shape innate responses to DNA by regulating interferon beta. Genes Dev. 32, 1472–1484 (2018).
Balzano-Nogueira, L. et al. Integrative analyses of TEDDY Omics data reveal lipid metabolism abnormalities, increased intracellular ROS and heightened inflammation prior to autoimmunity for type 1 diabetes. Genome Biol. 22, 39 (2021).
Eizirik, D. L., Miani, M. & Cardozo, A. K. Signalling danger: endoplasmic reticulum stress and the unfolded protein response in pancreatic islet inflammation. Diabetologia 56, 234–241 (2013).
Sahin, G. S., Lee, H. & Engin, F. An accomplice more than a mere victim: the impact of β-cell ER stress on type 1 diabetes pathogenesis. Mol. Metab. 54, 101365 (2021).
Zhou, H. L., Premont, R. T. & Stamler, J. S. The manifold roles of protein S-nitrosylation in the life of insulin. Nat. Rev. Endocrinol. 18, 111–128 (2022).
Garban, H. J., Marquez-Garban, D. C., Pietras, R. J. & Ignarro, L. J. Rapid nitric oxide-mediated S-nitrosylation of estrogen receptor: regulation of estrogen-dependent gene transcription. Proc. Natl Acad. Sci. USA 102, 2632–2636 (2005).
Kroncke, K. D. Zinc finger proteins as molecular targets for nitric oxide-mediated gene regulation. Antioxid. Redox Signal 3, 565–575 (2001).
Huang, J. et al. Solution structure of the RNA recognition domain of METTL3–METTL14 N6-methyladenosine methyltransferase. Protein Cell 10, 272–284 (2019).
Ravassard, P. et al. A genetically engineered human pancreatic β cell line exhibiting glucose-inducible insulin secretion. J. Clin. Investig. 121, 3589–3597 (2011).
El Ouaamari, A. et al. SerpinB1 promotes pancreatic beta cell proliferation. Cell Metab. 23, 194–205 (2016).
El Ouaamari, A. et al. Compensatory islet response to insulin resistance revealed by quantitative proteomics. J. Proteome Res. 14, 3111–3122 (2015).
Dirice, E. et al. Soluble factors secreted by T cells promote beta-cell proliferation. Diabetes 63, 188–202 (2014).
De Jesus, D. F. et al. Parental metabolic syndrome epigenetically reprograms offspring hepatic lipid metabolism in mice. J. Clin. Invest. 130, 2391–2407 (2020).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Chen, S., Zhou, Y., Chen, Y. & Gu, J. fastp: an ultra-fast all-in-one FASTQ preprocessor. Bioinformatics 34, i884–i890 (2018).
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Zhang, Z. et al. RADAR: differential analysis of MeRIP-seq data with a random effect model. Genome Biol. 20, 294 (2019).
Ritchie, M. E. et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47 (2015).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Fisher, R. A. in Breakthroughs in Statistics (eds Kotz, S. & Johnson, N. L.) 66–70 (Springer, 1992).
Liao, Y., Smyth, G. K. & Shi, W. featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30, 923–930 (2014).
Bray, N. L., Pimentel, H., Melsted, P. & Pachter, L. Near-optimal probabilistic RNA-seq quantification. Nat. Biotechnol. 34, 525–527 (2016).
Soneson, C., Love, M. I. & Robinson, M. D. Differential analyses for RNA-seq: transcript-level estimates improve gene-level inferences. F1000Res 4, 1521 (2015).
Robinson, M. D. & Oshlack, A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 11, R25 (2010).
Law, C. W., Chen, Y., Shi, W. & Smyth, G. K. voom: precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol. 15, R29 (2014).
McCarthy, D. J., Campbell, K. R., Lun, A. T. & Wills, Q. F. Scater: pre-processing, quality control, normalization and visualization of single-cell RNA-seq data in R. Bioinformatics 33, 1179–1186 (2017).
Lun, A. T., Bach, K. & Marioni, J. C. Pooling across cells to normalize single-cell RNA sequencing data with many zero counts. Genome Biol. 17, 75 (2016).
Scrucca, L., Fop, M., Murphy, T. B. & Raftery, A. E. mclust 5: clustering, classification and density estimation using Gaussian finite mixture models. R. J. 8, 289–317 (2016).
Herwig, R., Hardt, C., Lienhard, M. & Kamburov, A. Analyzing and interpreting genome data at the network level with ConsensusPathDB. Nat. Protoc. 11, 1889 (2016).
