Abstract
Neuroplacentology is an expanding field of interest that addresses the placental influence on fetal and neonatal brain lesions and on further neurodevelopment. The objective of this study was to clarify the link between placental pathology and perinatal arterial ischemic stroke (PAIS). Prior publications have reported different types of perinatal stroke with diverse methodologies precluding firm conclusions. We report here the histological placental findings in a series of 16 neonates with radiologically confirmed PAIS. Findings were grouped into 3 categories of lesions: (1) inflammation, (2) placental and fetal hypoxic lesions, and (3) placentas with a high birthweight/placenta weight ratio. Matched control placentas were compared to the pathological placentas when feasible. The eight term singleton placentas were compared to a series of 20 placentas from a highly controlled amniotic membrane donation program; in three twin pregnancies, the placental portions from the affected twin and unaffected co-twin were compared. Slightly more than half (9/16, 56%) had histopathological features belonging to more than one category, a feature shared by the singleton control placentas (13/20, 65%). More severe and extensive lesions were however observed in the pathological placentas. One case occurring in the context of SARS-CoV-2 placentitis further expands the spectrum of COVID-related perinatal disease. Our study supports the assumption that PAIS can result from various combinations and interplay of maternal and fetal factors and confirms the value of placenta examination. Yet, placental findings must be interpreted with caution given their prevalence in well-designed controls.
Similar content being viewed by others
Introduction
In eutherian mammals, the placenta plays a crucial role in the development and survival of the fetus, extending beyond pure fetal development, with the placenta influencing several aspects of a human life into adulthood. The placenta, a key player in fetal programming, has been linked in particular to cardiovascular comorbidities [1], psychiatric disorders such as autism [2], and neurological morbidity [3]. The placental influence on the brain, also known as neuroplacentology, is a growing field of interest [3]. In neonatal hypoxic-ischemic encephalopathy, and specifically in term newborns, histological examination of the placenta may identify clinically overt or silent, preexisting antepartum pathophysiologic processes that may directly cause CNS damage, decrease the threshold for neurologic injury, or serve as markers for a deleterious in utero environment [4, 5]. The role of the placenta is of particular interest in perinatal arterial ischemic stroke (PAIS). PAIS generally remains an isolated event as opposed to stroke occurring later in life, and may be due to local intracranial vascular pathologies, or result from distant embolism from another site such as extracranial vessels, the heart, the umbilical vein, or more likely, from the placenta. Converging evidence identifies the placenta as the main plausible source of emboli to the fetal brain circulation [6, 7], but studies on placenta histopathology in PAIS have been limited for several reasons. First, although the adverse events leading to PAIS occur shortly before birth, the neonate is often asymptomatic at birth which delays diagnosis; the placenta may by then have been discarded. Second, lack of standardization in placental pathology reporting has led to discrepancies between studies. Third, finding appropriate controls is challenging. Control placentas are biased by the pathologies or obstetrical events motivating their analysis, and case–control studies are rare.
In this study, we address the role of placental pathology in a series of 16 neonates diagnosed with PAIS. Histological findings were described according to the Amsterdam consensus terminology [4]. Placenta lesions allowed for classification into 3 distinct categories: (1) inflammation, (2) placental and fetal hypoxic lesions, and (3) placentas with a high birthweight/placenta weight ratio. Whenever feasible, we provide comparison with strictly defined controls.
Materials and methods
Patient selection and characteristics
Infants born in the University Hospital of Geneva over a period of 7 years and 5 months, between October 2016 and March 2023, with a diagnosis of PAIS and whose placentas were available for analysis were enrolled.
Data was retrospectively retrieved from the Swiss Neuropediatric Stroke Registry (SNPSR) for children born before June 2018, while infants born thereafter were prospectively included after parental consent. The SNPSR registry enables access to maternal, fetal, and neonatal data.
PAIS was defined as stroke occurring between the 20th gestational week and the 28th postnatal day of life, with evidence for focal arterial ischemic stroke on a brain MRI performed between days 1 and 25 of life (mean 8.2, median 4). Imaging was performed using a 1.5-T Avanto MRI scanner (Siemens, Erlangen, Germany). No sedation was required. Each MRI protocol included at least the following sequences: 3D T1 mprage, coronal T2 TSE, axial T1 IR, axial susceptibility-weighted image (SWI), and axial diffusion-weighted imaging (DWI) with apparent diffusion coefficient (ADC) map. MRI data were all reassessed by an experienced pediatric neonatal stroke specialist (JF) and a pediatric radiologist (FC) to reach agreement on the nature and localization of the stroke. Lesions were classified according to the classification of perinatal arterial ischemic stroke territory subtypes proposed by Wagenaar et al. [8].
