Abstract
Background and purpose
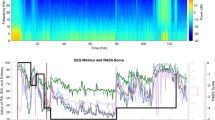
Bispectral Index (BIS) and University of Michigan Sedation Scale (UMSS) were two commonly used methods of monitoring the sedation depth, but their correlation was not clear. The purpose of this study is to ascertain if BIS correlates with UMSS in determining the sedation level during pediatric drug-induced sleep endoscopy (DISE).
Methods
One-hundred children, aged 36–143 months, with ASA I~II grade, were enrolled. They were subject to general anesthesia for an elective adenotonsillectomy. Two drug regimens were used. After UMSS ≥ 3, the sites of airway obstructions were located by checking the supraglottic airway structures with a fibrous laryngoscope. UMSS scores, BIS values, electromyography (EMG), and signal quality indices (SQIs) were recorded at the pre-medication and pre-DISE baseline (T0), 5 min subsequent to medication administration but prior to DISE initiation (T1), 1 min after DISE was initiated (T2), 1 min after DISE was completed (T3), 1 min subsequent to tracheal intubation (T4), 1 min following extubation (T5), and 30 min past extubation (T6).
Results
There were strong correlations between BIS monitor readings and UMSS scores for total and two regimens. Kappa values revealed moderate agreement between BIS and UMSS for total and two regimens. The agreement rates were 67.47% for the total, 61.43% for Regimen 1, and 73.42% for Regimen 2, respectively.
Conclusion
BIS correlates with UMSS in determining the sedation level during pediatric DISE for two regimens. BIS might serve as an appropriate indicator of sedation intensity when UMSS could not be used.


Similar content being viewed by others
Data availability
The novel findings presented within this research are detailed within the main text, and any additional inquiries should be addressed to the corresponding authors.
References
ZerpaZerpa V, Carrasco Llatas M, Agostini Porras G, Dalmau GJ (2015) Drug-induced sedation endoscopy versus clinical exploration for the diagnosis of severe upper airway obstruction in OSAHS patients. Sleep Breath 19:1367–1372. https://doi.org/10.1007/s11325-015-1266-z
Capasso R, Rosa T, Tsou DY, Nekhendzy V, Drover D, Collins J et al (2016) Variable findings for drug-induced sleep endoscopy in obstructive sleep apnea with propofol versus dexmedetomidine. Otolaryngol Head Neck Surg 154:765–770. https://doi.org/10.1177/0194599815625972
Chen RF, Nakayama M, Sung WC, Hung JF, Chu YM (2022) Comparison of surgical outcomes of sleep surgeries preoperatively evaluated with drug-induced sleep endoscopy and Müller’s maneuver. Auris Nasus Larynx 49:235–239. https://doi.org/10.1016/j.anl.2021.08.001
Smith DF, He S, Peddireddy NS, VairavanManickam PC, Heubi H, Shott SR et al (2020) Effectiveness of pediatric drug-induced sleep endoscopy for REM-predominant obstructive sleep apnea. Sleep Breath 24:1705–1713. https://doi.org/10.1007/s11325-020-02056-7
Cho JS, Soh S, Kim EJ, Cho HJ, Shin S, Kim HJ et al (2015) Comparison of three sedation regimens for drug-induced sleep endoscopy. Sleep Breath 19:711–717. https://doi.org/10.1007/s11325-015-1127-9
Liu KA, Liu CC, Alex G, Szmuk P, Mitchell RB (2020) Anesthetic management of children undergoing drug-induced sleep endoscopy: a retrospective review. Int J Pediatr Otorhinolaryngol 139:110440. https://doi.org/10.1016/j.ijporl.2020.110440
Coté CJ, Wilson S; AMERICAN ACADEMY OF PEDIATRICS; AMERICAN ACADEMY OF PEDIATRIC DENTISTRY. Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures. Pediatrics. (2019);143:e20191000. https://doi.org/10.1542/peds.2019-1000
Benzoni T, Cascella M. Procedural sedation. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; (2022)
Varndell W, Elliott D, Fry M (2015) The validity, reliability, responsiveness and applicability of observation sedation-scoring instruments for use with adult patients in the emergency department: a systematic literature review. Australas Emerg Nurs J 18:1–23. https://doi.org/10.1016/j.aenj.2014.07.001
Malviya S, Voepel-Lewis T, Tait AR, Merkel S, Tremper K, Naughton N (2002) Depth of sedation in children undergoing computed tomography: validity and reliability of the University of Michigan Sedation Scale (UMSS). Br J Anaesth 88:241–245. https://doi.org/10.1093/bja/88.2.241
Shields CH, Styadi-Park G, McCown MY, Creamer KM (2005) Clinical utility of the Bispectral Index score when compared to the University of Michigan Sedation Scale in assessing the depth of outpatient pediatric sedation. Clin Pediatr (Phila) 44:229–236. https://doi.org/10.1177/000992280504400306
Liu PP, Wu C, Wu JZ, Zhang MZ, Zheng JJ, Shen Y, He P, Sun Y (2018) The prediction probabilities for emergence from sevoflurane anesthesia in children: a comparison of the perfusion index and the Bispectral Index. Paediatr Anaesth 28:281–286. https://doi.org/10.1111/pan.13324
Delfino AE, Cortinez LI, Fierro CV, Muñoz HR (2009) Propofol consumption and recovery times after Bispectral Index or cerebral state index guidance of anaesthesia. Br J Anaesth 103:255–259. https://doi.org/10.1093/bja/aep138
Myles PS, Leslie K, McNeil J, Forbes A, Chan MT (2004) Bispectral Index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 363:1757–1763. https://doi.org/10.1016/S0140-6736(04)16300-9