Zhou, Y. et al. Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat. Commun. 10, 1523 (2019).
Saito, R. et al. A travel guide to Cytoscape plugins. Nat. Methods 9, 1069–1076 (2012).
Snel, B. et al. STRING: known and predicted protein–protein associations, integrated and transferred across organisms. Nucleic Acids Res. 33, D433–D437 (2005).
Duan, J. et al. Stochiometric quantification of the thiol redox proteome of macrophages reveals subcellular compartmentalization and susceptibility to oxidative perturbations. Redox Biol. 36, 101649 (2020).
Jumper, J. et al. Highly accurate protein structure prediction with AlphaFold. Nature 596, 583–589 (2021).
Acknowledgements
The authors thank F. Bosch (Universitat Autònoma de Barcelona) and her lab members for discussions about AAV design and in vivo administration. We thank A. Op de Beeck (ULB Center for Diabetes Research, Université Libre de Bruxelles) for helpful discussions related to viral infections. We thank E. Dirice (New York Medical College) for discussions related to co-culture of islets and splenocytes. We thank B. Kunkemoeller (Brigham and Women’s Hospital) for assistance with fluorescence-activated cell sorting analysis and E. Mandato (Dana-Farber Cancer Institute) and A. Ferreira (Brigham and Women’s Hospital) for discussions regarding site mutagenesis. The authors thank the Joslin Islet Isolation Core, Joslin Flow Cytometry Core and Joslin Bioinformatics Core (P30 DK36836). This work is supported by NIH grants R01 DK67536 (R.N.K.), UC4 DK116278 (R.N.K. and C.H.), RM1 HG008935 (C.H.) and R01 DK122160 (W.-J.Q. and R.N.K.). Portions of the mass spectrometry work were performed in the Environmental Molecular Sciences Laboratory, Pacific Northwest National Laboratory, a national scientific user facility sponsored by the Department of Energy under contract DE-AC05-76RL0 1830. R.N.K. acknowledges support from the Margaret A. Congleton Endowed Chair and C.H. is a Howard Hughes Medical Institute Investigator. D.F.D.J. acknowledges support from Mary K. Iacocca Junior Postdoctoral Fellowship, American Diabetes Association grant #7-21-PDF-140 and NIH K99 DK135927. The authors sincerely thank the families of the human islet donors.
Author information
Authors and Affiliations
Contributions
D.F.D.J. conceived the study, designed and performed experiments, analysed the data, assembled figures and wrote the manuscript. Z.Z. performed RNA-seq, m6A-seq and m6A LC–MS/MS experiments. N.K.B. and G.F. performed morphometric analyses of pancreases and assisted with animal experiments. X.L. and M.J.G. performed LC–MS/MS on SNO. S.K. performed cell culture experiments. J.W. assisted with omics data handling. J.H. performed immunohistochemistry. G.B. assisted with in vivo experiments. L.X. assisted with immune cell profiling by fluorescence-activated cell sorting. T.M.R. provided reagents. C.M. provided microarray data on T1D islets. A.C.P. provided T1D islets. M.A.A. contributed to conceptual discussions and assisted with nPOD pancreatic sections. D.L.E. contributed to conceptual discussion and shared protocols. S.D.-P. assisted with METTL3 structural modelling. A.V.P. assisted with human pseudoislet experiments. W.-J.Q. performed LC–MS/MS data analysis and contributed to conceptual discussions. C.H. contributed to conceptual discussions, designed the experiments and wrote the manuscript. R.N.K. conceived the study, designed the experiments, supervised the project and wrote the manuscript. All the authors have reviewed, commented on and edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
R.N.K is on the scientific advisory board of Novo Nordisk, Biomea and REDD. C.H. is a scientific founder and a member of the scientific advisory board of Accent Therapeutics. The remaining authors have no conflicts of interest.
