Abstract
Background/Aim
The aim of the study was to evaluate serum calprotectin (CLP) levels in familial Mediterranean fever (FMF) patients and to investigate the utility of CLP in distinguishing patients with attack from patients without attack.
Material and method
FMF patients, rheumatoid arthritis (RA) patients, and healthy controls were included. Serum calprotectin levels were quantified utilizing the enzyme-linked immunosorbent assay (ELISA) method. Receiver operating characteristic (ROC) curve analysis was used to identify the cut-off value of serum CLP level to differentiate FMF patients with attack from those without. Logistic regression analysis was performed to identify predictors.
Results
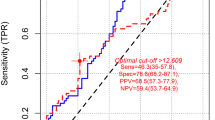
Significant differences were observed among the three groups concerning white blood cell (WBC), neutrophil, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and serum CLP levels (p = 0.003, p = 0.004, p < 0.001, p < 0.001, and p = 0.002, respectively). Higher ESR, CRP, and serum CLP levels were observed in FMF patients with attacks than those without (all, p < 0.001). Serum CLP was significantly higher in RA patients than in FMF patients in remission (p < 0.001). ROC analysis identified a threshold CLP concentration in FMF with an attack to be 47.1 pg/mL (83.3% sensitivity, 60.6% specificity, AUC = 0.74, 95% CI = 0.63–0.85, p < 0.001). In univariate logistic regression analysis, CLP (β = 1.045, 95% CI = 1.017–1.073, p = 0.001) was predictive of FMF patients experiencing an attack.
Conclusion
Serum CLP proves to be as productive as ESR in illustrating inflammation and demonstrating the existence of attacks in FMF patients.


Similar content being viewed by others
Data availability
The data from this study are available with the corresponding author and will be provided upon a reasonable request, subject to approval from the institute's ethics committee.
References
Gucenmez OA, Kume T, Makay B et al (2018) Role of fecal calprotectin in the assessment of intestinal inflammation in children with familial Mediterranean fever. Int J Rheum Dis 21:1844–1848. https://doi.org/10.1111/1756-185X.13396
Yalçınkaya F, Özen S, Özçakar Z et al (2009) A new set of criteria for the diagnosis of familial Mediterranean fever in childhood. Rheumatology 48(4):395–398
Korkmaz C, Özdogan H, Kasapçopur Ö et al (2002) Acute phase response in familial Mediterranean fever. Ann Rheum Dis 61(1):79–81
Lachmann H, Şengül B, Yavuzşen TU et al (2006) Clinical and subclinical inflammation in patients with familial Mediterranean fever and in heterozygous carriers of MEFV mutations. Rheumatology 45(6):746–750. https://doi.org/10.1093/rheumatology/kei279
Shohat M, Halpern GJ (2011) Familial Mediterranean fever a review. Genet Med 13(6):487–498
Chae JJ, Aksentijevich I, Kastner DL (2009) Advances in the understanding of familial Mediterranean fever and possibilities for targeted therapy. Br J Haematol 146:467–478. https://doi.org/10.1111/J.1365-2141.2009.07733.X
Gumucio DL, Diaz A, Schaner P et al (2002) Fire and ICE: the role of pyrin domain-containing proteins in inflammation and apoptosis. Clin Exp Rheumatol 20(4; SUPP/26):45–53
Chae J, Wood G, Richard K et al (2008) The familial Mediterranean fever protein, pyrin, is cleaved by caspase-1 and activates NF-κB through its N-terminal fragment. The Journal of the American Society of Hematology 112(5):1794–1803
Nishikawa Y, Kajiura Y, Lew JH et al (2017) Calprotectin induces IL-6 and MCP-1 production via toll-like receptor 4 signaling in human gingival fibroblasts. J Cell Physiol 232:1862–1871. https://doi.org/10.1002/jcp.25724
Garcia V, Perera Y, Biomolecules WC et al (2022) A structural perspective on calprotectin as a ligand of receptors mediating inflammation and potential drug target. Biomolecules 12(4):519
Kopeć-Mędrek M, Widuchowska M, Kucharz EJ (2016) Calprotectin in rheumatic diseases: a review. Reumatologia 54(6):306. https://doi.org/10.5114/reum.2016.64907
Kılıçaslan E, Düzenli T, Çelik S et al (2022) Assessment of serum resistin and plasma calprotectin levels as biomarkers of ınflammation in patients with familial Mediterranean fever disease. Mediterr J Rheumatol 33:322. https://doi.org/10.31138/MJR.33.3.322
Asan G, Derin ME, Doğan HO et al (2020) Can calprotectin show subclinical inflammation in familial Mediterranean fever patients. J Korean Med Sci 35(10):e63. https://doi.org/10.3346/jkms.2020.35.e63
Dzhndoian Z (2012) Serum levels of myeloıd-related proteın Mrp 8/14 (calprotectın) ın Armenıan patıents wıth famılıal Medıterranean fever (FMF). Ter Arkh 84(6):45–48