Goyal A, Mittal N, Mittal P, Gauba K. Bispectral Index Monitoring: validity and utility in pediatric dentistry. J Clin Pediatr Dent. (2014) 38:366-369. https://doi.org/10.17796/jcpd.38.4.17j63w8013614933
Lo YL, Ni YL, Wang TY, Lin HY, Li DP, White JR et al (2015) Bispectral Index in evaluating effects of sedation depth on drug-induced sleep endoscopy. J Clin Sleep Med. 11:1011–1020. https://doi.org/10.5664/jcsm.5016
Stierer TL, Ishman SL (2015) Bispectral Index in evaluating effects of sedation depth on drug-induced sleep endoscopy: DISE or no dice. J Clin Sleep Med 11:965–966. https://doi.org/10.5664/jcsm.5002
Heavner MS, Gorman EF, Linn DD, Yeung SYA, Miano TA (2022) Systematic review and meta-analysis of the correlation between bispectral Index (BIS) and clinical sedation scales: toward defining the role of BIS in critically ill patients. Pharmacotherapy 42:667–676. https://doi.org/10.1002/phar.2712
Sadhasivam S, Ganesh A, Robison A, Kaye R, Watcha MF (2006) Validation of the Bispectral Index monitor for measuring the depth of sedation in children. Anesth Analg 102:383–388. https://doi.org/10.1213/01.ANE.0000184115.57837.30
Haberland CM, Baker S, Liu H (2011) Bispectral Index monitoring of sedation depth in pediatric dental patients. Anesth Prog 58:66–72. https://doi.org/10.2344/0003-3006-58.2.66
Malviya S, Voepel-Lewis T, Ludomirsky A, Marshall J, Tait AR (2004) Can we improve the assessment of discharge readiness?: a comparative study of observational and objective measures of depth of sedation in children. Anesthesiology 100:218–24. https://doi.org/10.1097/00000542-200402000-00007
Malviya S, Voepel-Lewis T, Tait AR (2006) A comparison of observational and objective measures to differentiate depth of sedation in children from birth to 18 years of age. Anesth Analg 102:389–394. https://doi.org/10.1213/01.ANE.0000184045.01780.73
Jung SM, Lee E, Park SJ (2019) Validity of Bispectral Index monitoring during deep sedation in children with spastic cerebral palsy undergoing injection of botulinum toxin. Korean J Anesthesiol 72:592–598. https://doi.org/10.4097/kja.19129
Evans RG, Crawford MW, Noseworthy, Yoo SJ, Effect of increasing depth of propofol anesthesia on upper airway configuration in children. Anesthesiology. (2003) 99:596-602. https://doi.org/10.1097/00000542-200309000-00014
Malviya S, Voepel-Lewis T, Tait AR, Watcha MF, Sadhasivam S, Friesen RH (2007) Effect of age and sedative agent on the accuracy of Bispectral Index in detecting depth of sedation in children. Pediatrics 120:e461-70. https://doi.org/10.1542/peds.2006-2577
McDermott NB, VanSickle T, Motas D, Friesen RH (2003) Validation of the Bispectral Index monitor during conscious and deep sedation in children. Anesth Analg. 97:39–43. https://doi.org/10.1213/01.ane.0000067402.02136.a2
Ibrahim AE, Taraday JK, Kharasch ED (2001) Bispectral Index monitoring during sedation with sevoflurane, midazolam, and propofol. Anesthesiology 95:1151–9. https://doi.org/10.1097/00000542-200111000-00019
Woolsey AJ, Nanji JA, Moreau C, Sivapalan S, Bourque SL, Ceccherini-Nelli A, Gragasin FS (2022) Low-dose ketamine does not improve the speed of recovery from depression in electroconvulsive therapy: a randomized controlled trial. Braz J Psychiatry 44:6–14. https://doi.org/10.1590/1516-4446-2020-1705
Xin N, Yan W, Jin S (2022) Efficacy of analgesic propofol/esketamine and propofol/fentanyl for painless induced abortion: a randomized clinical trial. Biomed Res Int 2022:5095282. https://doi.org/10.1155/2022/5095282
Sengupta S, Ghosh S, Rudra A, Kumar P, Maitra G, Das T (2011) Effect of ketamine on Bispectral Index during propofol—fentanyl anesthesia: a randomized controlled study. Middle East J Anaesthesiol 21:391–395
Acknowledgements
We would like to express our sincere gratitude to all those who have supported us throughout the process of this study. And we are deeply grateful to Mr. Gao Zhanghong from the School of Foreign Languages and Literature at Wuhan University, Wuhan, Hubei, China, for his invaluable guidance and expertise in writing this manuscript.
Author information
Authors and Affiliations
Contributions
Z. Y. P. and X. B. R. contributed to the data analysis and manuscript preparation. Z. Y. P., S. A. M., and L. X. R. were involved in data collection. Z. Y. P., L. X. Y., and S. X. M. participated in the study design, and provided critical feedback on the manuscript. And all authors gave final approval for submission.
Corresponding authors
Ethics declarations
Ethics approval
Our research was conducted in adherence to the International Conference on Harmonization Guidelines for Good Clinical Practice and the Declaration of Helsinki, leading to its subsequent approval by the Ethical Board for Clinical/Scientific Research Projects of Zhongnan Hospital of Wuhan University (Permit Number: 2021071). The patients who participated in this study all provided their written informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, Y., Xiong, B., Sang, A. et al. Bispectral Index versus the University of Michigan Sedation Scale in assessing sedation depth during pediatric drug-induced sleep endoscopy. Sleep Breath (2024). https://doi.org/10.1007/s11325-024-03022-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-024-03022-3