Peer review
Peer review information
Nature Cell Biology thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
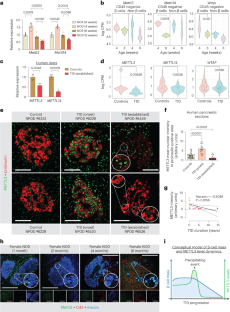
Extended Data Fig. 1 T1D pathways are upregulated in Mettl14 deficient mouse β-cells and pre-diabetic NOD β-cells show enrichment in pathways associated with Type 1 diabetes (related to Fig. 1).
a, Diagram of differentially expressed genes in Mettl14 KO β-cells compared to controls. b, Pathway enrichment analyses of genes upregulated in Mettl14 KO β-cells compared to controls (Controls, n = 4 pools, 2 animals/pool; M14KO, n = 4 pools, 4 animals/pool). c, Body weight of NOR and NOD females at 4- or 8-weeks of age (n = 6 mice/group). d, Random-fed serum glucose levels of NOR and NOD females at 4- or 8-weeks of age (n = 6 mice/group). e, Representative FACS sorting strategy to deplete CD45 positive cells, and obtain an enriched β-cell population based on size, granularity, and autofluorescence (FITC) from NOD female mice. f, Immunofluorescence staining of sorted β- and non-β-cell fractions showing insulin staining in red, glucagon in green, and somatostatin in blue (n = 3 independent experiments/group). Scale bar = 20μM. g, PCA plot of RNA-seq samples of 4- or 8-week-old FACS sorted β-cells or non-β-cells (n = 3 pools of 3 mice per pool). h, Heat-map representation of islet identity genes, showing enrichment for β cell identity genes in the β-cell fraction compared to non-β-cells. i, Heat-map of represented genes associated with Type 1 diabetes, innate immunity, and antigen processing and presentation and upregulated in pre-diabetic 8-week-old β-cells compared to 4-week-old. All samples in each panel are biologically independent. Data were expressed as means ± SEM. Heat maps represent clipped Z-scored log CPM. Statistical analyses were performed using the Benjamini-Hochberg procedure and genes were filtered for FDR<0.05 or 0.10 in ‘a’. P values of pathway enrichment analysis were calculated according to the hypergeometric test based on the number of physical entities present in both the predefined set and user-specified list of physical entities. Data in ‘a’ and ‘b’ were downloaded and reanalyzed from dataset GSE132306 (ref. 35). Source numerical data are available in source data.
Extended Data Fig. 2 scRNA-seq re-analyses of established T1D islets, upregulation of METTL3 in human β-cells at T1D onset, and Mettl3 downregulation in β-cells with T1D progression in female NOD mice (related to Fig. 1).
a-b, t-SNE representation of β-cells (a) (high insulin expression) or α-cells (b) (high glucagon expression) in control and established Type 1 diabetes (T1D) (GSE121863)40. c, Schematic representation of the Image J pipeline used to quantify the METTL3 nuclear intensity in proinsulin positive area in human pancreatic sections from the Network for Pancreatic Organ Donors with Diabetes (nPOD). d, Representative low magnification pictures of immunofluorescence staining of METTL3 (green) and Proinsulin (red) in pancreatic sections from human control and T1D onset showing a robust islet enriched upregulation of METTL3 at T1D onset. (Control, n = 9 patients; T1D Onset, n = 4 patients; established T1D, n = 7 patients). e, Representative pictures of immunofluorescence staining of Mettl3 (green), Insulin (blue), and Cd3 (red) in pancreatic sections from NOD male mice without any histological pancreatic immune cell infiltration patterns (n = 3 mice/group). Scale bar = 100μM. Source numerical data are available in source data.
Extended Data Fig. 3 m6A landscape analyses of human islets treated with IL-1β and IFN-α reveal differential methylation of class I MHC-mediated antigen processing and presentation genes (related to Fig. 3).
a, Venn diagram representation of the m6A hypermethylated, m6A hypomethylated, upregulated, or downregulated genes in human islets treated with IL-1β and IFN-α compared to PBS. Statistical analyses were performed using the Benjamini-Hochberg procedure and genes were filtered for FDR<0.05. b-e, Pathway enrichment analyses of m6A hypermethylated and upregulated (a), m6A hypermethylated and downregulated (c), m6A hypomethylated and upregulated (d), or m6A hypomethylated and downregulated genes (e) in human islets treated with IL-1β and IFN-α compared to PBS. P values were calculated according to the hypergeometric test based on the number of physical entities present in both the predefined set and user-specified list of physical entities. f, MHC class I differentially m6A methylated genes in human islets treated with IL-1β and IFN-α compared to PBS. g, Protein-protein interactions network of class I MHC-mediated antigen processing and presentation differentially m6A methylated in human islets treated with IL-1β and IFN-α compared to PBS. h-j, Coverage plots of m6A peaks ERAP1in human islets treated with IL-1β and IFN-α or PBS (h) (n = 15 biological independent samples/group), EndoC-βH1 cells treated with IL-1β and IFN-α or PBS (i) (n = 6 independent experiments/group), or human T1D and Control islets (j) (Controls, n = 20; T1D, n = 7 biological independent samples). Plotted coverages are the median of the n replicates presented. All samples in each panel are biologically independent. P values of pathway enrichment analysis were calculated according to the hypergeometric test based on the number of physical entities present in both the predefined set and user-specified list of physical entities. Source numerical data are available in source data.
