Abstract
Background
A grim prognosis of pancreatic cancer (PCa) was attributed to the difficulty in early diagnosis of the disease.
Aims
Identifying novel biomarkers for early detection of PCa is thus urgent to improve the overall survival rates of patients.
Methods
The study was performed firstly by identification of candidate microRNAs (miRNAs) in formalin-fixed, paraffin-embedded tissues using microarray profiles, and followed by validation in a serum-based cohort study to assess clinical utility of the candidates. In the cohorts, a total of 1273 participants from four centers were retrospectively recruited as two cohorts including training and validation cohort. The collected serum specimens were analyzed by real-time polymerase chain reaction.
Results
We identified 27 miRNAs expressed differentially in PCa tissues as compared to the benign. Of which, the top-four was selected as a panel whose diagnostic efficacy was fully assessed in the serum specimens. The panel exhibited superior to CA19-9, CA125, CEA and CA242 in discriminating patients with early stage PCa from healthy controls or non-PCa including chronic pancreatitis as well as pancreatic cystic neoplasms, with the area under the curves (AUC) of 0.971 (95% CI 0.956–0.987) and 0.924 (95% CI 0.899–0.949), respectively. Moreover, the panel eliminated interference from other digestive tumors with a specificity of 90.2%.
Conclusions
A panel of four serum miRNAs was developed showing remarkably discriminative ability of early stage PCa from either healthy controls or other pancreatic diseases, suggesting it may be developed as a novel, noninvasive approach for early screening of PCa in clinic.
Graphical Abstract

Similar content being viewed by others
Introduction
Pancreatic adenocarcinoma is the fourth leading cause of cancer-related mortality, and it is projected to become the second leading cause of cancer death by 2030 [1]. Pancreatic cancer (PCa) is characterized by extremely poor outcomes, with the 5-year relative survival rate of approximately 10% [2]. This low cancer survival rate is attributable to the difficulty in early diagnosis. Because of the lack of typical symptoms, more than two-thirds of patients with PCa are diagnosed with either regional or distant metastasis [3]. Early detection is a critical strategy for improving the overall survival of patients with PCa.
Unfortunately, current clinical diagnostic approaches for PCa are ineffective owing to their low sensitivity and/or specificity. Clinical diagnostic methods include imaging techniques and blood-based biomarkers. Imaging modalities, such as multidetector computed tomography, magnetic resonance imaging, and endoscopic ultrasonography with fine-needle aspiration, were limited by their disadvantages [4]. Carbohydrate antigen 19-9 (CA19-9), carbohydrate antigen 242 (CA242), carbohydrate antigen 125 (CA125), and carcinoembryonic antigen (CEA) are the common blood-based biomarkers for the clinical diagnosis of PCa [5]. However, the accuracy of these biomarkers is not strong because of their non-specific aberration in cancers other than PCa [6]. Though CA19-9 is the best-validated biomarker with a sensitivity of approximately 80%, it is limited by false-positive results in patients with inflammation and non-PCa lesions and false-negative results in Lewis-negative individuals.
In recent years, liquid biopsy based on biomarkers including circulating tumor cells, circulating tumor DNA, microRNAs (miRNAs), and exosomes in blood has proven to be a invasive and effective approach for the detection of cancer in its early stages [7]. Notably, prior research found that miRNAs-based biomarkers have been used for the diagnosis of patients with PCa. MiRNAs are small non-coding RNAs composed of 17–25 nucleotides, which are relative stable in blood and play important roles in various cancer-associated biological processes. For example, miR-132 was reported to function as a oncogene in pancreatic ductal adenocarcinoma (PDAC), a main subtype accounting for 90% of all subjects with PCa and promote the proliferation, invasion and migration of human pancreatic carcinoma cells [8, 9]. High expression of miR-30 family promoted migration and invasion of PCa stem cells [10, 11]. MiR-24 was shown to promote tumor growth and angiogenesis by suppressing Bim expression in vivo [12]. These miRNAs were included in the panel by identification in our work.
In this study, we identified a panel of four elevated serum miRNAs and assessed the clinical utility of the panel as noninvasive biomarker for the detection of early stage PCa in subjects from multiple centers.
