Abstract
Purpose
The number of leptomeningeal metastasis (LM) patients has increased in recent years, as the cancer survival rates increased. An optimal prediction of prognosis is essential for selecting an appropriate treatment. The European Association of Neuro-Oncology-European Society for Medical Oncology (EANO-ESMO) guidelines for LM proposed a classification based on the cerebrospinal fluid cytological findings and contrast-enhanced magnetic resonance imaging (MRI) pattern. However, few studies have validated the utility of this classification. This study aimed to investigate the prognostic factors of LM, including the radiological and cytological types.
Methods
We retrospectively analyzed the data of 240 adult patients with suspected LM who had undergone lumbar puncture between April 2014 and September 2021.
Results
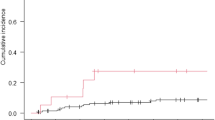
The most common primary cancer types were non-small-cell lung cancer (NSCLC) (143 (60%)) and breast cancer (27 (11%)). Positive cytology results and the presence of leptomeningeal lesions on contrast-enhanced MRI correlated with decreased survival in all patients. Nodular lesions detected on contrast-enhanced magnetic resonance were a poor prognostic factor in cytology-negative patients, while contrast-enhanced patterns had no prognostic significance in cytology-positive patients. Systemic therapy using cytotoxic agents and molecular-targeted therapy after LM diagnosis correlated with prolonged survival, regardless of the cytology results. Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor treatment and systemic chemotherapy after LM improved the survival of EGFR-mutated and wild-type NSCLC patients with positive cytology results.
Conclusions
This study validated the efficacy of prognostication according to the EANO-ESMO guidelines for LM. Systemic therapy after LM diagnosis improves the survival of NSCLC patients.


Similar content being viewed by others
Data availability
The data generated and analyzed during the current study are not publicly available for legal/ethical reasons but are available from the corresponding author upon reasonable request.
References
Le Rhun E, Weller M, Brandsma D, Van den Bent M, de Azambuja E, Henriksson R, Boulanger T, Peters S, Watts C, Wick W, Wesseling P, Rudà R, Preusser M (2017) EANO-ESMO clinical practice guidelines for diagnosis, treatment and follow-up of patients with leptomeningeal metastasis from solid tumours. Ann Oncol 28:iv84–iv99. https://doi.org/10.1093/annonc/mdx221
Li YS, Jiang BY, Yang JJ, Tu HY, Zhou Q, Guo WB, Yan HH, Wu YL (2016) Leptomeningeal metastases in patients with NSCLC with EGFR mutations. J Thorac Oncol 11:1962–1969. https://doi.org/10.1016/j.jtho.2016.06.029
Lee SJ, Lee JI, Nam DH, Ahn YC, Han JH, Sun JM, Ahn JS, Park K, Ahn MJ (2013) Leptomeningeal carcinomatosis in non-small-cell lung cancer patients: impact on survival and correlated prognostic factors. J Thorac Oncol 8:185–191. https://doi.org/10.1097/JTO.0b013e3182773f21
Yan W, Jing W, An N, Tian Y, Guo D, Kong L, Zhu H, Yu J (2019) The clinical characteristic and prognostic factors of leptomeningeal metastasis in patients with non-small-cell lung cancer-a retrospective study from one single cancer institute. Cancer Med 8:2769–2776. https://doi.org/10.1002/cam4.2156
Lee J, Choi Y, Han J, Park S, Jung HA, Su JM, Lee SH, Ahn JS, Park K, Ahn MJ (2020) Osimertinib improves overall survival in patients with EGFR-mutated NSCLC with leptomeningeal metastases regardless of T790M mutational status. J Thorac Oncol 15:1758–1766. https://doi.org/10.1016/j.jtho.2020.06.018
Liao BC, Lee JH, Lin CC, Chen YF, Chang CH, Ho CC, Shih JY, Yu CJ, Yang JC (2015) Epidermal growth factor receptor tyrosine kinase inhibitors for non-small-cell lung cancer patients with leptomeningeal carcinomatosis. J Thorac Oncol 10:1754–1761. https://doi.org/10.1097/jto.0000000000000669
Le Rhun E, Devos P, Weller J, Seystahl K, Mo F, Compter A, Berghoff AS, Jongen JLM, Wolpert F, Rudà R, Brandsma D, van den Bent M, Preusser M, Herrlinger U, Weller M (2021) Prognostic validation and clinical implications of the EANO ESMO classification of leptomeningeal metastasis from solid tumors. Neuro Oncol 23:1100–1112. https://doi.org/10.1093/neuonc/noaa298
Alder L, Trapani D, Bradbury C, Van Swearingen AED, Tolaney SM, Khasraw M, Anders CK, Lascola CD, Hsu L, Lin NU, Sammons S (2023) Durable responses in patients with HER2+ breast cancer and leptomeningeal metastases treated with trastuzumab deruxtecan. NPJ Breast Cancer 9:19. https://doi.org/10.1038/s41523-023-00519-0
Pellerino A, Soffietti R, Bruno F, Manna R, Muscolino E, Botta P, Palmiero R, Rudà R (2022) Neratinib and capecitabine for the treatment of leptomeningeal metastases from HER2-positive breast cancer: a series in the setting of a compassionate program. Cancers (Basel) 14:1192. https://doi.org/10.3390/cancers14051192