Extended Data Fig. 4 Human islets and EndoC-βH1 cells present an extensive overlap in the innate immune response to IL-1β and IFN-α (related to Figs. 3 and 4).
a, Diagram representation of the upregulated (red), downregulated (blue), and unchanged genes (black) in EndoC-βH1 cells treated with IL-1β and IFN-α compared to PBS. Statistical analyses were performed using the Benjamini-Hochberg procedure and genes were filtered for FDR<0.05. b, Pathway enrichment analyses of upregulated and downregulated genes in EndoC-βH1 cells treated with IL-1β and IFN-α compared to PBS. c, Venn diagram representation of the commonly upregulated (red), downregulated (blue), and unchanged genes (black) of the intersected genes in EndoC-βH1 and human islets cells treated with IL-1β and IFN-α compared to PBS. Statistical analyses were performed using the Benjamini-Hochberg procedure and genes were filtered for FDR<0.05. d, Pathway enrichment analyses of commonly upregulated and downregulated genes in human islets and EndoC-βH1 cells treated with IL-1β and IFN-α compared to PBS. e-f, Volcano-plot representation of differentially expressed genes in human islets (e) and EndoC-βH1 cells (f) treated with IL-1β and IFN-α compared to PBS. Innate immune genes are depicted in red and show a near absolute overlap between human islets and EndoC-βH1 cells. Human islets: n = 15 biologically independent samples. EndoC-βH1 cells: n = 6 independent experiments/group. Statistical analyses were performed using the Benjamini-Hochberg procedure. P values of pathway enrichment analysis were calculated according to the hypergeometric test based on the number of physical entities present in both the predefined set and user-specified list of physical entities. Source numerical data are available in source data.
Extended Data Fig. 5 OAS upregulation is more prominent in β-cells, and METTL3 silencing leads to the downregulation of ADAR1 p150 isoform in β-cells (related to Fig. 4).
a, Metagene of m6A enriched peaks in PBS (blue) or IL-1β + IFN-α-treated (red) EndoC-βH1 cells. b, Enrichment for known m6A consensus motif RRACH. c, Histogram of the distribution of differential m6A loci log2 fold changes from IL-1β plus IFN-α-treated versus PBS in EndoC-βH1 cells. d, m6A-IP-qPCR showing increased m6A in OAS1, OAS2, and OAS3 in IL-1β + IFN-α-treated EndoC-βH1 cells compared to PBS (Basal) (n = 3 independent experiments/group). e-g, Western-blot analyses of indicated proteins in EndoC-βH1 cells and 266-6 cells (e), or PANC-1 (f), or αTC-6 (g) treated with PBS or IL1-β plus IFN-α for 24h (n = 3 independent experiments/group). h, Western-blot analyses of indicated proteins EndoC-βH1 cells harboring METTL3 silencing or Scramble and treated with PBS or IL1-β plus IFN-α (n = 3 independent experiments/group). Same experiment of Fig. 4h, with same loading control. i, Protein quantification of indicated proteins related to (h). j, qRT-PCR analyses of YTHDF genes after IL-1β plus IFN-α stimulation in scramble, YTHDF1, YTHDF2, or YTHDF3 KD EndoC-βH1 cells (n = 4 independent experiments/group). All samples in each panel are biologically independent. Data were expressed as means ± SEM. Statistical analysis was performed by two-tailed unpaired t-test. Source numerical data and unprocessed gel images are available in source data.
Extended Data Fig. 6 m6A landscape analyses of established T1D reveal differential methylation of master regulators of β-cell identity and function (related to Fig. 6).
a, Venn diagram representation of the m6A hypermethylated, m6A hypomethylated, upregulated, or downregulated genes in human islets from patients with established T1D or non-diabetic Controls. Statistical analyses were performed using the Benjamini-Hochberg procedure and genes were filtered for FDR<0.05. Human islets: Controls n = 20 and T1D n = 7 biologically independent samples. b-e, Pathway enrichment analyses of m6A hypermethylated and upregulated (a), m6A hypermethylated and downregulated (c), m6A hypomethylated and upregulated (d), or m6A hypomethylated and downregulated genes (e) in human islets from established T1D compared to Controls. P values of pathway enrichment analysis were calculated according to the hypergeometric test based on the number of physical entities present in both the predefined set and user-specified list of physical entities. Source numerical data are available in source data.