Placenta histology and immunohistochemistry
Placentas were processed according to standard protocol and consensus guidelines [4]. Placental weight was recorded on fresh specimens, after trimming of the extraplacental membranes and umbilical cord. Representative sections and pathological findings from the cord, membranes, and placental disk were sampled. For routine histological examination, 3-μm-thick sections were stained with hematoxylin–eosin (H&E). For immunohistochemistry, SARS-CoV-2 nucleocapsid detection was performed using the Bio SB SARS-CoV-2 BSB-134 clone (Mouse Monoclonal, dilution 1:100).
Pathology criteria
Ascending intrauterine infection, villitis of unknown etiology (VUE), chronic deciduitis, maternal vascular malperfusion (MVM), and fetal vascular malperfusion (FVM) were reported and graded according to the Amsterdam consensus statement [4, 9]. Chorangiosis was defined as ≥ 10 capillaries in ≥ 10 terminal villi in ≥ 10 areas of the placenta using a × 10 objective [10]. Increased syncytial knots was reported when more than 33% of the villi showed knots [4]. Massive perivillous fibrin deposition (MPFD) was defined as perivillous fibrinoid material encasing at least 50% of the villi, extending from the maternal to the fetal surface, on at least one slide [11]. Coexistence of MPFD and trophoblast necrosis with identification of SARS-CoV-2 viral protein in placental tissue was considered as placental destruction and insufficiency from COVID-19 [12, 13].
Classification of the histopathological findings in 3 categories of lesions
We chose to group the findings into 3 distinct categories of lesions:
-
1)
Inflammation
-
2)
Placental and fetal hypoxic lesions
-
3)
Placentas with a high birthweight/placenta weight ratio (BW/PW ratio)
Category 1 includes ascending intrauterine infection, VUE, and chronic deciduitis.
Category 2 includes lesions resulting from oxidative stress and hypoxia to the placenta that may originate from the maternal circulation (i.e., MVM) or the fetal circulation (i.e., FVM) [14]. Since non-perfused/avascular villi encased in MPFD result in impaired fetoplacental circulation and fetal hypoxic-ischemic injury, SARS-CoV-2 placentitis was considered within the hypoxemic category [15]. Villous stromal hemorrhage was indicative of acute hypoxemia. Meconium staining of the membranes and increased circulating nucleated red blood cells (NRBCs) were markers of fetal hypoxia. Finally, chorangiosis and increased extravillous trophoblast (EVT) were considered as adaptive mechanisms to prolonged chronic hypoxia.
Category 3 corresponds to placentas that are small relative to neonatal birthweight.
Selection of controls
Defining “control placentas” is a complex and subjective task. We chose a stringent approach, allowing for the selection of 2 categories of controls:
-
1)
The singleton term placentas from our series were compared to placentas from an amniotic membrane donation program. These control placentas were from highly selected term pregnancies, with no obstetrical or maternal complications. Neonates displayed no neurological symptoms.
-
2)
For twin pregnancies, the placental disk/portion from the unaffected co-twin was used as control.
Results
Clinical characteristics of PAIS cases and controls
Sixteen neonates diagnosed with PAIS were included, 9 males and 7 females. Thirteen were born from singleton pregnancies. Of the three twin pregnancies, only one was spontaneous, the other two pregnancies following oocyte donation, or in vitro fertilization (IVF). Gestational age ranged between 31 + 2 gestational weeks (GW) and 41 + 5 GW, with 2 early preterm births, 5 preterm births, and 9 full-term deliveries. The majority of neonates (12/16) developed neurological symptoms between days 1 and 3 of life; the remaining 4 newborns were diagnosed following brain ultrasound routinely performed in the setting of prematurity.
The clinical characteristics of the PAIS cases and of the controls can be found in supplemental Table S1.
Placenta histopathological findings, neonates with PAIS
The histopathological features of the 16 placentas are summarized in Table 1. Slightly more than half the placentas (9/16, 56%) showed features belonging to more than one category. Representative examples from the 3 categories of lesions are illustrated in Fig. 1.
