Abstract
Background/Aims
Patients with chronic constipation (CC) exhibit symptoms and functional abnormalities upon testing, but their relationship to age and gender is unclear. We assessed age- and gender-related differences in symptoms, colon transit time, and anorectal motility, sensation, and expulsion.
Patients and Methods
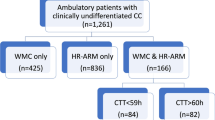
Retrospective, post hoc data analysis of patients with CC, who underwent Wireless Motility Capsule (WMC), High-Resolution Anorectal Manometry (HR-ARM), Balloon Expulsion Test (BET) and Rectal Sensory Testing (RST). Clinical assessment was made by questionnaires. Standard WMC criteria for colonic transit time (CTT) and the London classification was used for HR‐ARM analyses, and regression plots between age, gender, CTT, HR-HRM, RST and BET were calculated.
Results
We studied 75 women and 91 men. Abdominal pain, infrequent defecation, incomplete evacuation, defecatory straining, and multiple motility and anorectal function abnormalities were common. Abdominal pain was least frequently, and straining was most frequently associated with a motility abnormality. For each symptom, the highest prevalence was associated with failed BET. There was a significant increase in CTT with age only in men (p = 0.0006). In men, for each year of age there was a CTT increase of 1.02 h. The prevalence of abdominal pain and incomplete evacuation for females was significantly higher than that for males (both P < 0.05). The prevalence of low anal squeeze pressure for females was significantly higher than that for males, and the prevalence of poor rectal sensation for males was significantly higher than that for females (both P < 0.05). A significant decrease in basal anal and squeeze pressures with age occurred in women (p < 0.0001); an increase in age of one year was associated with a decrease in anal base pressure of 1.2 mmHg. Abnormal CTT and HR-ARM tests were associated with increased symptom frequency, but not severity.
Conclusions
There are significant age- and gender-related differences in symptoms, CTT, and HR-HRM parameters, rectal sensation, and expulsion, that may influence the multifaceted management of constipation.







Similar content being viewed by others
References
Mearin F, Lacy BE, Chang L et al. Bowel disorders. Gastroenterology. 2016. https://doi.org/10.1053/j.gastro.2016.02.031.
Whitehead WE, Wald A, Diamant NE et al. Functional disorders of the anus and rectum. Gut 1999;45:Ii55–Ii59.
Sommers T, Petersen T, Singh P et al. Significant morbidity and mortality associated with fecal impaction in patients who present to the emergency department. Dig Dis Sci. 2019;64:1320–1327. https://doi.org/10.1007/s10620-018-5394-8.
Aziz I, Whitehead WE, Palsson OS et al. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Rev Gastroenterol Hepatol. 2020;14:39–46. https://doi.org/10.1080/17474124.2020.1708718.
Camilleri M, Ford AC, Mawe GM et al. Chronic constipation. Nat Rev Dis Primers. 2017;3:17095. https://doi.org/10.1038/nrdp.2017.95.
Rao S, Hatfield R, Soffer E et al. Manometric tests of anorectal function in healthy adults. Am J Gastroenterol. 1999;94:773–783.
Carrington EV, Heinrich H, Knowles CH et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil. 2020;32:e13679. https://doi.org/10.1111/nmo.13679.
Lucak S, Lunsford TN, Harris LA. Evaluation and treatment of constipation in the geriatric population. Clin Geriatr Med. 2021;37:85–102. https://doi.org/10.1016/j.cger.2020.08.007.
Nojkov B, Baker JR, Chey WD et al. Age- and gender-based differences in anorectal function, gastrointestinal symptoms, and constipation-specific quality of life in patients with chronic constipation. Dig Dis Sci. 2023;68:1403–1410. https://doi.org/10.1007/s10620-022-07709-z.
Jameson JS, Chia YW, Kamm MA et al. Effect of age, sex and parity on anorectal function. Br J Surg. 1994;81:1689–1692.
Triadafilopoulos G, Lee M, Neshatian L. High prevalence of anorectal dysfunction in ambulatory patients with chronic constipation, regardless of colon transit time. Dig Dis Sci. 2023. https://doi.org/10.1007/s10620-023-08072-3.
Rosa-E-Silva L, Gerson L, Davila M et al. Clinical, radiologic, and manometric characteristics of chronic intestinal dysmotility: the Stanford experience. Clin Gastroenterol Hepatol. 2006;4:866–873.
Saad RJ. The wireless motility capsule: a one-stop shop for the evaluation of GI motility disorders. Curr Gastroenterol Rep. 2016;18:14.
Sheskin DJ. The cumulative frequency distribution. p35. Handbook of Parametric and Nonparametric Statistical Procedures, 4th edn. Boca Raton: Chapman & Hall/CRC; 2007.
Gelijns AC. Comparing the Development of Drugs, Devices and Clinical Procedures. P147–201. Modern Methods of Clinical Investigation. http://www.nap.edu/catalog/1550.html.
https://clinicaltrials.gov. Accessed 10-6-2023
Cali RL, Blachford GJ, Perry RE et al. Christensen MA. Normal variation in anorectal manometry. Dis Colon Rectum. 1992;35:1161–1164.
Triadafilopoulos G, Clarke JO, Kamal A et al. Intra-subject variability in high resolution anorectal manometry using the London classification: diagnostic and therapeutic implications. Dig Dis Sci. 2022;67:5014–5018.
Sonu I, Triadafilopoulos G, Gardner JD. Persistent constipation and abdominal adverse events with newer treatments for constipation. BMJ Open Gastroenterol. 2016;3:e000094. https://doi.org/10.1136/bmjgast-2016-000094).
Camilleri M, Brandler J. Refractory constipation: how to evaluate and treat. Gastroenterol Clin North Am. 2020;49:623–642.
Barnett JL, Hasler WL, Camilleri M. American Gastroenterological Association medical position statement on anorectal testing techniques. Gastroenterology 1999;116:732–7600.
Rao SS, Benninga MA, Bharucha AE et al. ANMS-ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders. Neurogastroenterol Motil. 2015;27:594–609.
Chiarioni G, Whitehead WE, Pezza V et al. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology 2006;130:657–664.
Girgis CM. Vitamin D and skeletal muscle: emerging roles in development, anabolism and repair. Calcif Tissue Int. 2020;106:47–55.
Chang L, Chey WD, Imdad A et al. American Gastroenterological Association-American College of Gastroenterology Clinical Practice Guideline: Pharmacological Management of Chronic Idiopathic Constipation. Gastroenterology 2023;164:1086–1106.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no Conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Triadafilopoulos, G., Gardner, J.D. Relationship of Age and Gender to Motility Test Results and Symptoms in Patients with Chronic Constipation. Dig Dis Sci 69, 1302–1317 (2024). https://doi.org/10.1007/s10620-024-08314-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08314-y