Abstract
Background
Many lesions in the anterior skull base may compress the optic nerve (ON), leading to vision loss, and even irreversible blindness. Although decompression of the optic nerve has traditionally been achieved transcranially, the endoscopic endonasal approach (EEA) is gaining traction as a minimally invasive approach recently.
Method
We describe the key steps of an EEA ON decompression. The relevant surgical anatomy with illustration is described. Additionally, a video detailing our technique and instruments on an illustrative case is provided.
Conclusion
Endoscopic endonasal approach ON decompression with a straight feather blade is a feasible, minimally invasive procedure to decompress the ON in the setting of anterior skull base mass lesions.





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Agosti E, Leonel LCPC, Alexander AY, Graepel S, Pinheiro-Neto CD, Peris-Celda M (2022) Endoscopic endonasal surgical anatomy of the optic canal: key anatomical relationships between the optic nerve and ophthalmic artery. Acta Neurochir (Wien). https://doi.org/10.1007/s00701-022-05395-4
Bander ED, Singh H, Ogilvie CB et al (2018) Endoscopic endonasal versus transcranial approach to tuberculum sellae and planum sphenoidale meningiomas in a similar cohort of patients. J Neurosurg 128(1):40–48. https://doi.org/10.3171/2016.9.JNS16823
Cabrilo I, Dorward NL (2020) Endoscopic endonasal intracanalicular optic nerve decompression: how I do it. Acta Neurochir (Wien) 162(9):2129–2134. https://doi.org/10.1007/s00701-020-04476-6
Caporlingua A, Prior A, Cavagnaro MJ et al (2019) The intracranial and intracanalicular optic nerve as seen through different surgical windows: endoscopic versus transcranial. World Neurosurg 124:522–538. https://doi.org/10.1016/j.wneu.2019.01.122
Chen B, Zhang H, Zhai Q, Li H, Wang C, Wang Y (2022) Traumatic optic neuropathy: a review of current studies. Neurosurg Rev 45(3):1895–1913. https://doi.org/10.1007/s10143-021-01717-9
Jacquesson T, Abouaf L, Berhouma M, Jouanneau E (2014) How I do it: the endoscopic endonasal optic nerve and orbital apex decompression. Acta Neurochir (Wien) 156(10):1891–1896. https://doi.org/10.1007/s00701-014-2199-1
Labib MA, Prevedello DM, Fernandez-Miranda JC et al (2013) The medial opticocarotid recess: an anatomic study of an endoscopic key landmark for the ventral cranial base. Neurosurgery 72. https://doi.org/10.1227/NEU.0b013e318271f614
Luxenberger W, Stammberger H, Jebeles JA, Walch C (1998) Endoscopic optic nerve decompression: the Graz experience. Laryngoscope 108(6):873–882. https://doi.org/10.1097/00005537-199806000-00016
Pletcher SD, Metson R (2007) Endoscopic optic nerve decompression for nontraumatic optic neuropathy. Vol 133. https://jamanetwork.com/. Accessed 2/4/23
Sakata K, Takeshige N, Nagata Y et al (2019) Endoscopic endonasal removal of primary/recurrent meningiomas in the medial optic canal: surgical technique and long-term visual outcome. Oper Neurosurg 17(5):470–480. https://doi.org/10.1093/ons/opz001
Author information
Authors and Affiliations
Contributions
Conception and design: DP, KW; supervision: DP, KW; materials: DP, KW; data collection and/or processing: AK; analysis and/or interpretation: AK; literature review: AK, GF; writer: AK, DP; critical review: GF, KW.
Corresponding author
Ethics declarations
Ethics approval
Pursuant to our institutional review board’s bylaws, as this manuscript includes less than three participants, no human subject review nor approval is required. Notwithstanding, this study followed all recommendations set forth in the Belmont Report.
Consent to participate
All patients in the study consented to the procedure.
Consent for publication
All patients in the study consented to their de-identified data being published.
Conflict of interest
The authors declare no competing interests.
Additional information
Key points
• Various pathologies in the anterior skull base, such as anterior clinoid, transsellar, and olfactory groove meningiomas, may lead to irreversible blindness by compromising the optic nerve.
• While transcranial decompression has been the traditional method, the endoscopic endonasal approach (EEA) is gaining popularity as a minimally invasive alternative, showing better visual outcomes.
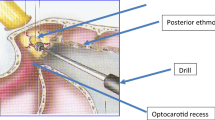
• Understanding the relevant surgical anatomy is crucial, including the sphenoid sinus structures, clinoid portion of the internal carotid artery, and the medial opticocarotid recess (MOCR), which is a key endoscopic ventral landmark.
• The MOCR marks the ophthalmic portion of the internal carotid artery, and its relationship with the optic nerve in the optic canal is significant for the EEA, especially concerning the lateral branch.
• Patients are positioned supine with their heads secured in a Mayfield frame, and stereotactic neuronavigation is calibrated following induction and intubation.
• The transsphenoidal phase involves standard transnasal dissection, middle turbinectomy, nasoseptal flap creation, ethmoidectomies, sphenoid osteotomy, and careful drilling down of the sphenoid sinus to expose relevant structures.
• The optic nerve decompression involves opening the optic sheath using specialized tools, including a back cutting feather blade, dissecting the dura, and stripping and decompressing the optic nerve. This process allows exposure of the optic canal for 270–360° disease resection in most cases.
• DuraGen® graft is used for reconstructing the dural defect, and the nasoseptal flap is rotated upwardly to cover the craniotomy. Gelfoam® pieces sustain the flap in position, followed by a Valsava maneuver to check for residual leaks.
• Difficult sinusoidal anatomy, prior septoplasty, and other factors may limit the EEA. To avoid complications, careful preoperative imaging studies, routine use of neuronavigation, and specific precautions during bone drilling are recommended.
• Patients should be informed about potential risks, and follow-up with a neuro-ophthalmologist is essential for monitoring visual changes.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 25.4 MB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keister, A., Wu, K.C., Finger, G. et al. Endoscopic endonasal decompression of the optic nerve in the setting of compressive lesions: how I do it. Acta Neurochir 166, 129 (2024). https://doi.org/10.1007/s00701-024-05994-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05994-3