Abstract
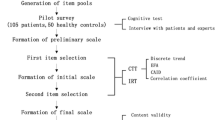
Objective: Patients with heart failure may experience thirst distress. There is, however, no measurement tool to define patients’ thirst distress in Turkey. The study aimed to determine psychometric properties of the translated Turkish version of the Thirst Distress Scale-Heart Failure (TDS-HF) in a sample of heart failure patients. Design: This methodologically planned study was conducted in two different training and research hospitals in Istanbul. Content validity, confirmatory factor analysis and concurrent validity were used in the validity analysis following the language validity analysis. Reliability coefficients were analysed by calculating Cronbach’s alpha, McDonald’s Omega and test-retest reliability coefficients. Validity and reliability analysis involved 116 patients, and test-retest analysis was carried out among 36 patients who volunteered to participate in the study. Results: The patients had a mean age of 55.2 ± 14.9. The factor structure and the examined fit indices of the one-dimensional eight-item scale indicated that the Turkish version of the scale was consistent with the original model. Item-total correlations were between 0.84 and 0.93, Cronbach’s alpha coefficient was 0.90, the test-retest reliability coefficient was 0.97 and the McDonald’s omega coefficient was 0.93, demonstrating that the scale is highly reliable. Conclusion: The Turkish version of the Thirst Distress Scale-Heart Failure was found to be valid and reliable.
Similar content being viewed by others
Introduction
Heart failure is a pathological progressive disease in which the heart can’t pump enough blood to tissues and organs to meet their metabolic needs, the structure or function of the heart is impaired, and symptoms and findings such as dyspnea, edema and fatigue are experienced (ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure, 2012). Heart failure (HF) is a growing problem today. The total number of patients with HF continues to increase (Groenewegen et al., 2020). The prevalence of HF in Turkey was reported as 2.9%, currently affecting 1.5 million people (Yılmaz et al., 2019). It is estimated that 64.3 million people worldwide live with HF, and the prevalence of HF varies between 1% and 2% in developed countries (Groenewegen et al., 2020).
Pharmacologic and device-assisted treatment methods prolong the lifespan of heart failure patients (Alpert et al., 2017). Blood pooling in heart failure patients; may cause signs and symptoms such as dyspnoea, oedema and fatigue during the disease (Allida et al., 2018; Oguz et al., 2008; Wefer et al., 2020) and their quality of life is negatively affected (Gong et al., 2022). Heart failure patients are informed to pay attention to the amount of fluid they consume and weight control to prevent fluid retention (Chrysohoou et al., 2022; Herrmann et al., 2022). Fluid restriction may help control symptoms such as dyspnea and edema experienced by patients, but it also increases the severity of thirst experienced by the patient (Ponikowski et al., 2016; Waldreus et al., 2018a).
Thirst is a physiological phenomenon associated with maintaining fluid balance (Caton et al., 2021). Behaviourally, it is defined as the desire and emotional state of the person striving to drink water but is described and experienced by affected patients differently (Allida et al., 2018; Waldreus et al., 2018a).
Several factors that contribute to thirst in HF have been suggested, such as the HF condition, the treatment adopted and self-care practices. When plasma volume or blood pressure decreases in patients with HF due to low cardiac output, volume receptors stimulate the thirst centre in the brain, causing thirst to occur (Guyton, 2007; Thornton, 2010). Angiotensin II and antidiuretic hormone levels are high in heart failure patients, and increased sympathetic activity is associated with the stimulation of the thirst center in the hypothalamus. Angiotensin II causes thirst by binding directly to receptors in the thirst center. Sympathetic stress causes vasoconstriction in the salivary glands with decreased salivary secretion. The decrease in salivation is detected by specific receptors in the mouth that are sensitive to changes in friction and osmosis in the oral mucosa. These receptors activate the thirst center (Guyton, 2007). Vasopressin antagonist tolvaptan, which is used in the treatment of volume-overloaded patients with HF, and diuretic treatment may trigger the development of thirst and dehydration in these patients (Allida et al., 2018; Chen et al., 2023; Ponikowski et al., 2016). In the case of dehydration, dry mouth develops because of decreased salivation, and the person experiences a feeling of thirst (Herrmann et al., 2022).
To understand the problems experienced by patients with HF, it is important to identify the thirst intensity and describe their distress from the thirst. Thirst intensity is defined as the severity of thirst, while thirst distress is the degree to which the patient is bothered by thirst or its associated discomfort (Waldreus et al., 2018a).
According to Waldreus et al. (2016), 63% of HF patients receiving inpatient treatment and 41% of patients in outpatient clinics experience thirst (Waldreus et al., 2016). Reilly and Dunbar (2010) reported that 46% of patients with HF described thirst as a bothersome symptom and stated they could not find anything to quench their thirst. In a study aimed at determining the factors associated with constant thirst experienced by 649 patients diagnosed with HF, the patients experienced more persistent thirst as HF symptoms increased (Waldreus et al., 2014).