Materials and Methods
Study Design and Participants
This study included a biomarker discovery stage in formalin-fixed, paraffin-embedded (FFPE) tissues, as well as clinical training and validation cohorts in retrospectively collected serum specimens. The cohort study was conducted according to the Technical Guidelines for Clinical Trials of In Vitro Diagnostic Reagents and the Administrative Measures for Registration and Filing of In Vitro Diagnostic Reagents.
For the biomarker discovery stage, miRNA arrays was performed to identify miRNA candidates, which were approved by the institutional review board (IRB) of both institutions (IRB#08-15183; IRB#10-15627). 300 FFPE tissues from the University of Nebraska Medical Center and Creighton University Medical Center, were grouped into normal (benign), early stage [pancreatic intraepithelial neoplasia (PanIN) I/II/III to TNM stage IIA], and advanced-stage (> IIA) groups. Each group contained 100 tissue cores with ≥ 95% statistical power. Then, RT-PCR assays were performed to verify the levels of candidate miRNAs in FFPE tissues.
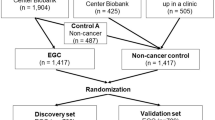
In the training and validation cohorts, dual-channel RT-PCR was performed in 1273 specimens enrolled from four medical centers, including Peking Medical Union College Hospital affiliated to the Chinese Medical Academy of Sciences, Liaoning Cancer Hospital & Institute, Shanghai Renji Hospital affiliated to Shanghai Jiaotong University, and Xiangya Hospital affiliated to Central South University between 2011 and 2021 who met the inclusion criteria (Supplementary Material 1). Subjects in both cohorts were classified into four groups: healthy control (HC), PDAC, chronic pancreatitis (CP), and pancreatic cystic neoplasms (PCN). In the PDAC group, all the tumors were histologically proven adenocarcinomas. All the cysts included in the PCN group were surgically confirmed not cancerous. Subjects were randomly allocated into two cohorts (training cohort, n = 635; validation cohort, n = 638). The cohort study was approved by the local ethics committees of Dalian University of Technology.
Externally, the discriminative model was further validated using a set of 51 non-PCa digestive tumors, including 29 colorectal, 7 hepatic, 6 esophageal, and 9 gastric carcinomas, respectively, to assess the tumor specification of the panel.
Microarray Expression Profiling of MiRNAs in FFPE Tissues
miRNAs were extracted from selected FFPE tissues using the mirVana™ miRNA isolation kit (Ambion, USA) according to the manufacturer’s protocol. miRNA microarray profiling was performed using Affymetrix GeneChip miRNA arrays (Affymetrix, Santa Clara, CA, USA) according to the manufacturer’s protocol. RNA was labeled by the addition of polyA polymerase using the Genisphere FlashTag HSR kit (Genisphere, Hatfield, PA, USA) following the manufacturer’s instructions. Labeled RNA was hybridized to the Affymetrix miRNA array 1.0. Chips were washed and stained in Fluidic Station 450 (Affymetrix, USA). Each chip was scanned using the GeneChip Scanner 300 7G system (Affymetrix, USA) to control the image scanning.
Serum RNA Isolation
Serum samples were assayed in a blinded manner. Total RNA was extracted from 0.25-mL serum samples using RNAiso Blood (Takara, Japan) according to the manufacturer’s instruction. Briefly, RNAiso Blood reagent (threefold more than the sample volume) was added to each serum sample, which was then lysed thoroughly via violent vortexes. Next, chloroform and isopropyl alcohol were used to precipitate RNA. The obtained RNA precipitate was then washed with 75% ethanol. Finally, RNA was quantified using a NanoDrop spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA).
Dual-Channel RT-PCR
The serum levels of miRNAs and endogenous U6 as an internal control were detected by dual-channel RT-PCR. RNA was transcribed into cDNA using miRNA-specific stem-loop primers and a PrimeScript™ RT reagent kit with gDNA Eraser (Perfect Real Time) (Takara, Japan) in a scaled-down (10 μL) reverse transcription reaction. Each reaction contained primers for both the internal control and one miRNA. RT-PCR was performed using Probe qPCR Mix (Takara, Japan) and pre-designed miRNA-specific probes and primers. To collect the signals of both the target miRNA and U6 simultaneously, miRNAs and U6 probes were labeled with different fluorophores. Each reaction was prepared in triplicates and performed on the LightCycler 480 II System (Roche, Switzerland) through 45-cycle amplification.