Chorti E, Kebir S, Ahmed MS, Keyvani K, Umutlu L, Kanaki T, Zaremba A, Reinboldt-Jockenhoefer F, Knispel S, Gratsias E, Roesch A, Ugurel S, Scheffler B, Schadendorf D, Livingstone E, Meier F, Glas M, Zimmer L (2021) Leptomeningeal disease from melanoma-poor prognosis despite new therapeutic modalities. Eur J Cancer 148:395–404. https://doi.org/10.1016/j.ejca.2021.02.016
Oberkampf F, Gutierrez M, Trabelsi Grati O, Le Rhun É, Trédan O, Turbiez I, Kadi A, Dubot C, Taillibert S, Vacher S, Bonneau C (2023) Phase II study of intrathecal administration of trastuzumab in patients with HER2-positive breast cancer with leptomeningeal metastasis. Neuro Oncol 25:365–374. https://doi.org/10.1093/neuonc/noac180
Kuiper JL, Hendriks LE, van der Wekken AJ, de Langen AJ, Bahce I, Thunnissen E, Heideman DA, Berk Y, Buijs EJ, Speel EJ, Krouwels FH, Smit HJ, Groen HJ, Dingemans AM, Smit EF (2015) Treatment and survival of patients with EGFR-mutated non-small cell lung cancer and leptomeningeal metastasis: a retrospective cohort analysis. Lung Cancer 89:255–261. https://doi.org/10.1016/j.lungcan.2015.05.023
Morshed RA, Saggi S, Cummins DD, Molinaro AM, Young JS, Viner JA, Villanueva-Meyer JE, Goldschmidt E, Boreta L, Braunstein SE, Chang EF, McDermott MW, Berger MS, Theodosopoulos PV, Hervey-Jumper SL, Aghi MK, Daras M (2023) Identification of risk factors associated with leptomeningeal disease after resection of brain metastases. J Neurosurg 13:1–12. https://doi.org/10.3171/2022.12.jns221490
Prabhu RS, Turner BE, Asher AL, Marcrom SR, Fiveash JB, Foreman PM, Press RH, Patel KR, Curran WJ, Breen WG, Brown PD, Jethwa KR, Grills IS, Arden JD, Foster LM, Manning MA, Stern JD, Soltys SG, Burri SH (2019) A multi-institutional analysis of presentation and outcomes for leptomeningeal disease recurrence after surgical resection and radiosurgery for brain metastases. Neuro Oncol 21:1049–1059. https://doi.org/10.1093/neuonc/noz049
Jung TY, Chung WK, Oh IJ (2014) The prognostic significance of surgically treated hydrocephalus in leptomeningeal metastases. Clin Neurol Neurosurg 119:80–83. https://doi.org/10.1016/j.clineuro.2014.01.023
Takano K, Kinoshita M, Takagaki M, Sakai M, Tateishi S, Achiha T, Hirayama R, Nishino K, Uchida J, Kumagai T, Okami J, Kawaguchi A, Hashimoto N, Nakanishi K, Imamura F, Higashiyama M, Yoshimine T (2016) Different spatial distributions of brain metastases from lung cancer by histological subtype and mutation status of epidermal growth factor receptor. Neuro Oncol 18:716–724. https://doi.org/10.1093/neuonc/nov266
Le Rhun E, Devos P, Winklhofer S, Lmalem H, Brandsma D, Kumthekar P, Castellano A, Compter A, Dhermain F, Franceschi E, Forsyth P, Furtner J, Galldiks N, Gàllego Pérez-Larraya J, Gempt J, Hattingen E, Hempel JM, Lukacova S, Minniti G, O’Brien B, Postma TJ, Roth P, Rudà R, Schaefer N, Schmidt NO, Snijders TJ, Thust S, van den Bent M, van der Hoorn A, Vogin G, Smits M, Tonn JC, Jaeckle KA, Preusser M, Glantz M, Wen PY, Bendszus M, Weller M (2022) Prospective validation of a new imaging scorecard to assess leptomeningeal metastasis: a joint EORTC BTG and RANO effort. Neuro Oncol 24:1726–1735. https://doi.org/10.1093/neuonc/noac043
Umemura S, Tsubouchi K, Yoshioka H, Hotta K, Takigawa N, Fujiwara K, Horita N, Segawa Y, Hamada N, Takata I, Yamane H, Kamei H, Kiura K, Tanimoto M (2012) Clinical outcome in patients with leptomeningeal metastasis from non-small cell lung cancer: Okayama lung cancer study group. Lung Cancer 77:134–139. https://doi.org/10.1016/j.lungcan.2012.03.002
Choi M, Keam B, Ock CY, Kim M, Kim TM, Kim DW, Heo DS (2019) Pemetrexed in the treatment of leptomeningeal metastasis in patients with EGFR-mutant lung cancer. Clin Lung Cancer 20:e442–e451. https://doi.org/10.1016/j.cllc.2019.03.005
Pellerino A, Bertero L, Pronello E, Rudà R, Soffietti R (2024) The early recognition and diagnosis of neoplastic meningitis. Expert Rev Neurother 24:105–116. https://doi.org/10.1080/14737175.2023.2295999
Acknowledgements
None
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
KNa, KT, and HA acquired data.
KNa and HA analyzed the data.
KNa, KNi, SO, TN and HA wrote the manuscript.
HA conceptualized the research.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board of the Osaka International Cancer Institute (reference no. 21122).
Consent to participate
The local institutional review board waivered written informed consent from patients for using clinical data for the present research.
Conflict of interests
The authors declare that they have no conflicts of interest in association with this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakagawa, K., Takano, K., Nishino, K. et al. Prognostic impact of clinical and radiological factors on leptomeningeal metastasis from solid cancers. J Neurooncol (2024). https://doi.org/10.1007/s11060-024-04616-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11060-024-04616-3