Thirst is more severe in the following category of patients diagnosed with HF: males, younger patients (Allida et al., 2018; Waldreus et al., 2014) and those who have fluid and sodium restrictions (Herrmann et al., 2022); high body mass index (Waldreus et al., 2014); have high serum urea measurements (Allida et al., 2018; Waldreus et al., 2014) suffer from depressive symptoms (Waldreus et al., 2014); use diuretics (Aliti et al., 2013; Ponikowski et al., 2016; Waldreus et al., 2016), taking omeprazole, patients with renal insufficiency and have higher New York Heart Association (NHYA) classification experince more thirst (Gong et al., 2022).
Persistent thirst in individuals with HF disturbs the person and causes distress, as they tend to drink water constantly to quench their thirst (Allida et al., 2018; Waldreus et al., 2013).
Thirst not only affects the mood of patients, but also causes patients to not comply with medication and fluid restriction. It causes people with this condition to lose their abilities, their general condition to deteriorate, and their quality of life to decrease. For this reason, healthcare personnel should pay attention to thirst in patients with heart failure (Chen et al., 2023). Although there are measurement tools developed to diagnose the thirst experienced by hemodialysis patients (Kara, 2013), and surgical patients in our country (Oztaş et al., 2022), there are no studies or measurement tools to identify the thirst experienced by heart failure patients. Adapting the thirst distress scale to Turkish culture will contribute to the definition of thirst distress experienced by patients and will increase awareness of thirst distress.
This study, planned based on this deficiency, was conducted to determine the validity and reliability of the Thirst Distress scale in Turkish heart failure patients. The study was presented under the headings of translation of the scale, cultural adaptation and evaluation of psychometric properties.
Methods
Aim
The study aimed to determine psychometric properties of the translated Turkish version of the TDS-HF in a sample of heart failure patients. This study was designed as a methodological study.
Sample
The study was conducted in two different thoracic, cardiovascular and vascular surgery hospitals on the Anatolian side of Istanbul, in Turkey, between June 2019 and April 2022. The inclusion criteria for the study were patients with HF that were older than 18 years of age; were diagnosed clinically with HF (admitted for any reason); were hospitalized; were assigned functional capacity 1, 2, 3 or 4 according to the New York Heart Association; had a stable condition; and volunteered to participate in the study. A total of 144 patients were reached.
Diabetes diagnosis (4%; n = 6), diuretic dose changed in the last 24 h (5.5%; n = 8), being hungry (1%; n = 2) and receiving oxygen therapy (6%; n = 9) were considered as the exclusion criteria as these would have affected patients’ thirst experience. Patients (2%; n = 3) who did not complete the data collection forms were also excluded.
In scale validity and reliability studies, it is recommended to consider a sample size 5–10 times the number of items in the scale (Karakoc & Donmez, 2014). Since the scale included eight items in total, it was aimed to reach 80 patients with HF. Based on the study of Waldreus et al. (2018b); thirst distress score was 16.4 ± 7.8; power 0.80; alpha 0.05; for a two-sided test; Cohen’s d effect size was calculated as 0.33. It was determined that a total of 75 people should be reached. Using the non-probability sampling method, the study was completed with 116 (80.5%) patients who met the inclusion criteria and completed the data collection forms completely. The STROBE guidelines were followed in this study.
The data were collected through one-on-one interviews with the patients at the bedside using the patient identification form, thirst severity form and TDS-HF. Data on clinical characteristics (such as left ventricular ejection fraction value and vital signs) were retrieved from the patients’ medical record system. Data collection was done during the period when the visits to the clinic were over and no action would be taken regarding the patient. Patient read and answered the questions in the patient’s room, conveyed the answers verbally to the researcher. The patients could not use their arms comfortably because they had vascular access in their arms and received infusion therapy. The researcher filled out the forms. The first interview took 15 min and the second 12 min, on average.
Data collection tools
The patient identification form includes 17 questions on patients’ sociodemographic details, including age, gender, education, smoking status and information about who the patient lives with. The form also contains clinical information, including height and weight, vital signs, duration of HF, left ventricular ejection fraction, NHYA classification, comorbidities, drugs used, and fluid and salt restriction.
The thirst severity form asks patients to show the severity of their thirst on the visual analogue scale (VAS) by indicating a score between zero and one hundred (Holst et al., 2003).
Thirst Distress Scale-HF: It was developed by Waldreus et al. (2018b). The scale has a total of eight items in a single sub-dimension. In the validity and reliability study of the scale, the Cronbach’s alpha internal consistency coefficient was found to be 0.90, the intraclass correlation coefficient was 0.88, and the weighted Kappa values between 0.29 and 0.60. It is a 5-point Likert-type scale, which determines patients’ thirst experience in the last two to three days. A total score of 0–8 indicates that there is no thirst, 9–16 points shows mild thirst, 17–24 points shows moderate thirst, 25–32 points indicates high thirst and 33–40 points shows severe thirst. Permission was obtained from the author of the scale for the validity and reliability study.