Illustrative gross and microscopic placenta pathological findings of the main categories of lesions. Associated brain MRI findings are shown. Case P2: inflammation. Ascending intrauterine infection, premature delivery at 33 + 6 GW. A, B Umbilical cord phlebitis (V, umbilical vein) and arteritis (A, umbilical arteries) identify a stage 2, grade 2 fetal inflammatory response (hematoxylin & eosin, H&E, A × 10, B × 60). C Left posterior MCA old infarct seen on axial T1 MRI at day 15. Case P6: hypoxia and high BW/PW. PW < P10, BWP50–P75, and term delivery. D, E On cut section, 20% of the placenta approximately showed large firm whitish areas (D), corresponding histologically to maternal vascular malperfusion (MVM) and large areas of infarction (E, H&E whole-mount view). Areas of villous stromal hemorrhage were consistent with acute hypoxia (F, H&E × 400). G Imaging findings at day 1 demonstrate on DWI massive acute left hemispheric stroke and right MCA stroke. Case P14: hypoxia. Diamniotic-dichorionic twin pregnancy, early premature delivery at 31 + 2 GW. H FVM was seen in the affected twin only. Villous stromal-vascular karyorrhexis, with iron deposition (arrow), and stem vessel obliteration (arrowhead) are shown. I, J Imaging findings (coronal T2 and axial T1) at term demonstrate bilateral porencephalic cavities in the MCA territories, more extensive on the left side
Category 1: inflammation
Evidence of ascending intrauterine infection was seen in 5 singleton placentas (5/16, 31%), one preterm, the other full term, that also displayed histological signs of hypoxia (Category 2 lesions). Two cases showed a S2, G2 fetal inflammatory response, i.e., severe acute umbilical phlebitis and arteritis were seen. The other three placentas showed acute non-severe S1, G1 umbilical phlebitis. One case also displayed high-grade, diffuse VUE.
VUE was seen in two twin placentas.
Category 2: placental and fetal hypoxic lesions
Features consistent with placental and fetal hypoxia were the most frequent findings, (15/16, 94%), consisting mainly of FVM and MVM.
FVM, identified in 7 placentas (7/16, 44%), was high grade in 4 cases, low grade in 2 placentas, and ungradable in the last (Case P8) due to freezing artifacts. The intensity of the lesions was therefore variable, ranging from recent intramural fibrin deposition in stem vessels, to high grade FVM with multiple chorionic plate and stem vessel thromboses, villous stromal-vascular karyorrhexis, and large areas of avascular villi. In one placenta (P12), focal vessel wall calcification was seen, together with umbilical vein, chorionic plate vessel, and stem vessel thrombi. High grade FVM was associated in two cases with signs of an acute hypoxic event to the placenta [16] (villous stromal hemorrhage) and with meconium-laden macrophages in the membranes or increased NRBCs and EVT in one case each. Meconium-laden macrophages in the membrane chorion have been associated with an increased likelihood of oropharyngeal meconium and increased risk of meconium aspiration [17]. Of note, FVM may have been overlooked in the sole placenta without histological evidence for hypoxia (P9), since evaluation was limited by freezing artifacts, the placenta having been sent with delay to the pathology ward. In 4 of the 7 cases with FVM, features of MVM were associated.
MVM without FVM was seen in 6 further cases. Two cases showed associated signs of acute or prolonged chronic hypoxia. Meconium staining of the membranes was also seen.
There is no consensus on the definition of high grade MVM. Provisional criteria consist of a placental weight < 3rd centile with at least one of the following: accelerated villous maturation, distal villous hyperplasia, and multiple infarcts [18]. One preterm singleton placenta (P5) met these criteria.
The one case of SARS-CoV-2-related MPFD showed extensive parenchymal damage, involving more than 80% of the placenta volume, expected to result in fetal hypoxia (P1, Fig. 2). There was no evidence of coexisting chronic histiocytic intervillositis.
Case P1: SARS-CoV-2 infection. A Macroscopic placenta section, early preterm delivery (31 + 4 GW), showing extensive fibrin deposition, involving > 80% of the total placenta volume. B Histology showed partially necrotic chorionic villi encased in fibrin (hematoxylin & eosin, H&E, × 100). C Circumferential cytotrophoblastic and syncytiotrophoblastic reactivity to SARS-CoV-2 nucleocapsid antibody (× 100). D Imaging at day 3 shows acute left MCA infarct on DWI
Finally, excessive EVT and increased syncytial knots consistent with chronic hypoxia, and patchy villous edema were documented in a placenta from a polydrug user (P4, Fig. 3), with prenatal exposure of the neonate.
