Abstract
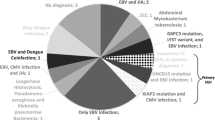
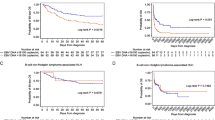
Visceral leishmaniasis-associated hemophagocytic lymphohistiocytosis (VL-HLH) is indistinguishable from those of HLH of other etiologies due to the overlap symptoms, posing a serious threat to life. In this study, we aimed to provide insights for early diagnosis and improve outcomes in pediatric patients with VL-HLH. We retrospectively analyzed the clinical and laboratory data of 10 pediatric patients with VL-HLH and 58 pediatric patients with Epstein–Barr virus-associated hemophagocytic lymphohistiocytosis (EBV-HLH). The median time from symptom onset to cytopenia in patients with VL-HLH and EBV-HLH was 11 days (interquartile range, 7–15 days) and five days (interquartile range, 3.75–9.25 days) (P = 0.005). Both groups showed liver injury and increased lactate dehydrogenase levels; however the levels of aspartate aminotransferase, alanine aminotransferase, direct bilirubin, and lactate dehydrogenase in patients with VL-HLH were significantly lower than those in patients with EBV-HLH (P < 0.05). The fibrinogen and triglyceride levels were almost normal in VL-HLH patients but were significantly altered in EBV-HLH cases ( P < 0.05). The positive rate of first bone marrow microscopy examination, anti-rK39 IgG detection, and blood metagenomic next-generation sequencing was 50%, 100%, and 100%, respectively. After VL diagnosis, eight patients were treated with sodium stibogluconate and two were treated with liposomal amphotericin B. All the patients with VL-HLH recovered. Our study demonstrates that regular triglyceride and fibrinogen levels in pediatric patients with VL-HLH may help in differential diagnosis from EBV-HLH. VL-HLH is milder than EBV-HLH, with less severe liver injury and inflammatory responses, and timely treatment with antileishmanial agents is essential to improve the outcomes of pediatric patients with VL-HLH.


Similar content being viewed by others
References
Al-Samkari H, Berliner N (2018) Hemophagocytic Lymphohistiocytosis. Annu Rev Pathol 13:27–49. https://doi.org/10.1146/annurev-pathol-020117-043625
Bolia R, Singh A, Maji M, Misra M, Sharawat IK, Panda PK (2021) Visceral Leishmaniasis Associated with Hemophagocytic Lymphohistiocytosis. Indian J Pediatr 88:73. https://doi.org/10.1007/s12098-020-03361-5
Scarpini S, Dondi A, Totaro C, Biagi C, Melchionda F, Zama D et al (2022) Visceral leishmaniasis: epidemiology, diagnosis, and treatment regimens in different geographical areas with a focus on pediatrics. Microorganisms 10:1887. https://doi.org/10.3390/microorganisms10101887
Guan Z, Chen C, Huang C, Zhang H, Zhou Y, Zhou Y et al (2021) Epidemiological features and spatial-temporal distribution of visceral leishmaniasis in mainland China: a population-based surveillance study from 2004 to 2019. Parasit Vectors 14:517. https://doi.org/10.1186/s13071-021-05002-y
Blazquez-Gamero D, Dominguez-Pinilla N, Chicharro C, Negreira S, Galan P, Perez-Gorricho B et al (2015) Hemophagocytic lymphohistiocytosis in children with visceral leishmaniasis. Pediatr Infect Dis J 34:667–669. https://doi.org/10.1097/INF.0000000000000685
Shi Q, Huang M, Li X, Zheng X, Wang F, Zou Y et al (2021) Clinical and laboratory characteristics of hemophagocytic lymphohistiocytosis induced by Leishmania infantum infection. PLoS Negl Trop Dis 15:e9944. https://doi.org/10.1371/journal.pntd.0009944
Bode SFNM, Bogdan CM, Beutel KM, Behnisch WM, Greiner JM, Henning SM et al (2014) Hemophagocytic Lymphohistiocytosis in Imported Pediatric Visceral Leishmaniasis in a nonendemic area. J Pediatr 165:147–153. https://doi.org/10.1016/j.jpeds.2014.03.047
Lun Z, Wu M, Chen Y, Wang J, Zhou X, Liao L et al (2015) Visceral leishmaniasis in China: an endemic disease under control. Clin Microbiol Rev 28:987–1004. https://doi.org/10.1128/CMR.00080-14
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S et al (2007) HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 48:124–131. https://doi.org/10.1002/pbc.21039
El Mallawany NK, Curry CV, Allen CE (2022) Haemophagocytic lymphohistiocytosis and Epstein–Barr virus: a complex relationship with diverse origins, expression and outcomes. Brit J Haematol 196:31–44. https://doi.org/10.1111/bjh.17638
Scalzone M, Ruggiero A, Mastrangelo S, Trombatore G, Ridola V, Maurizi P et al (2016) Hemophagocytic lymphohistiocytosis and visceral leishmaniasis in children: case report and systematic review of literature. J Infect Dev Countr 10:103–108. https://doi.org/10.3855/jidc.6385
Mottaghipisheh H, Kalantar K, Amanati A, Shokripour M, Shahriari M, Zekavat OR et al (2021) Comparison of the clinical features and outcome of children with hemophagocytic lymphohistiocytosis (HLH) secondary to visceral leishmaniasis and primary HLH: a single-center study. BMC Infect Dis 21. https://doi.org/10.1186/s12879-021-06408-w
