Abstract
Our SepsiVit study showed that long-term, automatically analyzed ECG recordings can be used to determine heart rate variability (HRV) features associated with the clinical deterioration of early septic patients at the ED. This study focus on the influence of cardiovascular medication on HRV in patients with early sepsis at the ED. This study is an exploratory post-hoc analysis of our SepsiVit study. Eligible patients were connected to a mobile bedside monitor for continuously ECG measurements. The first 3 hours were analyzed for this study. Between January 2017 and December 2018, 171 patients were included with early sepsis, defined as infection and two or more systemic inflammatory response syndrome criteria. We excluded sixteen patients because of insufficient measurements. Therefore, we included 155 patients in the final analysis: 72.9% with sepsis, 2.6% with septic shock, and 24.5% classified as infection. In 9.0% of the patients, medication directly impacting cardiac contractility was administered, while 22.6% received medication with an indirect effect. A combination of both types of medication was prescribed to 17.4% of the patients. The majority of patients (51.0%) did not utilize any cardiovascular medication. Patients using both medication with direct and indirect effect were on average 10 years older than patients using no cardiovascular medication (p 0.037). No differences in vital signs or HRV parameters were found in patients using cardiovascular medication. Our results showed that HRV is not influenced by cardiovascular medication. Consequently, the correction of HRV features for the use of cardiovascular medication is unnecessary when analyzing, modelling, and interpreting these signals.
Similar content being viewed by others
Introduction
Early recognition of sepsis is crucial for timely treatment and resuscitation to prevent organ dysfunction and mortality in patients with sepsis [1]. Current diagnostic criteria employed to recognize early sepsis in the emergency department (ED) use a combination of vital parameters combined with the suspicion of infection. Yet, these criteria are insufficient to precisely estimate the severity of illness or monitor the response to treatment. A promising approach to improve early recognition of hemodynamic instability in sepsis and monitor the response to treatment seems analyses of changes in vital signs over time, called variability analysis. In the general population, high degrees of variability mark health, while disease is associated with reduced variability [2].
Heart rate variability (HRV) is one of the parameters studied in variability analysis. HRV refers to the variations in heartbeat intervals or correspondingly in the instantaneous heart rate, which gives a reliable reflection of the physiological factors influencing the normal rhythm of the heart [3]. Furthermore, it provides robust information about the interaction between the sympathetic and parasympathetic nervous systems [3]. HRV in septic patients has been primarily studied in small pilot studies and studies in Intensive Care Unit (ICU) patients [4,5,6,7]. However, HRV has not yet been studied in septic patients at the ED. The fact that septic patients at the ED are less severely ill than ICU patients, but are at major risk for deterioration, makes further analysis of HRV at the ED even more relevant [4].
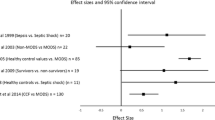
HRV is influenced by numerous factors like age, sex, race, physiological determinants influencing the cardiac system, sepsis itself, and by medication. Based on a pilot study at our ED, we know that 34% of patients presenting with sepsis use beta-blockers, 15% use dihydropyridines, 24% diuretics, and 25% renin-angiotensin system (RAS)-inhibitors [1]. The influence of medication on HRV was investigated in different patient populations, including Multi Organ Dysfunction Syndrome (MODS) patients at ICU [8,9,10,11,12,13,14]. In these previous studies, beta-blockers, dihydropyridines, and RAS-inhibitors had ambiguous effects on HRV. These ambiguous effects on HRV were also found in patients with end stage renal disease or congestive heart failure using spironolactone [15,16,17,18]. This ambiguous effect may depend on underlying pathology or comorbidities [12].
This study aimed to expand insight into the influence of cardiovascular medication on HRV in early sepsis. We hypothesized that the use of cardiovascular medication increases HRV in septic patients, which may thereby lead to an underestimation of the severity of illness in these patients.
Methods
Study Design and Setting
This study is an exploratory post-hoc analysis of the SepsiVit study in adult non-trauma patients presenting with fever, (suspected) infection, or (early) sepsis at the ED of the University Medical Centre Groningen (UMCG), a tertiary care teaching hospital with over 34.000 ED visits annually [4]. We aimed to determine whether HRV measurements can provide an early warning for deterioration in patients with early sepsis presenting at the ED. Therefore, ECG, heart rate, blood pressure, respiratory rate, and oxygen saturation were continuously recorded during the first 48 h of hospital admission [4].