Language adaptation
The original version of the scale was translated into Turkish by two translators whose native language is English, who are familiar with Turkish and English culture, who have lived abroad for a long time and who have different backgrounds. One of the translator was aware of the concept and the other translator had no medical clinical background and was not knowledgeable about the concept being measured (Beaton et al., 2000). After the translation, corrections were made by the first and second researchers and the final Turkish version of the scale was created.
The Turkish version of the scale was translated into English by two different translators who were different from the first translators but had the same characteristics.
The final English version of the scale was examined in terms of sentence structure, meaning and expression by the researcher and all the translators mentioned above, who did the translation and back-translation, and the final version was created.
It was conveyed to the owner of the scale, but feedback was received from the person who developed the scale, stating that the 2nd scale item did not have the same meaning.
The back-translation of the scale item for which correction was requested was re-translated by two different translators who have the same qualifications as the translators above.
The expression “I am very uncomfortable when I am thirsty” was translated as “I feel very unhappy when I am thirsty” in English and was translated into Turkish as “Susadığımda çok keyifsiz olurum”, and feedback was received once again regarding the suitability of this statement. The scale items that received positive feedback (Sousa &Rojjanasrirat, 2011).
Content validity
To determine content validity, The Davis technique was used (Davis, 1992; Capık and Gozum, 2018). A scale presentation form was created and presented to a panel of experts: eight academician nurses (three nurses are nurses who have worked in the cardiology clinic for more than ten years, two nurses are heart failure case manager nurses and have master’s degrees in research methods, three nurses are academic nurses working in the field of cardiology, with a PhD degree). Experts were asked to rate each item between one and four points to establish the consistency between the original English items and the Turkish translation of the scale and to determine the clarity of the statements (Capık and Gozum, 2018; Karacam, 2019). The points were allocated as follows: one point meant not appropriate, two points indicated somewhat appropriate (with some revision of the statement necessary), three points showed the statement was appropriate with minor changes necessary and four points showed that the statement was completely appropriate (Davis, 1992; Erdogan et al., 2018). The study was based on the opinions of eight experts. The content validity index (CVI) was calculated by dividing the number of experts who gave three and four points for the items on the scale by the total number of experts. The CVI score was found to be 0.92. After language equivalence was established, the scale was tested for intelligibility by applying it to eight inpatients with a diagnosis of HF outside of the sample, were asked to evaluate the intelligibility of the items on a 5-point Likert scale (from 1 = I don’t understand at all to 5 = I understand completely).
Construct validity
Confirmatory factor analysis (CFA) was used to evaluate the construct validity of the scale. CFA tests whether a predefined structure is validated as a model. In this process, the effectiveness of the model in explaining the obtained data is determined by the goodness-of-fit indices. Goodness-of-fit indices affect the decision to accept or reject the model (Cokluk et al., 2014). In this study, the following tests of fit indices were examined: the comparative fit index (CFI), the Tucker-Lewis Index (TLI), the root mean square error of approximation (RMSEA) and the weighted least squares mean and variance (WRMR). In CFA the covariance matrix is used to reveal the hidden conceptual structures and to see the interactions between the items. The created matrix is examined through the estimation method (Capık and Gozum, 2018). The weighted least squares mean and variance (WLSMV) estimation method was used here, since the item scores of the CFA are of the ordinal variable type.
Concurrent validity
To determine the concurrent validity, the relationship between the severity of thirst and the total score from the Thirst Distress Scale-HF was examined using the Pearson correlation test (Frey, 2018).
Reliability of the scale
Cronbach alpha reliability coefficient was used to test the reliability of the scale and item-total correlation analysis was used to determine the internal validity of the items (Oksuz & Malhan, 2005). McDonald’s Omega coefficient was calculated to determine the structural reliability of the scale (Kartal & Dirlik, 2016).
Test -retest reliability
Test-retest mean scores were compared to determine whether the scale was a consistent tool against time (Polit, 2015). The same scale items were re-administered to 36 patients selected from the sample group 15 days later. The Pearson correlation test was used to determine the degree and significance of the relationship between the two measures.
Ethical considerations
As per the Declaration of Helsinki, ethical approval from the ethics committee of the university (protocol code: 09.2019.400) and institutional permission from the hospitals where the study would be conducted were obtained. In addition, written informed consent was obtained from each participant before the study.
Evaluation of the data
Patients’ descriptive and clinical information was presented with percentiles and averages for the study. In the data set obtained from the Turkish version of the scale, the relations between the variables were analysed by CFA for the explanatory power of the theoretical model. CFA was performed using the WLSMV estimation method in the Mplus 8.1 software package, since the item scores were of the ordinal variable type.
Before confirmatory factor analysis was completed, a data check was carried out using the SPSS 26 program. The linear relationship between the items was examined by curve estimation. It was found that the linear model explained the covariance among the items more than the nonlinear ones. The correlations between item scores between 0.41 and 0.72 showed that there was no multicollinearity. In addition, no outliers were identified since there were no observations exceeding the value of Z.0001> 3.29 in any of the standard score distributions of the items.
