Abstract
Background and Aims
Recent studies point out to epidemiological changes in primary sclerosing cholangitis (PSC). Our aims were to determine in PSC patients followed in several centers in a Mediterranean geographic area: (i) changes in baseline features and (ii) effect of gender on clinical course.
Methods
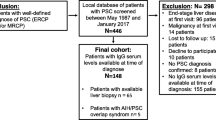
Retrospective multicenter study of PSC patients treated in 8 hospitals in a Mediterranean area between 2000 and 2021. Charts were reviewed compiling demographic, clinical, radiological, and histological variables.
Results
Cohort of 112 PSC patients included, 42% women, 70% diagnosed after 2010. Women were increasingly diagnosed in recent cohorts. The median time from diagnosis to the combined endpoint liver transplantation (Lt) and/or death was 6.9 years. Asthenia at diagnosis (p = 0.009) was associated with lower transplant-free survival, while diagnosis before 2005 was associated with greater LT-free survival (p < 0.001). By Cox regression, LT-free survival was not influenced by age, sex, or cirrhosis at the time of diagnosis. Women were found to have less jaundice at diagnosis (2 vs 14%; p = 0.013), higher prevalence of ANA antibodies (43.9 vs 15.7%; p = 0.003), and lower GGT levels at diagnosis (GGT 123 vs 209U/L; p = 0.014) than men.
Conclusion
In an area traditionally considered to have low prevalence, the prevalence of affected women surpasses expectations based on existing literature. There appear to be gender-related variations in the presentation of the condition, highlighting the need for confirmation through larger-scale studies.


Similar content being viewed by others
Abbreviations
- AIH:
-
Autoimmune hepatitis
- ANA:
-
Antinuclear antibodies
- ANCA:
-
Antineutrophil cytoplasmic antibodies
- anti-LC-1:
-
Liver cytosol-specific antibodies type 1
- AMA:
-
Antimitochondrial antibodies
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- ASGE:
-
American Society for Gastrointestinal Endoscopy
- ASM antibodies:
-
Anti-smooth muscle antibodies
- AST:
-
Aspartate aminotransferase
- CCA:
-
Cholangiocarcinoma
- CD:
-
Crohn disease
- DM:
-
Diabetes mellitus
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- GGT:
-
Gamma-glutamyl transferase
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- IBD:
-
Inflammatory bowel disease
- LKM-1 antibodies:
-
Liver kidney microsomal antibodies
- LT:
-
Liver transplantation
- LTD:
-
Liver transplantation and death
- MRCP:
-
Magnetic resonance cholangiopancreatography
- MRI:
-
Magnetic resonance imaging
- PBC:
-
Primary biliary cholangitis
- PSC:
-
Primary sclerosing cholangitis
- UC:
-
Ulcerative colitis
- UDCA:
-
Ursodeoxycholic acid
References
Berdal JE, Ebbesen J, Rydning A. [Incidence and prevalence of autoimmune liver diseases] Insidens og prevalens av autoimmune leverlidelser. Tidsskr Nor Laegeforen 1998;118:4517e9.
Hirschfield GM, Karlsen TH, Lindor KD, Adams DH. Primary sclerosing cholangitis. Lancet 2013;9:1587–1599. https://doi.org/10.1016/S0140-6736(13)60096-3.
Boonstra K, Beuers U, Ponsioen CY. Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review. J Hepatol 2012;56:1181–1188. https://doi.org/10.1016/j.jhep.2011.10.025.
Palmela C, Peerani F, Castaneda D, Torres J, Itzkowitz SH. Inflammatory bowel disease and primary sclerosing cholangitis: a review of the phenotype and associated specific features. Gut Liver 2018;15:17–29. https://doi.org/10.5009/gnl16510.
Liu JZ, Hov JR, Folseraas T et al. Dense genotyping of immune-related disease regions identifies nine new risk loci for primary sclerosing cholangitis. Nat Genet 2013;45:670–675. https://doi.org/10.1038/ng.2616.
Loftus E, Harewood G, Loftus C et al. PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut. 2005;54:91–96. https://doi.org/10.1136/gut.2004.046615.