Statistical Analysis
To screen the miRNA candidates from the discovery cohort, differential miRNA expression analysis was performed using the limma package in R software, version 4.1.1. The miRNA levels detected by microarray were first log2-transformed. MiRNA levels detected by RT-PCR were represented as the delta cycle threshold (Ct) value, which was the relative Ct value of each miRNA normalized to that of U6. Lower delta Ct values indicate higher miRNA expression. For continuous variables, data were expressed as the mean ± standard deviation (SD) and compared using Student’s t-test or one-way or two-way ANOVA performed in GraphPad Prism software, version 9.0. For categorical variables, the Chi-squared test was used to compare differences between two groups. Multiple linear regression was used to construct disease discrimination models using R software, version 4.1.1. Receiver operating characteristic (ROC) curves were used to evaluate the performance of these models. In addition, both univariate and multivariate logistic regression analyses were used to evaluate the relevant risk factors for PCa. Unless stated otherwise, p < 0.05 was considered statistically significant.
Results
Demographic Characteristics of Participants
In total, 1273 subjects from multiple centers were recruited into the serum cohort study, including 571, 90, 217, and 395 subjects in the PDAC, CP, PCN (45 patients with solid pseudopapillary neoplasm, SPN; 10 patients with serous cystic neoplasm, SCN; 62 patients with intraductal papillary mucinous neoplasm mucinous cystic neoplasm, IPMN; 50 patients with mucinous cystic neoplasm, MCN; 37 patients with pancreatic neuroendocrine tumor and 13 patients with pancreatic mass lesions), and HC groups, respectively. No significant differences in age, sex, body mass index (BMI), smoking history, drinking history, family history of cancer, and history of diabetes were found between the two cohorts. The demographic and clinicopathological characteristics of all subjects are presented in Table 1.
Identification of the Candidate miRNAs
In the discovery stage, we employed a microarray expression profiling approach to identify a clinically relevant miRNA panel for the early detection of patients with PCa. Using the criteria of absolute log2(fold change) > 1 and FDR (Benjamini–Hochberg-adjusted p) < 0.05, we identified 53 and 43 miRNAs with significantly different levels in patients with early stage (PanIN to TNM stage IIA) and advanced-stage PCa (TNM stage > IIA), respectively, compared with those in benign controls (Fig. 1a, b). Of these, 27 miRNAs were consistently up-regulated or down-regulated in both comparisons (Fig. 1c, Supplementary Figure S1). The following criteria were used for prioritizing candidate miRNAs: absolute log2(fold change) > 4 and FDR < 0.05. By this criteria, four miRNAs (hsa-miR-132-3p, hsa-miR-30c-5p, hsa-miR-24-3p, and hsa-miR-23a-3p) were selected as candidate biomarkers to be further verified.
Identification of the miRNA panel for PCa diagnosis. The two-dimensional plot of miRNAs identified by microarray profiling in PCa tissues at early (PanIN to TNM stage IIA), a or advanced stages (> IIA), (b) compared with benign controls. miRNAs were selected using the criteria of absolute log2(fold change) > 1 (vertical dashed line) and FDR (Benjamini–Hochberg-adjusted p value) < 0.05 (horizontal dashed line). c Heat map of differentially expressed miRNAs in PCa tissues in both early (PanIN to TNM stage IIA) and advanced stages (> IIA) compared with benign controls
Validation of the Candidate miRNAs
These candidates were subsequently verified by RT-PCR analysis in FFPE tissues, and they were consistently up-regulated in patients with PCa (p < 0.0001; Fig. 2a). Further, to confirm whether these four miRNAs can serve as noninvasive markers, we detected their endogenous serum levels by dual-channel RT-PCR in 1273 subjects and observed significantly higher (p < 0.0001) levels in patients with CP and other pancreatic diseases including PDAC than in HC (Fig. 2b). However, hsa-miR-23a-3p levels did not differ between patients with CP and HC (p = 0.22). Subjects with PCa were staged according to TNM staging via histopathology. Especially, the four miRNA exhibited the significant over-expression in patients with PDAC at both early stage (TNM stage < = IIA) and advanced stage (TNM stage > IIA) compared to non-PDAC subjects (including HC as well as subjects with CP and PCN), which indicated the potential of these four miRNAs as noninvasive biomarkers for early detection of PCa (p < 0.0001; Fig. 2c).