Holzinger D, Roth J (2016) Alarming consequences–autoinflammatory disease spectrum due to mutations in proline-serine-threonine phosphatase-interacting protein 1. Rheumatology J 28(5):550–559. https://doi.org/10.1097/BOR.0000000000000314
Jorch SK, McNally A, Berger P et al (2023) Complex regulation of alarmins S100A8/A9 and secretion via gasdermin D pores exacerbates autoinflammation in familial Mediterranean fever. J Allergy Clin Immunol 152:230–243. https://doi.org/10.1016/J.JACI.2023.01.03
Neogi T, Aletaha D, Silman AJ et al (2010) The 2010 American College of Rheumatology/European League Against Rheumatism classification criteria for rheumatoid arthritis: phase 2 methodological report. Arthritis Rheum 62:2582–2591. https://doi.org/10.1002/ART.27580
Kalla R, Kennedy NA, Ventham NT et al (2016) Serum calprotectin: a novel diagnostic and prognostic marker in inflammatory bowel diseases. Am J Gastroenterol Suppl. 111(12):1796–1805. https://doi.org/10.1038/ajg.2016.342
Unal I (2017) Defining an optimal cut-point value in ROC analysis: an alternative approach. Comput Math Methods Med 2017:3762651. https://doi.org/10.1155/2017/3762651
Fangyu L, Hua H (2018) Assessing the accuracy of diagnostic tests. Shanghai Arch Psychiatry 30(3):207
Jung S, Park Y, Ha Y et al (2006) Serum calprotectin as a marker for disease activity and severity in adult-onset Still’s disease. J Rheumatol 8(3):1–12
Arias MG, Pascual-Salcedo D, Ueberschlag M-E et al (2013) Calprotectin in rheumatoid arthritis: association with disease activity in a cross-sectional and a longitudinal cohort. Mol Diagn Ther 17:49–56. https://doi.org/10.1007/s40291-013-0016-9
Oktayoglu P, Bozkurt M, Mete N et al (2014) Elevated serum levels of calprotectin (myeloid-related protein 8/14) in patients with ankylosing spondylitis and its association with disease activity and quality of life. J Investig Med 62:880–884. https://doi.org/10.1097/JIM.0000000000000095
Inciarte-Mundo J, Ramirez J, Hernández MV et al (2016) Calprotectin and TNF trough serum levels identify power Doppler ultrasound synovitis in rheumatoid arthritis and psoriatic arthritis patients in remission or with low disease activity. Arthritis Res Ther 8(1):160. https://doi.org/10.1186/S13075-016-1032-Z
Nordal HH, Brun JG, Halse AK et al (2014) Calprotectin (S100A8/A9), S100A12, and EDTA-resistant S100A12 complexes (ERAC) in primary Sjögren’s syndrome Scandinavian. J Rheumatol 43(1):76–78. https://doi.org/10.3109/03009742.2013.848930
Frosch M, Ahlmann M, Vogl T et al (2009) The myeloid-related proteins 8 and 14 complex, a novel ligand of toll-like receptor 4, and interleukin-1β form a positive feedback mechanism in systemic-onset juvenile idiopathic arthritis. Arthritis Rheum 60:883–891. https://doi.org/10.1002/ART.24349
Haga HJ, Brun JG, Berntzen HB et al (1993) Calprotection in patients with systemic lupus erythematosus: relation to clinical and laboratory parameters of disease activity. Lupus 2:47–50. https://doi.org/10.1177/096120339300200108
Demirbaş F, Çaltepe G, Comba A et al (2019) Fecal calprotectin in children with familial Mediterranean fever in the attack-free period. Pediatr Int 61:1140–1145. https://doi.org/10.1111/PED.13995
Tezcan D, Onmaz DE, Sivrikaya A et al (2023) Assessment of serum neopterin and calprotectin as biomarkers for subclinical inflammation in patients with familial Mediterranean fever. Ir J Med Sci 192:2015–2022. https://doi.org/10.1007/s11845-022-03173-w/fıgures/1
Bae SC, Lee YH (2017) Calprotectin levels in rheumatoid arthritis and their correlation with disease activity: a meta-analysis. Postgrad Med 129:531–537. https://doi.org/10.1080/00325481.2017.1319729
Jarlborg M, Courvoisier DS, Lamacchia C et al (2020) Serum calprotectin: a promising biomarker in rheumatoid arthritis and axial spondyloarthritis. Arthritis Res Ther 22:1–11. https://doi.org/10.1186/s13075-020-02190-3/tables/4
Funding
This study was funded by the Research Fund of the Ankara Bilkent City Hospital which had no involvement in the design, collection analyses, or reporting of the study (trial project coordination unit. No: 2016/1208).
Author information
Authors and Affiliations
Contributions
MGP, AO, MFK, and SOK contributed to the study design. MGP, AO, and SOK collected the data. NG analyzed the data and took responsibility for the accuracy of the data analysis. MGP, AO, and NG interpreted the data and drafted the manuscript. MGP, AO, and NG critically revised the manuscript for important contents. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Polat, M.G., Omma, A., Gokcen, N. et al. Role of serum calprotectin in identifying familial Mediterranean fever attacks. Ir J Med Sci (2024). https://doi.org/10.1007/s11845-024-03659-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11845-024-03659-9