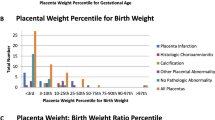
Category 3: placentas with a high BW/PW ratio
Five placentas, one twin and four singleton, were considered small relative to neonatal birthweight. Except for the one placenta with freezing artifact discussed above (P9), all showed features of hypoxia (Category 2), and three also displayed inflammation (Category 3).
Comparison with controls
Term pathological placentas vs. normal term controls from the membrane donation program
Similar to the PAIS placentas, lesions of more than one category were seen in a majority of the control cases (13/20, 65%).
All 20 control placentas showed some degree of hypoxic lesions. MVM was seen in 13 cases (13/20, 65%), and FVM in 9 (9/20, 45%); there was no high grade MVM or FVM. Meconium staining of the membranes was frequent (9/20, 45%). Inflammation was observed in 11 placentas (55%). Ascending intrauterine infection was mild only (S1, G1 maternal/fetal response). Two cases showed high-grade, patchy VUE and five chronic deciduitis (of which only one also had VUE).
Finally, high BW/PW ratio (Category 3 lesions) was seen in 4 cases.
Severe/high grade lesions were seen in the PAIS placentas only, with the exception of high-grade VUE that was seen in both PAIS and control placentas. Statistical significance (p = 0.0398) was reached for severe ascending intrauterine infection, defined as S3 and/or G2 maternal and/or fetal inflammatory response.
Twin placentas: affected twin vs. co-twin
In all three twin pregnancies, one twin developed neonatal stroke, while the co-twin remained unaffected. Signs of hypoxia were seen in both disks/portions from the affected, and unaffected co-twin, but no co-twin portion showed histological features from more than one category. Differences between the two placental disks/portions are reported in detail below.
Placenta #14: early preterm dichorionic-diamniotic twin placenta
The disk from the affected twin showed extensive hypoxic lesions, with high grade FVM, and severe MVM with infarcts, affecting approximately half the placenta disk volume, together with signs of prolonged chronic hypoxia. There were mild differences in relative placental volume, the affected twin receiving 40% of the total volume. Finally, low-grade focal VUE was seen in the affected twin disk only.
Placenta #15: preterm monochorionic-diamniotic twin placenta
The placental portion from the affected twin showed features from all three categories. Volume distribution was highly heterogeneous, with only 20% of the volume attributed to the affected twin. High-grade, patchy VUE was seen in this portion only, as well as low grade FVM. The much larger placental volume devoted to the unaffected twin showed only minor hypoxic features, with peripheral infarcts representing < 2% of the volume (in a preterm placenta however).
Placenta #16: term fused dichorionic-diamniotic twin placenta
The two disks showed chorangiosis (adaptation mechanism) and signs of acute hypoxia. The disk from the affected twin showed additional hypoxic features, meconium staining of the membranes, and decidual arteriopathy.
A comparison of the prevalence of severe or high grade lesions between affected neonates and controls is provided in Table 2. The detailed histological features of the control placentas can be found in Supplemental Tables S2 and S3.
Discussion
Given the nature of our cohort, we will first summarize the general findings, before discussing the conclusions drawn by the case–control groups. Then, we will provide a more in-depth discussion of two cases of particular interest, one with diffuse placental damage due to SARS-CoV-2 infection, the other with chronic hypoxic lesions likely secondary to polydrug abuse.
Hypoxic lesions were as expected the most frequent lesions in PAIS placentas (94%), followed by inflammation (44%). A majority of the PAIS placentas presented concomitant lesions from different categories (56%). Placentas from affected singleton neonates tended to show more severe lesions than controls. Lesions were also more numerous on the affected twin side.
Recent studies have linked several maternal and fetal risk factors to PAIS such as chorioamnionitis or small for gestational age (SGA), suggesting a multifactorial pathogenesis [19,20,21]. This is reflected by different histological findings in our series, which confirm the previous results showing that multiple lesions tend to coexist in neuroplacentology [22]. Multiple lesions were documented not only in our PAIS series but also surprisingly in the control placentas that frequently also displayed lesions belonging to more than one of the three categories (7/13 PAIS singleton placentas, 53%; vs. 13/20 singleton controls, 65%). Multiple patterns of lesions were described in 38.7% of term pregnancies with normal outcome reported by Romero et al. [23]. These results highlight the interpretation complexities, given the presence of some form of placental lesions even in highly controlled pregnancies with no delivery or neonatal complications. However, most lesions in control placentas were mild.