Results
The results of the study are presented under two headings: findings related to the descriptive and clinical characteristics of the patients and findings related to the reliability and validity of the scale.
Findings related to descriptive and clinical characteristics of the patients
The patients had a mean age of 55.2 ± 14.9. Patients’ total score from the TDS-HF scale was 27.1 ± 8.5. The mean duration of HF was 43 ± 30 months, and the left ventricular ejection fraction was 26 ± 10; 4% had Stage 3 functional capacity according to NYHA. 78.4% were male. Half of them (49.1%) were primary school graduates and the majority (81.9%) lived with their spouses. Less than half (34.5%) were smokers. As clinical characteristics Almost all the patients had water (90.5%) and salt (93.1%) restrictions. Other descriptive and clinical characteristics of the patients are listed in Table 1.
Reliability results of the Thirst distress Scale-HF (TDS-HF)
The Cronbach alpha reliability coefficient of the measurements obtained from the Turkish version of the scale was 0.90. The McDonald Omega coefficient was 0.93. The result of the study shows high structural reliability for the scale. Item-total correlations ranged from 0.84 to 0.93 (Table 2). Test-retest reliability was r = .97.
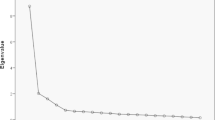
Construct Validity results of the Thirst Distress Scale-HF (TDS-HF)
A Kaiser-Mayer-Olkin (KMO) value of 0.87 and a Bartlett test result of \({\chi }_{28}^{2}\)= 504.86, p = .00 proved that the relations between item score distributions were sufficient for factor analysis.
The factor loadings of the data obtained from the Turkish version of the scale are given in Fig. 1. Factor loading values were between 0.65 and 0.84. Our model fit summary is shown in Table 3. A good model–data fit is indicated by RMSEA ≤ 0.06, CFI > 0.95, and TLI > 0.95 (Hu & Bentler, 1999) and WRMR equal to or less than 1 (Yu & Muthen, 2002; DiStefano et al., 2019). In this study, the RMSEA value is 0.17, CFI and TLI values are 0.95 and 0.93, respectively, The WRMR value is 0.91, were found acceptable.
Concurrent validity results of the Thirst Distress Scale-Heart Failure (TDS-HF)
Thirst severity (Vas: 0-100 mm) total score of the patients was 53.10 ± 26.58 mm. Thirst Distress Scale-HF total score was significantly and positively correlated with the severity of thirst (r = .48, p < .001) (Table 4), with the scores obtained from TDS-HF increasing as the severity of thirst increased. The relationship between the Thirst Distress Scale-HF and other variables is given in Table 4.
Discussion
The results of the study demonstrated that the Thirst Distress Scale-HF met the criteria for validity and reliability, and the scale was understandable and easy to use by the patients. After the analysis, the original form of the scale was preserved, and no changes were made to the scale items. There is no study conducted in our country to diagnose the thirst problem experienced by heart failure patients and no scale developed on this subject. The thirst distress scale is the only scale that can be used in heart failure patients in Turkey. For this reason, it is thought that the scale will make a significant contribution to diagnosing the thirst problem experienced by heart failure patients.
Expert opinion was sought to determine whether the scale items measured the intended parameter correctly (Sousa & Rojjanasrirat, 2011). In the literature, it is reported that the content validity index should be at least 0.80 for content validity (Erdogan et al., 2018). In this study, the content validity index was high (0.92) and the content validity of the scale was good. This finding was not discussed because the content validity index was not given in studies where the scale was adapted to different cultures (Eng et al., 2021; Waldreus et al., 2018b; Wefer et al., 2020).
It was concluded that the language structure and items of the scale were understandable.
Scale items have linguistic and cultural differences. Third item on the thirst distress scale: When I’m thirsty, my mouth feels like sandpaper. The sandpaper in the sentence is “cotton” in English; in Swedish and Dutch, the word “sandpaper” is used; and in the Japanese version, it is used as the word “rough” (Waldreus et al., 2018b). After patient and expert opinions, “zımpara kağıdı”, the Turkish equivalent of the word “sandpaper” used in Swedish and Dutch culture, was used. The expression “I am very uncomfortable when I am thirsty” was translated as “I feel very unhappy when I am thirsty” in English and was translated into Turkish as “Susadığımda çok keyifsiz olurum”. After the feedback received from patients and experts, it was decided to use this expression.
In cross-cultural scale adaptation studies, it is recommended to start with confirmatory factor analysis for the factor pattern of the scale in the target culture (Çokluk et al., 2014). It is also recommended to perform a linearity analysis before performing the confirmatory factor analysis (Black et al., 2021). The linearity assumption can be examined using correlation matrices or graphical representation methods. If this assumption is infringed, model fit estimates and standard errors become biased (Bayram, 2010). In this study, the linear relationship between the items was examined by curve estimation. It was found that the linear model explained the covariance among the items better than the nonlinear ones.