Bressler B. Is there an optimal sequence of biologic therapies for inflammatory bowel disease? Therap Adv Gastroenterol. 2023;5:17562848231159452. https://doi.org/10.1177/17562848231159452.
Boonstra K, Weersma RK, van Erpecum KJ et al. Population-based epidemiology, malignancy risk, and outcome of primary sclerosing cholangitis. Hepatology 2013;58:2045–2055. https://doi.org/10.1002/hep.26565.
Alabraba E, Nightingale P, Gunson B et al. A reevaluation of the risk factors for the recurrence of primary sclerosing cholangitis in liver allografts. Liver Transpl 2009;15:330e40. https://doi.org/10.1002/lt.21679.
Lleo A, Jepsen P, Morenghi E et al. Evolving trends in female to male incidence and male mortality of primary biliary cholangitis. Sci Rep 2016;6:25906. https://doi.org/10.1038/srep25906.
Carbone M, Mells GF, Pells G et al. Sex and age are determinants of the clinical phenotype of primary biliary cirrhosis and response to ursodeoxycholic acid. Gastroenterology 2013;144:560–569. https://doi.org/10.1053/j.gastro.2012.12.005.
Al-Chalabi T, Underhill JA, Portmann BC, McFarlane IG, Heneghan MA. Impact of gender on the long-term outcome and survival of patients with autoimmune hepatitis. J Hepatol 2008;48:140–147. https://doi.org/10.1016/j.jhep.2007.08.013.
Gleeson D. Long-term outcomes of autoimmune hepatitis. Clin Liver Dis (Hoboken) 2019;14:24–28. https://doi.org/10.1002/cld.797.
Schwinge D, Schramm C. Sex-related factors in autoimmune liver diseases. SeminImmunopathol 2019;41:165–175. https://doi.org/10.1007/s00281-018-0715-8.
Harms MH, Janssen QP, Adam R et al. Trends in liver transplantation for primary biliary cholangitis in Europe over the past three decades. Aliment PharmacolTher 2019;49:285–295. https://doi.org/10.1111/apt.15060.
Weismüller TJ, Trivedi PJ, Bergquist A et al. Patient age, sex, and inflammatory bowel disease phenotype associate with course of primary sclerosing cholangitis. Gastroenterology 2017;152:1975-1984.e8. https://doi.org/10.1053/j.gastro.2017.02.038.
European Association for the Study of the Liver. EASL clinical practice guidelines on sclerosing cholangitis. J Hepatol 2022;77:761–806. https://doi.org/10.1016/j.jhep.2022.05.011.
Björnsson E, Chari ST, Smyrk TC, Lindor K. Immunoglobulin G4 associated cholangitis: description of an emerging clinical entity based on review of the literature. Hepatology 2007;45:1547–1554. https://doi.org/10.1002/hep.21685.
Abdalian R, Heathcote EJ. Sclerosing cholangitis: a focus on secondary causes. Hepatology 2006;44:1063–1074. https://doi.org/10.1002/hep.21405.
Ponsioen CY. Diagnosis, differential diagnosis, and epidemiology of primary sclerosing cholangitis. Dig Dis 2015;33:134–139. https://doi.org/10.1159/000440823.
Toy E, Balasubramanian S, Selmi C, Li C, Bowlus CL. The prevalence, incidence and natural history of primary sclerosing cholangitis in an ethnically diverse population. BMC Gastroenterol 2011;18:83. https://doi.org/10.1186/1471-230X-11-83.
Bambha K, Kim WR, Talwalkar J et al. Incidence, clinical spectrum, and outcomes of primary sclerosing cholangitis in a United States community. Gastroenterology 2003;125:1364–1369. https://doi.org/10.1016/j.gastro.2003.07.011.
Sclair SN, Little E, Levy E. Current concepts in primary biliary cirrhosis and primary sclerosing cholangitis. Clin Transl Gastroenterol 2015;27:e109. https://doi.org/10.1038/ctg.2015.33.
Molodecky NA, Kareemi H, Parab R et al. Incidence of primary sclerosing cholangitis: a systematic review and meta-analysis. Hepatology 2011;53:1590–1599. https://doi.org/10.1002/hep.24247.