Fetal vascular malperfusion is considered as fetal blood flow obstruction, comprising a group of lesions attributed to absent or reduced perfusion of the villi [9]. FVM has been associated with an increased risk of neonatal encephalopathy and neonatal stroke [24]. FVM was seen in more than one-third of the PAIS placentas and surprisingly in 44% of the controls. The finding of two or more FVM lesions in a placenta is uncommon (< 1%) in normal pregnancies [23]. Although MVM was the most frequent observation, lesion impact was highly variable, ranging from small peripheral infarcts in a term placenta of minor if any significance, to infarcts involving more than half the placenta volume. High-grade or diffuse FVM or MVM lesions were observed in PAIS placentas only. Correlation between adverse clinical outcome and pathological findings is obviously expected to be higher with diffuse and high grade lesions, but other factors creating a favorable context for stroke are also probably at play. Histological features of FVM (thromboses of varying ages, avascular villi…) suggest that lesions evolve during a subacute to chronic period before birth. MVM lesions also exemplified maternal underperfusion manifesting at different time points, both of abrupt onset (infarcts) and gradual onset, of intermediate (increased syncytial knots) or prolonged duration (high BW/PW ratio) [25]. Clinical and imaging findings support the occurrence of PAIS close to the time of birth, including those diagnosed later in infancy. Impaired fetal blood flow and oxygenation secondary to FVM has been postulated to prime the brain to acute injury in the per partum period in conditions that would otherwise have no consequences [26]. A stroke could therefore occur in a neonate with an unfavorable environment, “weakened” by chronic stressors and a pathological placenta, thereby imparting an “acute upon chronic” pattern of lesions [26, 27].
Inflammation was seen in 7 PAIS placentas, of which 3 also had clinical chorioamnionitis. Interestingly, although 7 singleton term control placentas had signs of acute inflammation after elective cesarean section, the maternal and fetal inflammatory responses were never more severe than S1G1. This is in accordance with studies describing the common occurrence of mild acute inflammation (grade 1, stage 1–2, fetal, and maternal inflammatory responses) in normal deliveries [28]. Conversely, umbilical cord arteritis was seen in PAIS placentas only. Involvement of the umbilical arteries (Stage 2 fetal inflammatory response) has been linked to higher rates of adverse neonatal outcome due to higher plasma concentrations of interleukin-6 [29]. In our series, differences in the prevalence of severe ascending intrauterine infection between term singleton PAIS and control placentas reached statistical significance. VUE was seen in both the pathological placentas and the controls and chronic deciduitis in control placentas solely. Chronic placental inflammatory lesions were reported by Romero et al. in 29.9% uncomplicated pregnancies [23]. The association of chorioamnionitis with neonatal brain lesions including stroke is well established [30, 31], but pathogens are rarely identified despite the histopathological diagnosis of chorioamnionitis [22]. Cytokine elevation in inflammation or infection induces prothrombotic events such as endothelial activation, hypercoagulability, platelet activation, and impaired fibrinolysis. The close interaction between the inflammatory and coagulation cascades suggests that inflammation may promote thrombus formation in the placenta, umbilical cord, or other vessels supplying the brain. Cerebral arteries susceptible to stroke show a higher expression of proinflammatory cytokines compared to non-susceptible arteries [32]. Focal arteritis and thrombosis caused by susceptibility to proinflammatory mechanisms may therefore contribute to the inflammatory pathophysiology of stroke.
In the twin cases, more severe and numerous lesions were found on the placental portion of the affected twin. Cases P14 and P15 clearly showed reduced effective placental volume and higher degrees of hypoxic lesions in the affected twin portion. In mild placental insufficiency, the brain’s ability to prioritize oxygen supply is effective in maintaining adequate oxygenation [33]. However, as the hypoxic condition persists, there is a point beyond which cerebral blood vessels no longer vasodilate as effectively, while the resistance to blood flow in the placenta continues to rise. The weight of the two affected twins was below the 10th centile. In severe intrauterine growth restriction (IUGR), the brain’s ability to prioritize oxygen supply eventually fails, leading to the significant clinical challenge of preventing hypoxic brain injury.
Why are certain territories more affected than others? One hypothesis would be that blood flow directed to areas of lower resistance would benefit some areas to the detriment of others.
The characteristics of the two cases illustrated in Figs. 2 and 3, both showing extensive placental involvement, need to be highlighted.