A Kaiser-Mayer-Olkin coefficient and Bartlett’s sphericity test were applied to test the suitability of the scale in terms of construct validity. A Kaiser-Mayer-Olkin value between 0.50 and 0.60 indicates bad, between 0.60 and 0.70 poor, between 0.70 and 0.80 moderate, between 0.80 and 0.90 good and over 0.90 indicate excellent sample adequacy (Cokluk et al., 2014). In the studies examining scales adapted to different cultures, KMO value was found as 0.90 by Waldreus et al. (2018b) and 0.92 by Eng et al. (2021). In our study, the KMO value of 0.87 showed that the relationships between the item score distributions and the sample size were sufficient for factor analysis. The Bartlett test of sphericity is significant indicates that the correlation matrix of the items in the scale is suitable for factor analysis (Cokluk et al., 2014). In this study, Bartlett’s test was determined to be significant. When these findings were evaluated, it was concluded that the research sample size was sufficient for factor analysis and that factor analysis regarding the scale could be performed.
The factor loading value is a coefficient that explains the relationship of the items with the factor. If there is a set of items yielding a high correlation with a factor, this means that these items measure the structure in question (Cokluk et al., 2014). Tabachnick and Fidell (2013) recommend evaluating the load value of each variable as 0.32 and above. In Waldreus et al. (2018b) study, the factor loadings of the scale were between 0.40 and 0.79; In Wefer et al. (2020) study, it was stated that factor loadings varied between 0.57 and 0.86. In this study, factor loading values (standard regression weights) were greater than 0.50 (Fig. 1). The relevant scale items adequately represent the factor dimension they belong to.
In the study, the CFI value was 0.95, the TLI value was 0.93, the WRMR value was 0.91 and the RMSEA value was 0.17 (90% CI: 0.14 to 0.21) (Table 3). Since the Comparative Fit Index value also considers the sample size, it works well even when the sample is small. CFI gives a value between 0 and 1. A value close to 1 corresponds to a perfect fit, and a value closer to 0 indicates lack of fit for the selected scale (Hu & Bentler, 1999). It is recommended that the Tucker-Lewis Index value be close to or greater than 0.95 (Hu & Bentler, 1999; Brown, 2006). WRMR is a model data fit index obtained when estimation methods (such as WLMSV and WLSM) for ordinal data and categorical data are used. According to Yu and Muthen (2002), a WRMR value of ≤ 1 indicates good fit. In another study examining the validity and reliability of the scale, CFI, TLI, and RMSEA were 0.94, 0.92, and 0.11 (90%CI:0.05-0.16), respectively (Wefer et al., 2020). Root Mean Square Error of Approximation (RMSEA) shows that there is no difference between population and sample covariances. RMSEA value ≤ 0.06 indicates good fit (Hu & Bentler, 1999); ≤ 0.10 indicates poor fit (Tabachnick & Fidell, 2013). Chi-square is affected by sample size and RMSEA was calculated based on chi-square. Model fit was evaluated from the values above, apart from the general fit coefficients.
In addition, the standard regression weights (factor loads) were greater than 0.50 (Fig. 1), and the average variance extracted (AVE) by the factor in the items was = 0.62. The McDonald Omega coefficient was 0.93, which is greater than the AVE. As a result, the fit coefficients other than chi-square and RMSEA (such as CFI and TLI, which compares the fit with the baseline model, and WRMR, which indicates the inconsistency of the model, are close to 1) and the other parameter estimates above indicate the adequacy of the model. The fit indices examined in this study showed that the Turkish version of the scale was compatible with the original model.
The average variance extracted (AVE) shows the strength of the factor structure of the scale (Fornell & Larcker, 1981). The AVE of the unidimensional scale in this study was 0.62. As stated by Cokluk et al. (2014), a total variance of 30% or more explained in single-factor scales is considered an indication of the one-dimensional measurability of the relevant concept and structure.
A positive correlation was found between the severity of thirst and the TDS-HF total score (r = .48, p < .001), establishing the concurrent validity (Table 4). The relationship between thirst severity and TDS-HF was reported as r = .59, p < .001 (Eng et al., 2021), r = .56, p < .001 (Waldreus et al., 2018b) r = .72, p ≤ .001 (Wefer et al., 2020) from similar studies. Accordingly, as the severity of thirst increases, the scores obtained from TDS-HF increase.
In this study, the Cronbach alpha coefficient of the scale was found to be 0.90. Finding a high reliability coefficient indicates that the items used for measurement measure a homogeneous structure (Oksuz & Malhan, 2005). In their study adapting the scale to different cultures, Waldreus et al. (2018b) found the internal consistency coefficient as 0.90 compared with 0.89 reported Wefer et al. (2020). The reliability coefficient of this study is similar to the above studies.
In this study, the scale was re-administered to 36 patients after an interval of 15 days. The test-retest reliability coefficient was found to be 0.97 (Table 2). The optimal period for the test-retest interval is 15 days, and the test-retest reliability coefficient should be above 0.90. (Polit, 2015). Bolarinwa (2015) stated that a correlation coefficient above 0.70 is an acceptable good value. Waldreus et al. (2018b) found the test-retest reliability coefficient to be 0.88 in their study. The high correlation value indicated that the scale was a consistent measurement tool against time.