Study Population and Protocol
The protocol of the SepsiVit study was published before [4]. In short, eligible patients visiting the ED of the UMCG between 8 a.m. and 11 p.m. were recruited for the study. Adult patients suspected for early sepsis were included. Early sepsis was defined as the presence of an infection and at least two Systemic Inflammatory Response Syndrome (SIRS) criteria: body temperature < 36 °C or > 38 °C, heart rate > 90/min, respiratory rate > 20/min or PaCO2 < 4.3 kPa, or leukocytes < 4,000/mm3 or > 12,000/mm3 [19]. Exclusion criteria were known pregnancy, cardiac transplantation or no admission at our hospital after triage at the ED.
Eligible patients were equipped with a mobile patient monitor (Philips IntelliVue MP70 System with Multi-Measurement Module; Philips, Eindhoven, The Netherlands) which continuously recorded vital signs (ECG, heart rate, respiratory rate, oxygen saturation, and blood pressure every 4 hours) during the first 48 hours of admission. Only the first 3 hours at the ED were used for this analysis, with the assumption that the influence of medication is more significant during this time, while later on, advanced treatment may confound HRV measurements. Furthermore, more complete inclusions were realized during the first 3 hours.
In addition, we collected data on patient characteristics, prescription drug usage, treatment parameters, and vital signs measurements (blood pressure, heart rate, temperature, respiratory rate) every 30 min during the stay at the ED and follow-up during hospital admission [4].
Data Integration
Raw 500 Hz ECG data captured by the monitor were pre-processed prior to analysis. Pre-processing the raw ECG data is extensively discussed in the SepsiVit protocol by Quinten et al. [4, 20]. In short, noise was filtered out of the raw signal, non-sinus rhythm ectopic beats were corrected and the R-peaks were detected in the resulting signal. The pre-processing and analysis of HRV were performed by an automated algorithm implemented in MATLAB R2018a (The MathWorks Inc., Natick, MA, USA). The ECG data in the first 3 hours were used to calculate HRV parameters in time and frequency domains (Table 1). Patients with insufficient measurement time, < 3 hours, were excluded.
Statistical Analysis
HRV was compared between four subgroups: patients using [1] medication with direct effect on cardiac contractility, [2] medication with indirect effect on cardiac contractility, [3] medication from both groups, with direct and indirect effect on cardiac contractility, and [4] no cardiovascular medication.
Medication with direct effect on cardiac contractility was defined as usage of ß-blockers and/or digoxin. Medication with indirect effect on cardiac contractility was defined as usage of RAS-inhibitors, dihydropyridines, and/or diuretics. Patients using medication from both of these categories were classified into group 3. If none of this medication was used, patients were classified into the group using no cardiovascular medication.
Continuous data are presented as mean ± standard deviation or median [interquartile range] in case of skewed distribution. Categorical data are presented as total numbers (percentages). Differences among the four groups were analyzed using one-way ANOVA for normally distributed continuous data and Kruskal–Wallis for skewed data. Categorical data were analyzed with a Chi-square test. A two-sided p-value of ≤ 0.05 was considered statistically significant. In the case of significance, groupwise comparison was conducted. The Mann–Whitney U test was used for skewed continuous data for each group combination, and the Chi-square test was employed for categorical data. Bonferroni correction was used to correct the p-values for multiple testing. All statistical analyzes were performed using SPSS Statistics (version 28, SPSS Inc., Chicago, IL, USA).
Results
Study Population
Between January 2017 and December 2018, 171 patients were included in the SepsiVit study. Sixteen patients were excluded because of insufficient measurement time (less than 3 hours). The data from the remaining 155 patients were used in the final analysis (Fig. 1).
Of these 155 patients, 72.9% presented with sepsis and 2.6% with septic shock. Sepsis severity was classified as infection in 24.5% of the patients, involving patients who demonstrated clinical signs of infection without a clearly identified focus. The overall population’s median age was 65 years [52–75 years], and 54.8% were male (Table 2). Most common comorbidities were diabetes mellitus (26.5%), history of organ transplantation (25.2%), and malignancy (32.9%) (Table 2). In 9.0% of the patients, medication directly impacting cardiac contractility was administered, while 22.6% received medication with an indirect effect. A combination of both types of medication was prescribed to 17.4% of the patients. The majority of patients (51.0%) did not use any cardiovascular medication. Patients using both medication with direct and indirect effect were on average10 years older than patients using no cardiovascular medication (p 0.037). After pairwise comparison of the comorbidities diabetes mellitus, chronic renal insufficiency, and organ transplantation, no significant results were found.
Effects of Cardiovascular Medication on Vital Signs
Table 3 presents data about vital signs, stratification scores, organ failure development, hospital/ICU admission, and mortality. Nonetheless, no significant differences were observed among these variables across the four groups.