First, in Case P1, neonatal stoke occurred in the context of a SARS-CoV-2 infection, the mother having declined vaccination. COVID-19 is associated with adverse pregnancy outcomes and neonatal complications [34, 35]. SARS-CoV-2 placentitis is defined by the coexistence of 3 histological findings: (1) chronic histiocytic intervillositis, (2) increased fibrin deposition, and (3) trophoblast necrosis [15]. Although not specific to SARS-CoV-2 and of still unclear etiology, MPFD is associated with IUGR, preterm labor, and stillbirth [36, 37]. Severe placental SARS-CoV-2 infection can impact neonatal outcome even in the absence of vertical transmission [38]. Few case reports document severe neurological damage with cystic periventricular leukomalacia in the newborn of mothers with SARS-CoV-2 placentitis [39, 40], but to the best of our knowledge there has been no previous report of SARS-CoV-2 placentitis-associated PAIS.
Extensive and unusual histological findings attributed to the hypoxia category were observed in a premature neonate exposed in utero to cocaine, cannabis, and tobacco (P4). Fetal cocaine exposure has been linked to IUGR, stillbirth, preterm delivery, and placental abruption [41, 42]. The neurotoxic effects of cocaine are potentiated by pyrolysis and are therefore majored with exposure to the smoked form of cocaine (crack cocaine) [41]. Cocaine exerts major vasoconstrictive effects on the uterine vessels resulting in fetal hypoxia, with compensatory increases in blood flow to the fetal brain and heart [43]. Histology in documented cases of cocaine or crack abuse ranges from an absence of specific placental findings [44, 45] to chorionic villus edema and hemorrhage [46]. Hypovascularization of the villi has been potentially ascribed to uteroplacental vasoconstriction and chronic underperfusion [47]. Chronic exposure to tobacco in early pregnancy is also associated with hypoxia, resulting in reduced cytotrophoblastic invasion, and increased EVT islands [48]. The increase in EVT islands was particularly striking in this placenta from a polydrug user. Cells showed nuclear pleomorphism, with irregular and enlarged, hyperchromatic nuclei. These cells are known to become aneuploid from endoreduplication [49]. Pleomorphism is often seen in EVT; it is noteworthy however that ploidy changes may be promoted by hypoxia [50]. The associated patchy villous edema, sufficient to induce placental hypertrophy (placenta weight > P90), may represent further indication of microcirculatory anomalies with flow changes in the fetal circulation [51].
Conclusion
Even though larger cohorts are needed to draw more definitive conclusions on the placental implications in neonatal stroke, our study brings insight into important aspects of the placenta-brain interaction. We describe the occurrence of PAIS in specific clinical contexts, namely, COVID-19 infection, drug abuse, and twin pregnancies. All stroke cases presented some form of placental lesions and compared to controls showed more severe lesions. On the other hand, the presence of significant lesions in healthy control pregnancies points towards an additional multifactorial background permissive to stroke. Multiple elements including perinatal risk factors appear to be implicated in PAIS outcome. Identifying those risk factors and understanding their implication on placental remodeling remains a challenge, which has to be addressed to design potential preventive measures.
Large-scale studies using consensus histology reporting [4, 9] will facilitate future comparisons; in the meantime, we can rely on observational studies to increase our understanding of neuroplacentology.
Data availability
All the data derived from this study are included in the manuscript. Further information can be made available by contacting the last author (anne-laure.rougemont@hug.ch).