In this study, item-total correlations of the scale were found to be between 0.84 and 0.93 (Table 2). In item-total-score correlations, values 0.40 and above are considered very distinctive, between 0.30 and 0.40 good and between 0.20 and 0.30 requiring revision (Tavsancıl, 2014). Item-total correlations between 0.58 and 0.78 was found by Wefer et al. (2020) and between 0.63 and 0.75 by Waldreus et al. (2018b). The item-total correlation values in our study were higher than the other studies. These results showed us that the scale items were related to the topic and measured the intended topic.
In this study, McDonald Omega coefficient was found to be 0.93. Suggested by McDonald, omega coefficient is one of the reliability coefficients developed as an alternative to Cronbach’s alpha. Structural reliability Omega coefficient usually gives a value equal to or higher than Cronbach’s alpha in reliability calculations (Kartal & Dirlik, 2016; Yurdugul, 2006). McDonald’s Omega value > 0.8 was interpreted as indicative of good reliability (Feibt et al., 2019). The results could not be compared with the findings reported by Waldreus et al. (2018b) because McDonald Omega coefficient had not been conducted in the original study. The result of the study shows high structural reliability for the scale.
Conclusion
It was determined that the Thirst Distress Scale-HF was valid and reliable in patients with heart failure in our country. It is recommended to use the TDS-HF scale in determining thirst distress in HF patients. The thirst distress scale is a short and easy to understand scale that can be used in heart failure patients. Identifying the thirst distress experienced by patients will guide the planning of interventions to alleviate thirst distress. It should not be overlooked by healthcare professionals that patients who have water and salt restrictions and use more than one diuretic may experience thirst. It should be anticipated that foods with high salt content (such as olives, sausage, pastrami, roasted meat, and pickles), which are consumed most frequently by the public in Turkish culture, will increase the feeling of thirst if consumed by heart failure patients.
It is important for healthcare professionals (nurses, physicians) to be aware of the thirst experienced by heart failure patients and that this situation causes distress in patients, and to evaluate the thirst experienced by patients at regular intervals. Although the symptom of thirst is common in heart failure patients, it can often be ignored by healthcare professionals. This situation is thought to be due to healthcare professionals’ lack of awareness about thirst, lack of questioning of thirst, and lack of evidence-based practices related to thirst management. For this reason, it is important to inform healthcare professionals about the management of thirst symptoms, to assess thirst, to take evidence-based interventions to prevent or to minimize thirst distress if it exists.
Limitations
The data collection process took a long time due to the restrictions during the Covid-19 pandemic process. This study was conducted in heart failure patients receiving inpatient treatment. Due to the long duration of the data collection process, air temperatures that are thought to affect thirst varied. According to the New York Heart Association (NHYA), the number of patients with functional capacity IV was low.
Implications for future research.
The tool can be used to evaluate the effectiveness of interventions to prevent thirst distress. The psychometric properties of the measure will provide cross-cultural comparison after translations into different cultures. A study can be conducted to determine the thirst problem experienced by patients living in different climatic conditions and from different cultures.
It is recommended to examine the impact of interventions to reduce thirst distress on the patient’s compliance with fluid restriction and quality of life. It may be recommended to conduct studies on the food and beverages consumed by heart failure patients in different cultures to alleviate their thirst.
Data availability
The data underlying this article cannot be shared publicly due to participants not consenting to sharing of data. The data will be shared on reasonable request to the corresponding author.
References
Aliti, G. B., Rabelo, E. R., Clausell, N., Rohde, L. E., Biolo, A., & Silva, L. B. (2013). Aggressive fluid and sodium restriction in acute decompensated heart failure: A randomized clinical trial. JAMA Intern Med, 173(12), 1058–1064. https://doi.org/10.1001/jamainternmed.2013.552
Allida, S., Hayward, C., & Newton, P. (2018). Thirst in heart failure: What do we know so far? Current Opinion in Supportive and Palliative Care, 12, 4–9. https://doi.org/10.1097/SPC.0000000000000314
Alpert, C. M., Smith, M. A., Hummel, S. L., & Hummel, E. K. (2017). Symptom burden in heart failure: Assessment, impact on outcomes, and management. Heart Failure Reviews, 22(1), 25–39.
Bayram, N. (2010). Yapısal Eşitlik Modellemesine Giriş (Amos Uygulamaları). Ezgi Kitabevi.
Beaton, D. E., Bombardier, C., Guillemin, F., & Ferraz, M. B. (2000). Guidelines for the process of cross-cultural adaptation of self-report measures. Spine, 15(24), 3186–3191.
Black, J. F., Babin, B. J., & Anderson, R. E. (2021). Multivariate data analysis (8th ed.). Cengage Learning.