Table 4 shows the correlation between drug dose and vital signs. Dosage of beta-blockers and heart rate are negatively correlated. SBP, diastolic blood pressure (DBP), and MAP are positively correlated with the dosage of dihydropyridines (Table 4).
Effects of Cardiovascular Medication on HRV
HRV parameters were compared between patients with and without prescription of t medication with direct or indirect effect on cardiac contractility (Table 5). After pairwise comparison of VLF, no significant differences were found between the four groups. Dosage of beta-blockers and AVNN was positively correlated, while dosage of beta-blockers and LF/HF ratio was negatively correlated (Table 4).
Discussion
The current study is a subanalysis of the SepsiVit study, which showed that continuous HRV measurement can provide an early warning for deterioration in patients with an infection and sepsis presenting at the ED. Here, we aimed to gain more insight into the influence of cardiovascular medication on HRV. We found that medication with direct or indirect effect on cardiac contractility had no significant impact on vital signs or HRV parameters.
Effects of cardiovascular medication on vital signs and HRV parameters
Our study revealed that cardiovascular medication had no impact on vital signs or HRV parameters. No effect on heart rate is remarkable based on the pharmacodynamics of beta-blockers, especially blockage of the ß1-receptors lowers the heart rate and is expected to increase the AVNN [23, 24]. We found a positive correlation between the dosage of dihydropyridines and SBP, DBP, and MAP. Based on the pharmacodynamics a lower blood pressure would be expected [25].
Previous studies showed a higher VLF in MODS patients using beta-blockers or RAS-inhibitors [8, 13]. Our study could not confirm these results, probably because the study population is different. Patients presenting at the ED with infection or (early) sepsis appear to be less severely ill than ICU patients, in general. Furthermore, 72.9% of our patients were in an early septic stage rather than having sepsis or MODS. Besides that, VLF is best monitored over 24 hours. However, only the first 3 hours of measurement were used in this analysis, which implies that our time window may have been too short to identify the effect on VLF [26].
The effect of dihydropyridines and diuretics on HRV was, to the best of our knowledge, not previously investigated in septic patients. Also, Sahin et al. did not find any significant changes in HRV parameters in patients using amlodipine prescribed because of previously untreated essential hypertension [10]. Zaliunas et al. found a lower VLF, LF (norm), HF norm, and LF/HF ratio in patients with stable angina pectoris, atrial hypertension, and isolated left ventricular diastolic dysfunction using amlodipine [14]. Furthermore, in the same study, a lower VLF, LF, and HF in patients using lacidipine were found [14]. Patients with end stage renal disease using spironolactone showed a significantly higher SDNN [15]. A significantly lower HF was found in patients with congestive heart failure using spironolactone [18]. We could not confirm this result in our study.
Non-pharmacological factors influencing HRV parameters
HRV is influenced by many factors, which have to be considered when analyzing and modelling the effect of cardiovascular medication on HRV. One of the factors influencing HRV is age; a higher age leads to a lower HRV [27]. Patients using both medication with direct and indirect effect on cardiac contractility were on average 10 years older in contrast to patients using no cardiovascular medication. So, one might expect a lower HRV in this group [27]. However, our results showed no differences in HRV parameters.
Another factor influencing HRV is cardiac disease [28]. Patients surviving an acute myocardial infarction showed an increased LF norm and a diminished HF norm [28]. In contrast, our findings indicated no significant alterations in LF norm or HF norm, even when comparing groups with and without cardiovascular medication. Buttà et al. demonstrated the influence of several comorbidities on HRV, including among others obesity, pneumonia, dysthyroidism, ischemic stroke, and arterial hypertension [12]. Patients with several comorbidities were included in our study, which is representative for patients presenting at the ED with fever or suspected infection and/or sepsis.
Technical and clinical implications
Before this study, HRV in septic patients has been primarily studied in ICU patients [4]. Our SepsiVit study showed that long-term, automatically analyzed ECG recordings can be used to determine HRV features that are associated with clinical deterioration of early septic patients at the ED [20]. The results of this current subanalysis indicate that the use of cardiovascular medication is not associated with changes in HRV in the early sepsis ED population. Correcting HRV measurements for cardiovascular medication seems to be unnecessary, however may still be relevant in a different setting and population. Recommendations for further research are to analyze the influence of more different types of medication and polypharmacy on HRV in septic patients at the ED. Thereby, it would be interesting to assess the diagnostic accuracy of potential screening tools utilizing HRV features, for detecting patient deterioration in septic patients at the ED and to examine the influence of cardiovascular medication on this interpretation.