Jordan MB, Allen CE, Greenberg J, Henry M, Hermiston ML, Kumar A et al (2019) Challenges in the diagnosis of hemophagocytic lymphohistiocytosis: recommendations from the North American Consortium for Histiocytosis (NACHO). Pediatr Blood Cancer 66. https://doi.org/10.1002/pbc.27929
Colomba C, Di Carlo P, Scarlata F, Iaria C, Barberi G, Fama F et al (2016) Visceral leishmaniasis, hypertriglyceridemia and secondary hemophagocytic lymphohistiocytosis. Infection 44:391–392. https://doi.org/10.1007/s15010-016-0881-3
Valade S, Mariotte E, Azoulay E (2020) Coagulation disorders in Hemophagocytic Lymphohistiocytosis/Macrophage activation syndrome. Crit Care Clin 36:415–426. https://doi.org/10.1016/j.ccc.2019.12.004
Valade S, Azoulay E, Galicier L, Boutboul D, Zafrani L, Stepanian A et al (2015) Coagulation disorders and bleedings in critically ill patients with Hemophagocytic Lymphohistiocytosis. Medicine 94:e1692. https://doi.org/10.1097/MD.0000000000001692
Esmaeeli S, Hoseinirad SM, Rajabian M, Taheri AR, Berenji F, Hashemy SI (2019) Evaluation of the oxidant-antioxidant balance, isoprostane and quantitative CRP in patients with cutaneous leishmaniasis. Microb Pathog 137:103738. https://doi.org/10.1016/j.micpath.2019.103738
López Marcos M, Ruiz Sáez B, Vílchez Pérez JS, Moreno Pérez D, Carazo Gallego B, Falcón Neyra L et al (2021) Distinct laboratory and clinical features of secondary hemophagocytic lymphohistiocytosis in Pediatric Visceral Leishmaniasis. Pediatr Infect Dis J 40:525–530. https://doi.org/10.1097/INF.0000000000003086
Mantovani A, Garlanda C (2023) Humoral innate immunity and Acute-Phase proteins. N Engl J Med 388:439–452. https://doi.org/10.1056/NEJMra2206346
Koubâa M, Mâaloul I, Marrakchi C, Mdhaffar M, Lahiani D, Hammami B et al (2012) Hemophagocytic syndrome associated with visceral leishmaniasis in an immunocompetent adult—case report and review of the literature. Ann Hematol 91:1143–1145. https://doi.org/10.1007/s00277-011-1367-0
Gagnaire MH, Galambrun C, Stephan JL (2000) Hemophagocytic syndrome: a misleading complication of visceral leishmaniasis in children–a series of 12 cases. Pediatrics 106:E58. https://doi.org/10.1542/peds.106.4.e58
Guo F, Kang L, Xu M (2020) A case of pediatric visceral leishmaniasis-related hemophagocytic lymphohistiocytosis diagnosed by mNGS. Int J Infect Dis 97:27–29. https://doi.org/10.1016/j.ijid.2020.05.056
Oliva G, Scalone A, Foglia Manzillo V, Gramiccia M, Pagano A, Di Muccio T, Gradoni L (2006) Incidence and time course of Leishmania infantum infections examined by parasitological, serologic, and nested-PCR techniques in a cohort of naive dogs exposed to three consecutive transmission seasons. J Clin Microbiol 44(4):1318–1322. https://doi.org/10.1128/JCM.44.4.1318-1322.2006PMID: 16597857; PMCID: PMC1448675
Aronson N, Herwaldt BL, Libman M, Pearson R, Lopez-Velez R, Weina P et al (2016) Diagnosis and treatment of Leishmaniasis: clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis 63:e202–e264. https://doi.org/10.1093/cid/ciw670
Krepis P, Argyri I, Krepi A, Syrmou A, Spyridis N, Tsolia M (2017) Short-course regimens of liposomal amphotericin B for the treatment of Mediterranean visceral leishmaniasis in children: an 11-year Retrospective Study at a Tertiary Care Center. Pediatr Infect Dis J 36:849–854. https://doi.org/10.1097/INF.0000000000001602
Krepis P, Krepi A, Argyri I, Aggelis A, Soldatou A, Papaevangelou V et al (2018) Childhood visceral leishmaniasis: distinctive features and diagnosis of a re-emerging Disease. An 11-year experience from a Tertiary Referral Center in Athens, Greece. Pediatr Infect Dis J 37:419–423. https://doi.org/10.1097/INF.0000000000001797
Funding
This research did not recieve any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Dao Wang: Conceptualization, Methodology, Supervision,
Yuanfang Li: Writing-Origial Draft, Formal analysis.
Sanjing Li: Resources, Methodology.
Nadan Lu: Investigation, Formal analysis.
Weilin Wang: Investigation, Formal analysis.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare.
Ethics approval
The study protocol was evaluated and approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University (approval number 2023-KY-0730). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Y., Li, S., Lu, N. et al. Secondary hemophagocytic lymphohistiocytosis in pediatric patients with visceral leishmaniasis and Epstein-Barr virus infection. Ann Hematol 103, 1541–1547 (2024). https://doi.org/10.1007/s00277-024-05695-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-024-05695-y