Bolarinwa, O. A. (2015). Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Nigerian Postgraduate Medical Journal, 22(4), 195–201. https://doi.org/10.4103/1117-1936.173959
Brown, T. A. (2006). Confirmatory factor analysis for applied research. Guilford.
Capık, C., & Gozum, S. (2018). Intercultural scale adaptation stages, language and culture adaptation: Updated guideline. Florence Nightingale Journal of Nursing, 26(3), 199–210. https://doi.org/10.26650/FNJN397481
Caton, J. B., Jimenez, S., & Wang, S. X. Y. (2021). Things we do for no reason™: Fluid restriction for the management of acute decompensated heart failure in patients with reduced ejection fraction. Journal of Hospital Medicine, 16(12), 754–756. https://doi.org/10.12788/jhm.3639
Chen, Y., Ding, J., Xi, Y., Huo, M., Mou, Y., Song, Y., Zhou, H., & Cui, X. (2023). Thirst in heart failure: A scoping review. Nursing Open, 10, 4948–4958.
Chrysohoou, C., Mantzouranis, E., Dimitroglou, Y., Mavroudis, A., & Tsioufis, K. (2022). Fluid and salt balance and the role of nutrition in heart failure. Nutrients, 14(7), 1386.
Cokluk, Ö., Şekercioglu, G., & Buyukozturk, Ş. (2014). Sosyal Bilimler için Çok Degiskenli Istatistik SPSS ve LISREL Uygulamaları. Pegem Akademi, 3. Baskı, Ankara, 2014.
Davis, L. L. (1992). Instrument review: Getting the most from a panel of experts. Applied Nursing Research, 5, 194–197.
Eng, S. H., Waldreus, N., Gonzalez, B., Ehrlin, J., Diaz, V., Rivas, C., & Jaarsma, T. (2021). Thirst distress in outpatients with heart failure in a Mediterranean zone of Spain. ESC Heart Failure, 2021(8), 2492–2501. https://doi.org/10.1002/ehf2.13395
Erdogan, S., Nahçivan, N., & Esin, M. N. (2018). Hemşirelikte Araştırma: Sürec, Uygulama ve Kritik. Nobel Tıp Kitabevleri. 3. Basım, İstanbul.
ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure, (2012). Turkish Society of Cardiology, 40(3):77–137.
Feibt, M., Hennings, A., Moosbrugger, H., Kelawa, A., Stolpner, I., Kieser, M., & Rauch, G. (2019). Refining scores based on patient reported outcomes – statistical and medical perspectives. BMC Medical Research Methodology, 19, 167. https://doi.org/10.1186/s12874-019-0806-9
Fornell, C., & Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18, 39–50.
Frey, B. (2018). The SAGE Encyclopedia of Educational Research, Measurement, and Evaluation, Chapter Title: Concurrent Validity. SAGE Publications, Inc., 2018.
Gong, J., Waldreus, N., Hu, S., Luo, Z., Xu, M., & Zhu, L. (2022). Thirst and factors associated with thirst in hospitalized patients with heart failure in China. Heart & Lung, 53, 83–88.
Groenewegen, A., Rutten, F. H., Mosterd, A., & Hoes, A. W. (2020). Epidemiology of heart failure. European Journal of Heart Failure, 22, 1342–1356. https://doi.org/10.1002/ejhf.1858
Guyton, A. H. J. (2007). Tıbbi Fizyoloji. 11 th edit. Cavusoglu, Hayrunnisa; Çag B, editor.
Herrmann, J. J., Beckers-Wesche, F., Baltussen, L. E., Verdijk, M. H., Bellersen, L., Brunner-la Rocca, H. P., & Van Kimmenade, R. R. (2022). Fluid restriction in heart failure vs liberal fluid uptake: Rationale and design of the randomized FRESH-UP study. Journal of Cardiac Failure, 28(10), 1522–1530. https://doi.org/10.1016/j.cardfail.2022.05.015
Holst, M., Strömbergc, A., Lindholma, M., Uden, G., & Willenheimer, R. (2003). Fluid restriction in heart failure patients: Is it useful? The design of a prospective, randomised study. European Journal of Cardiovascular Nursing, 2, 237–242. https://doi.org/10.1016/S1474-5151(03)00066-5
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
Kara, B. (2013). Validity and reliability of the Turkish version of the Thirst distress scale in patients on hemodialysis. Asian Nursing Research, 7, 212–218.
Karacam, Z. (2019). Adaptation of scales to Turkish. Journal of Midwifery and Health Sciences, 2(1), 28–37.
Karakoc, F. Y., & Dönmez, L. (2014). Basic principles of scale development. Tıp Egitimi Dunyası, 40, 39–49.
Kartal, K. S., & Mor Dirlik, E. (2016). Geçerlik kavramının tarihsel gelişimi ve güvenirlikte en çok tercih edilen yöntem: Cronbach Alfa Katsayısı. Abant İzzet Baysal Üniversitesi Eğitim Fakültesi Dergisi, 16(4), 1865–1879.