Strengths and Limitations
Our study is the first observational study analyzing the influence of cardiovascular medicine on HRV in patients with early sepsis at the ED [4]. The inclusion criteria of the current study were based on sepsis-2 definitions [19], instead of the sepsis-3 definitions that were introduced in 2016 [29]. This allowed to include a heterogeneous population with a severe infection at risk for deterioration, which represents a real-world population at the ED. We used the first three hours of data at the ED, since later on advanced treatment (e.g., vasopressors, inotropics) may confound HRV measurements. Our study had several limitations: First, the study focuses on the use of cardiovascular medication, while HRV is influenced by many factors, including demographic factors (e.g., age, sex) and comorbidities. Second, the current study was a single-center study in a tertiary care teaching hospital with the referral of patients for academic specialist care, which may limit its generalizability.
Conclusion
Our results showed that HRV is not influenced by cardiovascular medication in patients presenting with early sepsis at the ED. Consequently, the correction of HRV features for the use of cardiovascular medication is unnecessary when analyzing, modelling, and interpreting these signals.
Data Availability
Data is available upon reasonable request.
Code Availability
Upon reasonable request.
Abbreviations
- AVNN :
-
Average of all NN intervals
- CV :
-
Coefficient of variation of the NN-intervals
- DBP :
-
Diastolic blood pressure
- ED :
-
Emergency department
- HF norm :
-
Normalized high frequency power
- HRV :
-
Heart rate variability
- ICU :
-
Intensive Care Unit
- LF norm :
-
Normalized low frequency power
- LF/HF ratio :
-
Ratio between low and high frequency power
- MAP :
-
Mean arterial pressure
- MODS :
-
Multi Organ Dysfunction Syndrome
- RAS :
-
Renin-angiotensin system
- SBP :
-
Systolic blood pressure
- SDNN :
-
Standard deviation of the NN intervals
- SIRS :
-
Systemic Inflammatory Response Syndrome
- UMCG :
-
University Medical Center Groningen
- VLF :
-
Very low frequency
References
Quinten VM, van Meurs M, ter Maaten JC, Ligtenberg JJM. Trends in vital signs and routine biomarkers in patients with sepsis during resuscitation in the emergency department: a prospective observational pilot study. BMJ Open. 2016;6(5):1–9.
Seely AJE, Macklem PT. Complex systems and the technology of variability analysis. Crital Care. 2004;8(6):367–84.
Acharya UR, Joseph KP, Kannathal N, Lim CM, Suri JS. Heart rate variability: a review. Med Biol Eng Comput. 2006;44(12):1031–51.
Quinten VM, Meurs van M, Renes MH, Ligtenberg JJM. Protocol of the SepsiVit study : A prospective observational study to determine whether continuous heart rate variability measurement during the first 48 hours of hospitalization provides an early warning for deterioration in patients presenting with infection or sepsis to the emergency department of a Dutch academic teaching hospital. BMJ Open. 2017;7(11):e018259.
Barnaby DP, Fernando SM, Ferrick KJ, Herry CL, Seely AJE, Bijur PE, et al. Use of the low-frequency/high-frequency ratio of heart rate variability to predict short-term deterioration in emergency department patients with sepsis. Emergency Med J. 2017;0:1–8.
Barnaby PBF, Herry SM, Scales CL, Gallangher NB, AJE EJS. Heart rate variability, clinical and laboratory measures to predict future deterioration in patients presenting with sepsis. Shock Soc. 2019;51(4):416–22.
Liu N, Prabhakar SM, Chong S-L, Lye WK, Koh ZX, Guo D, et al. A novel heart rate variability based risk prediction model for septic patients presenting to the emergency department. 2018;97(23):e10866.
Werdan K, Schmidt H, Ebelt H, Zorn-Pauly K, Koidl B, Hoke RS, et al. Impaired regulation of cardiac function in sepsis, SIRS, and MODS. This article is one of a selection of papers from the NATO Advanced Research Workshop on Translational Knowledge for Heart Health (Published in part 2 of a 2-part Special Issue). Can J Physiol Pharmacol. 2009;87(4):266–74.
Taçoy G, Balcioğlu AS, Arslan U, Durakoğlugil E, Erdem G, Ozdemir M, et al. Effect of metoprolol on heart rate variability in symptomatic patients with mitral valve prolapse. Am J Cardiol. 2007;99(11):1568–70.
Sahin I, Kosar F, Altunkan S, Günaydin M. Comparison of the effects of amlodipine and verapamil on autonomic activity in hypertensive patients. Eur J Intern Med. 2004;15(4):225–30.
