Abstract
Purpose
To investigate the relationship between blood lead levels (BLLs) and IVF clinical outcomes in infertile females and to further explore the possible involvement of granulosa cell (GC) endoplasmic reticulum (ER) stress in the process.
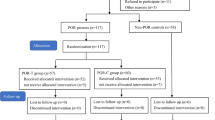
Methods
One hundred twenty-three infertile women undergoing IVF cycles were included in the current study. All participants were divided into three (low, medium, and high) groups determined by BLL tertiles. Gonadotropin releasing hormone (GnRH) agonist regimen for ovarian stimulation was used for all patients, with follicular fluids being collected on the day of oocyte retrieval. Lactate dehydrogenase (LDH) levels in follicular fluid and the endoplasmic reticulum stress-signaling pathway of granulosa cells (GCs) were examined.
Results
The oocyte maturation rate and high-quality embryo rate on cleaved stage decreased significantly as BLL increased. For lead levels from low to high, live birth rate (68.29%, 56.10%, 39.02%; P=0.028) showed negative correlations with BLLs. Also, follicular fluid Pb level and LDH level was significantly higher in the high lead group versus the low group. Binomial regression analysis revealed significant negative correlation between BLLs and live birth rate (adjusted OR, 0.38; 95% CI, 0.15–0.95, P=0.038). Further analysis of the endoplasmic reticulum stress (ER stress) signaling pathway of GCs found that expressions of GRP78, total JNK, phosphorylated JNK, and CHOP increased and BCL-2 decreased with increasing BLLs.
Conclusions
BLLs are negatively associated with final clinical outcomes in IVF patients that may be related to increased ER stress response and GC apoptosis. Thus, reducing Pb exposure before IVF procedures may improve final success rates.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMH:
-
anti-Mullerian hormone
- BCL-2:
-
B cell lymphoma-2
- BLL:
-
blood lead level
- BMI:
-
body mass index
- CDC:
-
Center for Disease Control and Prevention of US
- COH:
-
controlled ovarian hyperstimulation
- CHOP:
-
C/EBP homologous protein
- E2:
-
estrogen
- ER:
-
endoplasmic reticulum
- FF:
-
follicle fluid
- FSH:
-
follicular-stimulating hormone
- GRP78:
-
glucose regulated protein 78
- GnRH:
-
gonadotropin-releasing hormone
- GC:
-
granulosa cell
- Gn:
-
gonadotropins
- GM:
-
geometric mean
- ICSI:
-
intracytoplasmic sperm injection
- IQR:
-
median and interquartile range
- IVF:
-
in vitro fertilization
- JNK:
-
c-Jun N-terminal kinase
- LDH:
-
lactate dehydrogenase
- LH:
-
luteinizing hormone
- P:
-
progesterone
- PRL:
-
prolactin
- T:
-
testosterone
- WHO:
-
World Health Organization
References
Priya K, Setty M, Babu UV, Pai KSR. Implications of environmental toxicants on ovarian follicles: how it can adversely affect the female fertility? Environ Sci Pollut Res Int. 2021;28(48):67925–39.
CDC: Fourth National Report on Human Exposure to Environmental Chemicals. Centers for Disease Control and Prevention 2019; http://www.cdc.gov/exposurereport/ (updated tables, January 2019).
WHO: Lead poisoning and health [Online]. World Health Organization 2022; https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health.
Lei HL, Wei HJ, Ho HY, Liao KW, Chien LC. Relationship between risk factors for infertility in women and lead, cadmium, and arsenic blood levels: a cross-sectional study from Taiwan. BMC Public Health. 2015;15:1220.
Tolunay HE, Sukur YE, Ozkavukcu S, Seval MM, Ates C, Turksoy VA, Ecemis T, Atabekoglu CS, Ozmen B, Berker B, Sonmezer M. Heavy metal and trace element concentrations in blood and follicular fluid affect ART outcome. Eur J Obstet Gynecol Reprod Biol. 2016;198:73–7.
Chang SH, Cheng BH, Lee SL, Chuang HY, Yang CY, Sung FC, Wu TN. Low blood lead concentration in association with infertility in women. Environ Res. 2006;101(3):380–6.
Lamadrid-Figueroa H, Tellez-Rojo MM, Hernandez-Avila M, Trejo-Valdivia B, Solano-Gonzalez M, Mercado-Garcia A, Smith D, Hu H, Wright RO. Association between the plasma/whole blood lead ratio and history of spontaneous abortion: a nested cross-sectional study. BMC Pregnancy Childbirth. 2007;7:22.
Dearth RK, Hiney JK, Srivastava V, Les Dees W, Bratton GR. Low level lead (Pb) exposure during gestation and lactation: assessment of effects on pubertal development in Fisher 344 and Sprague-Dawley female rats. Life Sci. 2004;74(9):1139–48.
He Y, Wang L, Li X, Zhao H. The effects of chronic lead exposure on the ovaries of female juvenile Japanese quails (Coturnix japonica): developmental delay, histopathological alterations, hormone release disruption and gene expression disorder. Ecotoxicol Environ Saf. 2020;205:111338.
Pérez-Debén S, Gonzalez-Martin R, Palomar A, Quiñonero A, Salsano S, Dominguez F. Copper and lead exposures disturb reproductive features of primary endometrial stromal and epithelial cells. Reprod Toxicol. 2020;93:12.