Validation of the candidate miRNAs in tissues and serum specimens. a RT-PCR analysis of candidate miRNAs in benign, early-stage, and advanced-stage tissues. Each group was duplicated with nine samples. The column and bar represent the mean ± SD. Statistical significance was analyzed by one-way ANOVA. ****p < 0.001. b Comparison of the serum levels of four miRNAs between subjects with chronic pancreatitis (CP, n = 90), pancreatic cystic neoplasms (PCN, n = 217), pancreatic ductal adenocarcinoma (PDAC, n = 571) and healthy controls (HC, n = 395). c Comparison of the serum levels of four miRNAs between non-PDAC subjects (including HC, individuals with CP and PCN), patients with early stage PDAC (TNM stage ≤ IIA), and patients with advanced PDAC (TNM stage > IIA). The median is the line in the middle of the box, and the 25th and 75th percentiles are the lower and upper parts, respectively, of the box. The bars above and below the box represents the maximum and minimum values, respectively. The points above and below the bar are outliers. Statistical significance was analyzed using an unpaired t-test. ****p < 0.0001
Diagnostic Ability of the MiRNA Panel in the Detection of Early-Stage PCa
The detection of early-stage PCa is challenging in clinical practice. To best evaluate the performance of the miRNAs as panel in detecting subjects with early-stage PCa, a multiple linear regression model was constructed in the training cohort and validated in the validation cohort. Firstly, the miRNA panel in distinguishing patients with PDAC at different stage was evaluated. Compared with HC, the miRNA panel demonstrated an excellent diagnostic performance in patients with PCa with the area under the curves (AUC) values of 0.978, 0.968, 0.968 and 0.974 in the training cohort and 0.929, 0.925, 0.908 and 0.876 in the validation cohort for stage I, II, III, and IV, respectively (Supplementary Figure S2, Supplementary Table S1).
Notably, subjects with early-stage PCa were also investigated. Compared with HC, the sensitivity, specificity, and accuracy of the miRNA panel in the detection of early-stage PCa were 92.9% (95% CI 88.2%–97.6%), 92.9% (95% CI 89.3%–96.5%), and 92.9% (95% CI 92.9%–92.9%), respectively, in the training cohort and 94.2% (95% CI 89.7%–98.7%), 92.4% (95% CI 88.7%–96.1%), and 93.0% (95% CI 93.0%–93.1%), respectively, in the validation cohort (Fig. 3a, Table 2).
ROC of the miRNA panel in the detection of early stage PCa. Receiver operating characteristic (ROC) curves of the miRNA panel and common biomarkers in distinguishing patients with early-stage pancreatic ductal adenocarcinoma (PDAC, TNM stage ≤ IIA) from healthy controls (HC) (a), non-PDAC subjects (healthy controls and individuals with chronic pancreatitis and pancreatic cystic neoplasms) (b), and patients with chronic pancreatitis (CP) (c) in the training and validation cohorts
The discriminative ability of the miRNA panel for subjects with early stage PCa versus non-PDAC subjects was also evaluated. The sensitivity, specificity, and accuracy were 93.8% (95% CI 89.4%–98.2%), 75.7% (95% CI 71.2%–80.2%), and 80.1% (95% CI 80.1%–80.2%), respectively, in the training cohort and 95.1% (95% CI 91.0%–99.3%), 77.0% (95% CI 72.6%–81.4%), and 81.1% (95% CI 81.0%–81.2%), respectively, in the validation cohort (Fig. 3b, Table 2).
The sensitivity, specificity, and accuracy of the miRNA panel in discriminating subjects with early-stage PCa from subjects with CP were 81.4% (95% CI 74.2%–88.6%), 86.7% (95% CI 76.7%–96.6%), and 82.9% (95% CI 82.7%–83.1%), respectively, in the training cohort and 80.6% (95% CI 72.9%–88.2%), 82.2% (95% CI 71.1%–93.4%), and 81.1% (95% CI 80.9%–81.3%), respectively, in the validation cohort (Fig. 3c, Table 2).