Card TR, Solaymani-Dodaran M, West J. Incidence and mortality of primary sclerosing cholangitis in the UK: a population-based cohort study. J Hepatol 2008;48:939–944. https://doi.org/10.1016/j.jhep.2008.02.017.
Lindkvist B, de Valle MB, Gullberg B, Björnsson E. Incidence and prevalence of primary sclerosing cholangitis in a defined adult population in Sweden. Hepatology 2010;52:571–577. https://doi.org/10.1002/hep.23678.
Bernstein CN, Wajda A, Svenson LW et al. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol 2006;101:1559–1568. https://doi.org/10.1111/j.1572-0241.2006.00603.x.
Kitahora T, Utsunomiya T, Yokota A. Epidemiological study of ulcerative colitis in Japan: incidence and familial occurrence. J Gastroenterol 1995;30:5–8.
Berenguer M, Di Maira T, Baumann U et al. Characteristics, trends and outcomes of liver transplantation for primary sclerosing cholangitis in female vs male patients: an analysis from the European Liver Transplant Registry. Transplantation 2021;105:2255–2262. https://doi.org/10.1097/TP.0000000000003542.
Duclos-Vallee JC, Sebagh M. Recurrence of autoimmune disease, primary sclerosing cholangitis, primary biliary cirrhosis, and autoimmune hepatitis after liver transplantation. Liver Transpl 2009;15:S25-34. https://doi.org/10.1002/lt.21916.
Visseren T, Murad SD. Recurrence of primary sclerosing cholangitis, primary biliary cholangitis and auto-immune hepatitis after liver transplantation. Best Pract Res Clin Gastroenterol 2017;31:187–198. https://doi.org/10.1016/j.bpg.2017.04.004.
Boberg KM, Bergquist A, Mitchell S et al. Cholangiocarcinoma in primary sclerosing cholangitis: risk factors and clinical presentation. Scand J Gastroenterol 2002;37:1205–1211. https://doi.org/10.1080/003655202760373434.
Fevery J, Verslype C, Lai G, Aerts R, Van Steenbergen W. Incidence, diagnosis, and therapy of cholangiocarcinoma in patients with primary sclerosing cholangitis. Dig Dis Sci 2007;52:3123–3135. https://doi.org/10.1007/s10620-006-9681-4.
Tischendorf JJ, Hecker H, Krüger M, Manns MP, Meier PN. Characterization, outcome, and prognosis in 273 patients with primary sclerosing cholangitis: a single center study. Am J Gastroenterol 2007;102:107–114. https://doi.org/10.1111/j.1572-0241.2006.00872.x.
Farrant JM, Hayllar KM, Wilkinson ML et al. Natural history and prognostic variables in primary sclerosing cholangitis. Gastroenterology 1991;100:1710–1717. https://doi.org/10.1016/0016-5085(91)90673-9.
Broome U, Olsson R, Loof L et al. Natural history and prognostic factors in 305 Swedish patients with primary sclerosing cholangitis. Gut 1996;38:610–615. https://doi.org/10.1136/gut.38.4.610.
Karlsen TH, Folseraas T, Thorburn D, Vesterhus M. Primary sclerosing cholangitis—a comprehensive review. J Hepatol 2017;67:1298–1323. https://doi.org/10.1016/j.jhep.2017.07.022.
Funding
This research has not received specific aid from public sector agencies, the commercial sector, or non-profit entities.
Author information
Authors and Affiliations
Contributions
AM and MB equally participated in the design of the study, the analysis, and then drafted the manuscript; IC and TDM participated in the interpretation of the data and critically reviewed the manuscript; CM, LG, SP, MDA, AP, AF, CG, AO, and EG recruited patients for the study and contributed to the critical review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study has been reviewed and approved by the Medicine Research Ethics Committee (CEIM) of H. U. P. La Fe (registration number: 2020-109-1: January 28, 2020). This article does not contain any studies with animals performed by any of the authors.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mínguez, A., Conde, I., Montón, C. et al. Primary Sclerosing Cholangitis: Gender Effects in Valencia’s Low-Prevalence Region. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08368-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08368-y