Oguz, S., & Enc, N. (2008). Symptoms and strategies in heart failure in Turkey. International Nursing Review, 55(4), 462–467. https://doi.org/10.1111/j.1466-7657.2008.00661.x
Oksuz, E., & Malhan, S. (2005). Sağlığa Bağlı Yaşam Kalitesi Kalitemetri, 68–104.
Oztaş, B., Öztas, M., Şahin, S. Y., İyigün, E., & Alkuş, Ü. (2022). Assessing thirst symptom of patients undergoing abdominal surgery: A scale development study. Turkish Journal of Colorectal Disease, 32, 48–53.
Polit, D. (2015). Assessing measurement in health: Beyond reliability and validity. International Journal of Nursing Studies, 52, 1746–1753. https://doi.org/10.1016/j.ijnurstu.2015.07.002
Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H., Cleland, J. G. F., Coats, A. J. S., & Meer, P. (2016). 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal, 14(37(27), 2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Reilly, C. M., Meadows, K., Dunbar, S., Culler, S., & Smith, A. (2010). Thirst and QoL in persons with heart failure. Heart & Lung, 39(4), 353. https://doi.org/10.1016/j.hrtlng.2010.05.011
Sousa, V. D., & Rojjanasrirat, W. (2011). Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. Journal of Evaluation in Clinical Practice, 17(2), 268–274. https://doi.org/10.1111/j.1365-2753.2010.01434.xl
Tabachnick, B. G., & Fidell, L. S. (2013). Using Multivariate statistics (6thed). Pearson.
Tavsancıl, E. (2014). Tutumların Ölçülmesi ve Spss İle Veri Analizi (5. Baskı). Nobel Yayınevi.
Thornton, S. N. (2010). Thirst and hydration: Physiology and consequences of dysfunction. Physiology & Behavior, 100(1), 15–21. https://doi.org/10.1016/j.physbeh.2010.02.026
Waldreus, N., Hah, R. G., & Jaarsma, T. (2013). Thirst in heart failure: A systematic literature review. European Journal of Heart Failure, 15(2), 141–149. https://doi.org/10.1093/eurjhf/hfs174
Waldreus, N., van der Wal, M. H., Hahn, R. G., Veldhuisen, D. J., & Jaarsma, T. (2014). Thirst trajectory and factors associated with persistent thirst in patients with heart failure. Journal of Cardiac Failure, 20(9), 689–695. https://doi.org/10.1016/j.cardfail.2014.06.352
Waldreus, N., Hü, R. G., Lynga, P., Wal, M. H. L., Hagglund, E., & Jaarsma, T. (2016). Changes in thirst intensity during optimization of heart failuıe medical therapy by nurses at the outpatient c|inic. Journal of Cardiovascular Nursing, 2016; 3l(5),E17-E24. https://doi.org/10.1097/JCN.0000000000000319
Waldreus, N., Chung, M. L., Wal, M., & Jaarsma, T. (2018a). Trajectory of thirst intensity and distress from admission to 4-weeks follow up at home in patients with heart failure. Patient Preference and Adherence, 12, 2223–2231. https://doi.org/10.2147/PPA.S167724
Waldreus, N., Jaarsma, T., Wal, M. H. L., & Kato, N. P. (2018b). Development and psychometric evaluation of the Thirst distress scale for patients with heart failure. European Journal of Cardiovascular Nursing, 17(3), 226–234. https://doi.org/10.1177/1474515117728624
Wefer, F., Inkrot, S., Waldreus, N., Jaarsma, T., Cube, M., & Kugler, C. (2020). Translation and psychometric evaluation of the German version of the Thirst distress scale for patients with heart failure. The Journal of Cardiovascular Nursing, 37(4), 378–385. https://doi.org/10.1097/JCN.0000000000000780
Yılmaz, B. M., Celik, A., Cavuşoglu, Y., Bekar, L., Onrat, E., Eren, M., & Tokgözoğlu, L. (2019). Snapshot evaluation of heart failure in Turkey: Baseline characteristics of SELFIE-TR. Turk Kardiyol Dern Ars, 47(3), 198–206. https://doi.org/10.5543/tkda.2019.66877
Yu, C. Y., & Muthen, B. (2002). Evaluation of model fit indices for latent variable models with categorical and continuous outcomes. In annual meeting of the American Educational Research Association, New Orleans, LA.
Yurdugul, H. (2006). The comparison of reliability coefficients in parallel, Tau-equivalent, and congeneric measurements. Ankara University. Journal of Faculty of Educational Sciences, 39(1), 15–37.
Acknowledgements
The authors gratefully acknowledge the patients who participated in this study are appreciated.
Funding
This research did not receive specific grant from funding agencies.
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical consideration
As per the Declaration of Helsinki, ethical approval from the ethics committee of the university (date: 09.2019; decision number: 400) were obtained.
Conflicts of interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yakar, H.K., Oguz, S. & Waldreus, N. Reliability and validity of the Turkish version of the thirst distress scale-heart failure. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-05792-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s12144-024-05792-1