Heusser K, Vitkovsky J, Schmieder RE, Schobel HP. AT1 antagonism by eprosartan lowers heart rate variability and baroreflex gain. Auton Neurosci. 2003;107(1):45–51.
Buttà C, Tuttolomondo A, Casuccio A, Petrantoni R, Miceli G, Cuttitta F, et al. Relationship between HRV measurements and demographic and clinical variables in a population of patients with atrial fibrillation. Heart Vessels. 2016;31(12):2004–13.
Hennen R, Friedrich I, Hoyer D, Nuding S, Rauchhaus M, Schulze M, et al. Autonome dysfunktion und betablocker beim multiorgandysfunktionssyndrom. DMW - Deutsche Medizinische Wochenschrift. 2008;133(48):2500–4.
Žaliūnas R, Braždžionytė J, Zabiela V, Jurkevičius R. Effects of amlodipine and lacidipine on heart rate variability in hypertensive patients with stable angina pectoris and isolated left ventricular diastolic dysfunction. Int J Cardiol. 2005;101(3):347–53.
Eklund M, Hellberg O, Furuland H, Cao Y, Nilsson E. Effects of spironolactone on extrasystoles and heart rate variability in haemodialysis patients: A randomised crossover trial. Ups J Med Sci. 2021;126(1):e5660.
Lin C, Zhang Q, Zhang H, Lin A. Long-term effects of low-dose spironolactone on chronic dialysis patients: a randomized placebo-controlled study. J Clinical Hypertension. 2016;18(2):121–8.
Flevari P, Kalogeropoulou S, Drakou A, Leftheriotis D, Panou F, Lekakis J, et al. Spironolactone improves endothelial and cardiac autonomic function in non heart failure hemodialysis patients. J Hypertens. 2013;31(6):1239–44.
Yee KM, Pringle SD, Struthers AD. Circadian variation in the effects of aldosterone blockade on heart rate variability and QT dispersion in congestive heart failure. J Am Coll Cardiol. 2001;37(7):1800–7.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003;31(4):530–8.
van Wijk RJ, Quinten VM, van Rossum MC, Bouma HR, Ter Maaten JC. Predicting deterioration of patients with early sepsis at the emergency department using continuous heart rate variability analysis: a model-based approach. Scand J Trauma Resusc Emerg Med. 2023;31(1):15.
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, et al. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2(1):1–138.
Burt CC, Arrowsmith JE. Respiratory failure. Surg Infect (Larchmt). 2009;27(11):475–9.
Farmacotherapeutisch kompas. Bètablokkers, systemisch. Internet site farmacotherapeutisch kompas 2020. Available: https://www.farmacotherapeutischkompas.nl/bladeren/groepsteksten/betablokkers__systemisch. Accessed 8 Apr 2020.
Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health. 2017;28:5.
Farmacotherapeutisch kompas. Dihydropyridinen. Internet site farmacotherapeutisch Kompas. 2020. Available: https://www.farmacotherapeutischkompas.nl/bladeren/groepsteksten/dihydropyridinen#dihydropyridinen_werking. Accessed 8 Apr 2020.
Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health. 2017;5(September):1–17.
Valentini M, Parati G. Variables influencing heart rate. Prog Cardiovasc Dis. 2009;52(1):11–9.
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability guidelines. Eur Heart J. 1996;17:354–81.
Singer M, Deutschman CS, Seymour C, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA - J Am Med Assoc. 2016;315(8):801–10.
Acknowledgements
The authors thank the nurses, students, and physicians in the ED for their assistance during the acquisition of the data.
Funding
This study is funded by the emergency department of the University Medical Center Groningen.
Author information
Authors and Affiliations
Contributions
LvdL participated in data acquisition, analyzed data, and drafted the manuscript. RJvW participated in data acquisition, analyzed data, and revised the manuscript. VMQ designed the study and assisted with data acquisition and data analysis. HRB assisted with data interpretation and revised the manuscript. JCtM supervised the study, participated in the study design, assisted with data interpretation, revised the manuscript, and has given final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics Approval
The study was performed in the University Medical Centre Groningen (UMCG, Groningen, the Netherlands), a tertiary care teaching hospital and approved by the institutional review board of the UMCG (METC 2015/164). The protocol of the study was published by us previously [4].
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Patients signed informed consent regarding publishing their anoymized data.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Laan, L., van Wijk, R.J., Quinten, V.M. et al. The Effect of Cardiovascular Medication on Heart Rate Variability in Patients Presenting with Early Sepsis at the Emergency Department: A Prospective Cohort Study. SN Compr. Clin. Med. 6, 30 (2024). https://doi.org/10.1007/s42399-024-01656-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-024-01656-8