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- BW:
-
Birthweight
- CNS:
-
Central nervous system
- CS:
-
Cesarean section
- DWI:
-
Diffusion-weighted imaging
- EVT:
-
Extravillous trophoblast
- FVM:
-
Fetal vascular malperfusion
- G:
-
Grade
- GA:
-
Gestational age
- GW:
-
Gestational weeks
- H&E:
-
Hematoxylin–eosin
- HG:
-
High grade
- ICA:
-
Internal carotid artery
- IUGR:
-
Intrauterine growth restriction
- IVF:
-
In vitro fertilization
- LG:
-
Low-grade
- MAR:
-
Medically assisted reproduction
- MCA:
-
Middle cerebral artery
- MPFD:
-
Massive perivillous fibrin deposition
- MRI:
-
Magnetic resonance imaging
- MVM:
-
Maternal vascular malperfusion
- NRBCs:
-
Nucleated red blood cells
- PAIS:
-
Perinatal arterial ischemic stroke
- PAS:
-
Placenta accreta spectrum
- PROM:
-
Premature rupture of membranes
- PW:
-
Placenta weight
- S:
-
Stage
- SGA:
-
Small for gestational age
- SWI:
-
Susceptibility-weighted image
- SNPSR:
-
Swiss Neuropediatric Stroke Registry
- TTTS:
-
Twin-to-twin transfusion syndrome
- UC:
-
Umbilical cord
- VUE:
-
Villitis of unknown etiology
References
Sallout B, Walker M (2003) The fetal origin of adult diseases. J Obstet Gynaecol 23(5):555–560
Straughen JK et al (2017) The association between placental histopathology and autism spectrum disorder. Placenta 57:183–188
Gardella B et al (2022) What is known about neuroplacentology in fetal growth restriction and in preterm infants: a narrative review of literature. Front Endocrinol (Lausanne) 13:936171
Khong TY et al (2016) Sampling and definitions of placental lesions: Amsterdam placental workshop group consensus statement. Arch Pathol Lab Med 140(7):698–713
Vik T et al (2018) The placenta in neonatal encephalopathy: a case-control study. J Pediatr 202:77-85 e3
Fluss J, Dinomais M, Chabrier S (2019) Perinatal stroke syndromes: similarities and diversities in aetiology, outcome and management. Eur J Paediatr Neurol 23(3):368–383
Kirton A et al (2011) Symptomatic neonatal arterial ischemic stroke: the International Pediatric Stroke Study. Pediatrics 128(6):e1402–e1410
Wagenaar N et al (2018) Promoting neuroregeneration after perinatal arterial ischemic stroke: neurotrophic factors and mesenchymal stem cells. Pediatr Res 83(1–2):372–384
Redline RW, Ravishankar S (2018) Fetal vascular malperfusion, an update. APMIS 126(7):561–569
Altshuler G (1984) Chorangiosis an important placental sign of neonatal morbidity and mortality. Arch Pathol Lab Med 108(1):71–74
Katzman PJ, Genest DR (2002) Maternal floor infarction and massive perivillous fibrin deposition: histological definitions, association with intrauterine fetal growth restriction, and risk of recurrence. Pediatr Dev Pathol 5(2):159–164
Roberts DJ et al (2021) A standardized definition of placental infection by SARS-CoV-2, a consensus statement from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development SARS-CoV-2 Placental Infection Workshop. Am J Obstet Gynecol 225(6):593 e1–593 e9
Watkins JC, Torous VF, Roberts DJ (2021) Defining severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) placentitis. Arch Pathol Lab Med 145(11):1341–1349
Schoots MH et al (2018) Oxidative stress in placental pathology. Placenta 69:153–161
Schwartz DA et al (2022) Placental tissue destruction and insufficiency from COVID-19 causes stillbirth and neonatal death from hypoxic-ischemic injury. Arch Pathol Lab Med 146(6):660–676
Jaiman S et al (2020) Disorders of placental villous maturation in fetal death. J Perinat Med. /j/jpme.ahead-of-print/jpm-2020-0030/jpm-2020-0030.xml. https://doi.org/10.1515/jpm-2020-0030. Online ahead of print
Redline RB, Boyd TK, Roberts DJ (2018) Diagnostic pediatric pathology. Placental and gestational pathology. Cambridge University Press. Chapter 19 Meconium Effects, pp 199–205
Zhou YY et al (2020) Predictors of high grade and other clinically significant placental findings by indication for submission in singleton placentas from term births. Pediatr Dev Pathol 23(4):274–284
Sorg AL et al (2020) Risk factors for perinatal arterial ischaemic stroke: a large case-control study. Dev Med Child Neurol 62(4):513–520
Srivastava R et al (2022) Development and validation of a prediction model for perinatal arterial ischemic stroke in term neonates. JAMA Netw Open 5(6):e2219203
Roy B et al (2020) The role of the placenta in perinatal stroke: a systematic review. J Child Neurol 35(11):773–783
Bernson-Leung ME et al (2018) Placental pathology in neonatal stroke: a retrospective case-control study. J Pediatr 195:39-47 e5
Romero R et al (2018) The frequency and type of placental histologic lesions in term pregnancies with normal outcome. J Perinat Med 46(6):613–630
Spinillo A et al (2023) Placental fetal vascular malperfusion, neonatal neurologic morbidity, and infant neurodevelopmental outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol 229(6):632–640 e2