To further demonstrate the performance of the miRNA panel in the detection of early-stage PDAC, the panel was compared with four biomarkers used routinely in clinical practice, namely CA125, CA19-9, CA242, and CEA, using the same serum specimens. The results demonstrated that the performance of the four-miRNA panel was substantially better overall than that of the biomarkers routinely used in discriminating subjects with early-stage PDAC from non-PDAC subjects, subjects with CP, or HC (Fig. 3, Supplementary Table S2 and S3).
Performance of the MiRNA Panel in Discriminating Early-Stage PCa from PCN Subtypes
Patients harboring a cystic lesion are more likely to develop cancer [13]. PCN is generally classified into SPT, SCN, MCN, and IPMN subtypes [14]. Patients with these subtypes were enrolled in this study. The discriminative ability of the miRNA panel for subjects with early stage PCa versus those with PCN subtypes was assessed.
The sensitivity, specificity, and accuracy of the panel in distinguishing patients with early stage PDAC from patients with PCN were 85.8% (95% CI 79.4%–92.3%), 67.7% (95% CI 58.5%–76.9%) and 77.4% (95% CI 77.2%–77.5%), respectively, in the training cohort and 90.3% (95% CI 84.6%–96.0%), 69.0% (95% CI 59.9%–78.1%), and 79.8% (95% CI 79.6%–80.0%), respectively, in the validation cohort (Fig. 4a, Supplementary Table S4). Collectively, these findings supported the potential of the miRNA panel to discriminate patients with early stage PDAC from those with high-risk PCa.
ROC of the miRNA panel in the detection of PCN. Receiver operating characteristic (ROC) curves of the miRNA panel in distinguishing patients with pancreatic cystic neoplasms (PCN) from those with early stage pancreatic ductal adenocarcinoma (PDAC, TNM stages ≤ IIA) (a), healthy controls (HC) (b), and patients with chronic pancreatitis (CP) (c) in the training and validation cohorts
The ability of the miRNA panel to discriminate patients with PCN from patients with CP or HC was also explored (Fig. 4b and c). Interestingly, the panel had AUCs of 0.841 (95% CI 0.792–0.889) and 0.771 (95% CI 0.702–0.841) in discriminating individuals with PCN from HC in the training and validation cohorts, respectively (Fig. 4b). However, it failed to classify subjects with PCN from those with CP (AUC, 0.681 and 0.587) by the miRNA panel (Fig. 4c).
Specificity of the MiRNA Panel in Discriminating PCa from Other Digestive Tumors
Biomarkers commonly used in clinic usually fail to distinguish different types of malignant tumors, especially digestive tumors, such as liver, gastric, esophageal, and colorectal cancers. To evaluate the ability of the miRNA panel to discriminate PCa from other digestive tumors, we recruited 29, 7, 6, and 9 patients with colorectal carcinoma, hepatic carcinoma, esophageal carcinoma, and gastric carcinoma, respectively. Of these, 46 tumors were predicted to be non-PCa using the discrimination model of PDAC versus non-PDAC, and the specificity was 90.2% (Table 3). These data highlight the ability of the miRNA panel to eliminate the interference of other digestive tract tumors.
Discussion
In this study, a panel of four serum miRNAs was identified and validated to distinguish PCa, especially at its early stages, from HC and individuals with CP or other pancreatic diseases with high sensitivity and specificity. These findings highlight the potential of circulating miRNAs as noninvasive biomarkers for the early detection of PCa.
Several studies identified circulating miRNAs as biomarkers for distinguishing patients with PDAC from healthy subjects [15,16,17,18]. However, they failed to validate the detection ability of biomarkers in distinguish early stage PCa from interfering diseases and high-risk groups, which is an important benchmark to assess the diagnostic ability of biomarkers. Moreover, these single-center studies did not account for regional variations. For example, elevated serum miR-1290 was reported early to distinguish patients with low-stage PCa from healthy and disease controls [18]. However, its clinical utility was limited as the sample size in the study was small (n = 133), and the single-target biomarker was not tumor-specific in PCa. It was also reported that miR-1290 may be a potential biomarker of high-grade serous ovarian carcinoma [19]. Therefore, a biomarker study should be with a large sample size, high-throughput screening, and validation with diverse groups including other pancreatic diseases and other cancers besides PCa.