Ou J, Peng P, Qiu L, Teng L, Li C, Han J, Liu X. Effect of Lead Exposure on Spontaneous Abortion: a Case-Control Study. Clin Lab. 2020;66(5):1–7.
Wide M, Nilsson BO. Interference of lead with implantation in the mouse- a study of the surface ultrastructure of blastocysts and endometrium. Teratology. 1979;20(1):101–13.
Bloom MS, Kim K, Kruger PC, Parsons PJ, Arnason JG, Steuerwald AJ, Fujimoto VY. Associations between toxic metals in follicular fluid and in vitro fertilization (IVF) outcomes. J Assist Reprod Genet. 2012;29(12):1369–79.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group Embryology. Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Reprod Biomed Online. 2011;22(6):632–46.
Wu S, Wang M, Deng Y, Qiu J, Zhang X, Tan J. Associations of toxic and essential trace elements in serum, follicular fluid, and seminal plasma with In vitro fertilization outcomes. Ecotoxicol Environ Saf. 2020;204:110965–77.
Li D, Liang C, Cao Y, Zhu D, Shen L, Zhang Z, Jiang T, Zhang Z, Zong K, Liu Y, et al. The associations of serum metals concentrations with the intermediate and pregnancy outcomes in women undergoing in vitro fertilization (IVF). Ecotoxicol Environ Saf. 2022;233:113309.
Foster WG, McMahon A, Rice DC. Subclinical changes in luteal function in cynomolgus monkeys with moderate blood lead levels. J Appl Toxicol. 1996;16(2):159–63.
Taupeau C, Poupon J, Nome F, Lefevre B. Lead accumulation in the mouse ovary after treatment-induced follicular atresia. Reprod Toxicol. 2001;15(4):385–91.
Nandi S, Gupta PS, Selvaraju S, Roy SC, Ravindra JP. Effects of exposure to heavy metals on viability, maturation, fertilization, and embryonic development of buffalo (Bubalus bubalis) oocytes in vitro. Arch Environ Contam Toxicol. 2010;58(1):194–204.
Wang D, Fu X, Zhang J, Xu C, Hu Q, Lin W. Association between blood lead level during pregnancy and birth weight: A meta-analysis. Am J Ind Med. 2020;63(12):1085–94.
Okubo H, Nakayama SF, Japan E, Children's Study G. Periconceptional maternal diet quality influences blood heavy metal concentrations and their effect on low birth weight: the Japan Environment and Children's Study. Environ Int. 2023;173:107808.
Pinon-Lataillade G, Thoreux-Manlay A, Coffigny H, Masse R, Soufir JC. Reproductive toxicity of chronic lead exposure in male and female mice. Hum Exp Toxicol. 1995;14(11):872–8.
Mariann W. NILSSON B: Interference of lead with implantation in the mouse: a study of the surface illtrastructure of blastocysts and endometrium. Teratology. 1979;20(1):13.
Paksy K, Gati I, Naray M, Rajczy K. Lead accumulation in human ovarian follicular fluid, and in vitro effect of lead on progesterone production by cultured human ovarian granulosa cells. J Toxicol Environ Health A. 2001;62(5):359–66.
Qu J, Niu H, Wang J, Wang Q, Li Y. Potential mechanism of lead poisoning to the growth and development of ovarian follicle. Toxicology. 2021;457:152810.
Qian Y, Tiffany-Castiglioni E. Lead-induced endoplasmic reticulum (ER) stress responses in the nervous system. Neurochem Res. 2003;28(1):153–62.
Aglan HS, Gebremedhn S, Salilew-Wondim D, Neuhof C, Tholen E, Holker M, Schellander K, Tesfaye D. Regulation of Nrf2 and NF-kappaB during lead toxicity in bovine granulosa cells. Cell Tissue Res. 2020;380(3):643–55.
Huang Z, Wells D. The human oocyte and cumulus cells relationship: new insights from the cumulus cell transcriptome. Mol Hum Reprod. 2010;16(10):715–25.
Tulić L, Vidaković S, Tulić I, Ćurčić M, Bulat Z. Toxic metal and trace element concentrations in blood and outcome of in vitro fertilization in women. Biol Trace Elem Res. 2018;188(2):284–94.
Funding
This work was supported by grants from Wenzhou City Science and Technology Bureau, CN (Y20220412) and Natural Science Foundation of Zhejiang Province, CN (Z23H040003, HC). These sources did not influence the study design, the collection, analysis or interpretation of data, or the writing of the paper.
Author information
Authors and Affiliations
Contributions
Dan Shan and Yanning Lv: Conceptualization, Investigation, Methodology, Formal analysis, Data curation, Visualization, Writing – original draft. Junzhao Zhao, Fan zhang, Haitao Xi, Haifan Qiu: Methodology, Formal analysis, Validation. Jieqiang Lv: Conceptualization, Methodology, Project administration, Writing – review. Haolin Chen: Conceptualization, Methodology, Supervision, Project administration, Funding acquisition, Writing – review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 82 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shan, D., Lv, Y., Zhao, J. et al. Association between blood lead levels and unfavorable IVF outcomes: potential involvement of endoplasmic reticulum stress response in granulosa cells. J Assist Reprod Genet 41, 947–956 (2024). https://doi.org/10.1007/s10815-024-03056-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03056-2