Redline RW et al (2005) Placental diagnostic criteria and clinical correlation--a workshop report. Placenta 26(Suppl A):S114–7
Volpe JJ (2019) Placental assessment provides insight into mechanisms and timing of neonatal hypoxic-ischemic encephalopathy. J Neonatal Perinatal Med 12(2):113–116
Michoulas A et al (2011) The role of hypoxia-ischemia in term newborns with arterial stroke. Pediatr Neurol 44(4):254–258
Roberts DJ et al (2012) Acute histologic chorioamnionitis at term: nearly always noninfectious. PLoS ONE 7(3):e31819
Kim CJ et al (2001) Umbilical arteritis and phlebitis mark different stages of the fetal inflammatory response. Am J Obstet Gynecol 185(2):496–500
Grether JK, Nelson KB (1997) Maternal infection and cerebral palsy in infants of normal birth weight. JAMA 278(3):207–211
Wu YW et al (2003) Chorioamnionitis and cerebral palsy in term and near-term infants. JAMA 290(20):2677–2684
Giraud A et al (2017) Role of perinatal inflammation in neonatal arterial ischemic stroke. Front Neurol 8:612
Luria O et al (2012) The role of blood flow distribution in the regulation of cerebral oxygen availability in fetal growth restriction. Med Eng Phys 34(3):364–369
Zambrano LD et al (2020) Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-October 3, 2020. MMWR Morb Mortal Wkly Rep 69(44):1641–1647
Zaigham M, Andersson O (2020) Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand 99(7):823–829
Kotiloglu-Karaa E et al (2022) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) placental infection is associated with massive perivillous fibrin deposition at the maternal-fetal interface: a preliminary study. Clin Infect Dis 75(1):e1176–e1179
Redline RW (2021) Extending the spectrum of massive perivillous fibrin deposition (maternal floor infarction). Pediatr Dev Pathol 24(1):10–11
Cribiu FM et al (2021) Severe SARS-CoV-2 placenta infection can impact neonatal outcome in the absence of vertical transmission. J Clin Invest 131(6):e145427. https://doi.org/10.1172/JCI145427
Favre G et al (2021) Decreased fetal movements: a sign of placental SARS-CoV-2 infection with perinatal brain injury. Viruses 13(12):2517. https://doi.org/10.3390/v13122517
Benny M et al (2023) Maternal SARS-CoV-2, placental changes and brain injury in 2 neonates. Pediatrics 151(5):e2022058271. https://doi.org/10.1542/peds.2022-058271
Dos Santos JF et al (2018) Maternal, fetal and neonatal consequences associated with the use of crack cocaine during the gestational period: a systematic review and meta-analysis. Arch Gynecol Obstet 298(3):487–503
Miller CB, Wright T (2018) Investigating mechanisms of stillbirth in the setting of prenatal substance use. Acad Forensic Pathol 8(4):865–873
Pena AE, Burchfield DJ, Abrams RM (1996) Myocardial and cerebral oxygen delivery are not adversely affected by cocaine administration to early-gestation fetal sheep. Am J Obstet Gynecol 174(3):1028–1032
Cejtin HE et al (1999) Effects of cocaine on the placenta. Pediatr Dev Pathol 2(2):143–147
Gilbert WM et al (1990) Lack of specific placental abnormality associated with cocaine use. Am J Obstet Gynecol 163(3):998–999
Mooney EE et al (1998) Placental pathology in patients using cocaine: an observational study. Obstet Gynecol 91(6):925–929
Ortigosa S et al (2012) Feto-placental morphological effects of prenatal exposure to drugs of abuse. Reprod Toxicol 34(1):73–79
Stanek J (2011) Chorionic disk extravillous trophoblasts in placental diagnosis. Am J Clin Pathol 136(4):540–547
Biron-Shental T et al (2012) Endoreduplication in cervical trophoblast cells from normal pregnancies. J Matern Fetal Neonatal Med 25(12):2625–2628
Nelson DA et al (2004) Hypoxia and defective apoptosis drive genomic instability and tumorigenesis. Genes Dev 18(17):2095–2107
Redline RW (2009) Disorders of placental circulation and the fetal brain. Clin Perinatol 36(3):549–559
Funding
Open access funding provided by University of Geneva
Author information
Authors and Affiliations
Contributions
JF and ALR designed the study. JH, FBM, and ALR wrote the manuscript. ALR performed the histological analysis. FC described the imaging findings. JF, FC, and ME selected the cases and controls. All authors critically read the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the Commission Cantonale d’Ethique de la Recherche (CCER:2021–00433), Geneva, Switzerland.
Informed consent
Informed consent was obtained according to national and institutional guidelines.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hirschel, J., Barcos-Munoz, F., Chalard, F. et al. Perinatal arterial ischemic stroke: how informative is the placenta?. Virchows Arch (2024). https://doi.org/10.1007/s00428-024-03780-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00428-024-03780-1