Similar to previous reports, this study also demonstrated that a panel of multiple markers is usually superior to a single marker. We compared the performance of the four miRNAs individually and in combination (Supplementary Figure S3). Individually, hsa-miR-30c-5p had the best performance in all three comparison sets. The combination of hsa-miR-30c-5p and hsa-miR-23a-3p displayed superior ability in distinguishing patients with early stage PDAC from those with CP. These findings highlight the advantages of using multiple miRNAs in combination.
This study had several strengths. First, this biomarker study began with a high-throughput screening for differential miRNAs in early stage PCa tissues compared with benign controls. Second, we enrolled a large number of participants from multiple centers in different regions of the country to obtain results that were as representative as possible. In addition, to fully demonstrate the performance of the miRNA panel, we included both healthy individuals and patients with multiple high-risk diseases, including CP and PCN, as controls. We also attempted to distinguish pancreatic mucinous tumors from serous tumors given that mucinous tumors including IPMN and MCN are usually more malignant than the other subtypes of PCN. However, the performance of the miRNA panel was not ideal (AUC = 0.68, 95% CI 0.60–0.75; Supplementary Figure S4). Furthermore, we validated the discrimination model in a group of subjects with other digestive tumors, thereby highlighting the tumor-specific miRNA panel as biomarker.
Our findings also suggest the promise of the miRNA panel in the postoperative treatment of PCa. We tested an independent set including 10 pre-treated patients and 20 patients who underwent surgery, radiotherapy, or chemotherapy for PCa. Of these, 19 patients after receiving treatment were predicted to be PCa-negative, and the levels of all four miRNAs were significantly decreased after treatment (Supplementary Figure S5).
This study had a few limitations. This study analyzed associations of several risk factors, such as gender, age, smoking, drinking, obesity, a history of cancers, and diabetes, with PCa by univariate and multivariate logistic regression analysis (Supplementary Table S5). Similar to previous reports [20], our results revealed that gender, age, drinking, BMI, a family history of cancer, and diabetes were significantly associated with the risk of PCa (all p < 0.05). However, multivariate analysis illustrated that only age, a family history of cancer, and diabetes were independent risk factors for PCa while smoking, drinking, and BMI were not independent risk factors for PCa. As a potential reason, smoking and drinking might be biased by sex. Via excluded variable analysis, we found that BMI was the intermediary variable of a history of cancers and diabetes, which resulted in the loss of significance of BMI in multivariate analysis. Furthermore, this cohort study was retrospectively rather than prospectively designed. The diagnostic ability of the miRNA panel was needed to be further accessed in a prospective trial, which is underway by us.
In summary, our findings indicated that the four-miRNA panel could be a superior classifier for discriminating PCa from healthy individuals or those in other at-risk groups. The panel is likely to be an adjunctive method in clinical practice of early diagnosis of PCa.
Data Availability
Data are available on reasonable request to the corresponding author.
References
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–2921.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Park W, Chawla A, O’Reilly EM. Pancreatic cancer: a review. JAMA. 2021;326:851–862.
Singhi AD, Koay EJ, Chari ST, Maitra A. Early detection of pancreatic cancer: opportunities and challenges. Gastroenterology. 2019;156:2024–2040.
Ge L, Pan B, Song F et al. Comparing the diagnostic accuracy of five common tumour biomarkers and CA19-9 for pancreatic cancer: a protocol for a network meta-analysis of diagnostic test accuracy. BMJ Open. 2017;7:e018175.
Luo H, Shen K, Li B, Li R, Wang Z, Xie Z. Clinical significance and diagnostic value of serum NSE, CEA, CA19-9, CA125 and CA242 levels in colorectal cancer. Oncol Lett. 2020;20:742–750.
Yang J, Xu R, Wang C, Qiu J, Ren B, You L. Early screening and diagnosis strategies of pancreatic cancer: a comprehensive review. Cancer Commun (Lond). 2021;41:1257–1274.
Moghbeli M, Zangouei AS, Nasrpour Navaii Z, Taghehchian N. Molecular mechanisms of the microRNA-132 during tumor progressions. Cancer Cell Int. 2021;21:439.