Extended Data Fig. 7 Mettl3 overexpression in NOD β-cells (related to Fig. 7).
a, Schematic diagram showing the vector design of AAV8 driving eGFP or Mettl3 under the control of a rat insulin promoter II. b, Representative immunofluorescence images of pancreas, white adipose tissue (WAT), muscle, liver, and intestine showing insulin (red), eGFP (green), and DAPI (blue) (n = 4 mice/group). Scale bar = 100μM.
Extended Data Fig. 8 Immune cell profiling of NOD pancreatic lymph nodes (related to Fig. 7).
a-n, Flow cytometry analyses of CD4 (a,b), CD8 (c,d), B-cells (e,f), dendritic cells (g,h), activated dendritic cells (i,j), tolerogenic dendritic cells (k,l), or th1 cells (m,n) isolated from pancreatic lymph nodes of NOD mice receiving PBS, eGFP, or Mettl3 overexpression (n = 4 mice/group). All samples in each panel are biologically independent. Data were expressed as means ± SEM. Statistical analysis was performed by One-Way ANOVA with Holm-Sidak test. Source numerical data are available in source data.
Extended Data Fig. 9 Immune cell profiling of NOD splenocytes (related to Fig. 7).
a-n, Flow cytometry analyses of CD4 (a,b), CD8 (c,d), B-cells (e,f), dendritic cells (g,h), activated dendritic cells (i,j), tolerogenic dendritic cells (k,l), or th1 cells (m,n) isolated from spleens of NOD mice receiving PBS, eGFP, or Mettl3 overexpression (n = 4 mice/group). All samples in each panel are biologically independent. Data were expressed as means ± SEM. Statistical analysis was performed by One-Way ANOVA with Holm-Sidak test. Source numerical data are available in source data.
Extended Data Fig. 10 Summary schemes of experimental approaches and METTL3 protein structural modeling (related to Fig. 8).
a, Western-blot analyses of indicated proteins in human islets cells treated with DMSO, 1μM thapsigargin, or 2μg/mL tunicamycin for 24h (n = 2 biological independent samples/group). b, Protein quantification of indicated proteins related to (a). c, Western-blot analyses of indicated proteins in EndoC-βH1 cells treated with DMSO, 25μM H2O2, or 25μM H2O2 + 5μM MG132 for 24h (n = 3 independent experiments/group). d, Protein quantification of indicated proteins related to (c). e, Summary scheme of experimental approach to measure METTL3 SNO by LC-MS/MS. f, MS/MS spectra of S-nitrosylated METTL3 peptides and the identification of cysteines C276, C294, C326, and C336 (n = 2 replicates). g, Predicted aligned error related to Fig. 8i–k. The color at position (x, y) indicates AlphaFold’s expected position error at residue x, when the predicted and true structures are aligned on residue y. h, CLUSTAL (1.2.4) multiple sequence alignment of METTL3 in represented species. i, Conceptual model of the role of METTL3 in controlling the OAS innate antiviral immune response by regulating the formation of deleterious dsRNAs and/or controlling viral response. The METTL3 response is decreased by the presence of ER stress and increased ROS levels, resulting from several potential factors such as hyperglycemia, dyslipidemia, genetic, or other environmental mediators such as pollution. Data were expressed as means ± SEM. Statistical analysis was performed by Two-Way ANOVA with Holm-Sidak test in b, and One-Way ANOVA with Holm-Sidak test in d. Source unprocessed gel images and numerical data are available in source data.
Supplementary information
Supplementary Table 1
Human islet patient information and primer sequences.
Source data
Source Data
Statistical source data for Figs. 1–8.
Source Data
Statistical source data for Extended Data Figs. 1–10.
Source Data
Unprocessed western blots for Figs. 2, 4, 5, 7 and 8 and Extended Data Figs. 5 and 10.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
F. De Jesus, D., Zhang, Z., Brown, N.K. et al. Redox regulation of m6A methyltransferase METTL3 in β-cells controls the innate immune response in type 1 diabetes. Nat Cell Biol 26, 421–437 (2024). https://doi.org/10.1038/s41556-024-01368-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41556-024-01368-0
This article is cited by
-
METTL3 restrains autoimmunity in β-cells
Nature Cell Biology (2024)