Zhang H, Liu A, Feng X et al. MiR-132 promotes the proliferation, invasion and migration of human pancreatic carcinoma by inhibition of the tumor suppressor gene PTEN. Prog Biophys Mol Biol. 2019;148:65–72.
Tsukasa K, Ding Q, Miyazaki Y, Matsubara S, Natsugoe S, Takao S. miR-30 family promotes migratory and invasive abilities in CD133(+) pancreatic cancer stem-like cells. Hum Cell. 2016;29:130–137.
Xiong Y, Wang Y, Wang L et al. MicroRNA-30b targets Snail to impede epithelial-mesenchymal transition in pancreatic cancer stem cells. J Cancer. 2018;9:2147–2159.
Liu R, Zhang H, Wang X et al. The miR-24-Bim pathway promotes tumor growth and angiogenesis in pancreatic carcinoma. Oncotarget. 2015;6:43831–43842.
Mukewar SS, Sharma A, Phillip N et al. Risk of pancreatic cancer in patients with pancreatic cysts and family history of pancreatic cancer. Clin Gastroenterol Hepatol. 2018;16:1123–1130.
Carmicheal J, Patel A, Dalal V et al. Elevating pancreatic cystic lesion stratification: Current and future pancreatic cancer biomarker(s). Biochim Biophys Acta Rev CANCER. 2020;1873:188318.
Schultz NA, Dehlendorff C, Jensen BV et al. MicroRNA biomarkers in whole blood for detection of pancreatic cancer. JAMA. 2014;311:392–404.
Nakamura K, Zhu Z, Roy S et al. An exosome-based transcriptomic signature for noninvasive, early detection of patients with pancreatic ductal adenocarcinoma: a multicenter cohort study. Gastroenterology. 2022;163:1252–1266.
Seyed Salehi A, Parsa-Nikoo N, Roshan-Farzad F et al. MicroRNA-125a-3p, -4530, and -92a as a Potential Circulating MicroRNA Panel for Noninvasive Pancreatic Cancer Diagnosis. Dis Markers. 2022;2022:8040419.
Li A, Jun Y, Kim H et al. MicroRNA array analysis finds elevated serum miR-1290 accurately distinguishes patients with low-stage pancreatic cancer from healthy and disease controls. Clin Cancer Res. 2013;19:3600–3610.
Kobayashi M, Sawada K, Nakamura K et al. Exosomal miR-1290 is a potential biomarker of high-grade serous ovarian carcinoma and can discriminate patients from those with malignancies of other histological types. J Ovarian Res. 2018;11:81.
GBD 2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2019;4:934–947.
Acknowledgments
We thank Joe Barber Jr., PhD, from Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the English text of a draft of this manuscript.
Funding
This work was funded by Natural National Science Foundation of China, 81770846 and 81642006, US Hirshberg Foundation for Pancreatic Cancer Research, AH201901083, and Kante Seeds Foundation for Cancer Research, KD2021030001. The English text of a draft of this manuscript was edited by Joe Barber Jr., PhD, from Liwen Bianji (Edanz) (www.liwenbianji.cn). It was funded by Fundamental Research Funds for the Central Universities (3332022004, Grant Recipient: Jianzhou Liu).
Author information
Authors and Affiliations
Contributions
VLG, SH, YT, HW and GGX: Conceptualization, JH, YG, JL, RZ, JW and SW: Methodology, JH and HC: Software, GG and GGX: Validation, JH and HC: Formal analysis, JH, GG, JL and YG: Investigation, YL, MY, YS, DS, ZX, HW and JG: Resources, JH and GG: Data curation, JH: Writing-original draft, GGX: Writing-review & editing, JH and HC: Visualization, ZZ and JG: Supervision, GG and JG: Project administration, GGX: Funding acquisition.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the University of Nebraska Medical Center and Creighton University Medical Center (IRB#08-15183; IRB#10-15627) and the Ethical Committees of Dalian University of Technology.
Informed consent
Patient consent was waived due to all specimens were from participating patients who cannot be identified.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Huang, J., Gao, G., Ge, Y. et al. Development of a Serum-Based MicroRNA Signature for Early Detection of Pancreatic Cancer: A Multicenter Cohort Study. Dig Dis Sci 69, 1263–1273 (2024). https://doi.org/10.1007/s10620-024-08338-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08338-4