Abstract
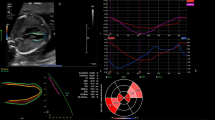
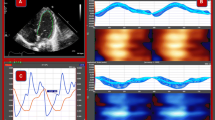
Morphology and function in a fetal heart with severe tricuspid regurgitation remains challenging. The aim of this study was to assess cardiac morphology and function in fetuses with severe tricuspid regurgitation by fetal heart quantification (HQ) and to assess the practical value of fetal HQ. Clinical information was analyzed for 63 pregnant women who underwent fetal cardiac ultrasonography. The women were divided into those who had a fetus with severe tricuspid regurgitation (n = 20) and those with a normal fetus (n = 40). The global sphericity index (GSI), fractional area change (FAC), and global longitudinal strain (GLS) of both ventricles and the sphericity index (SI) and fractional shortening (FS) of 24 segments were quantified by fetal HQ using speckle tracking imaging. Fetuses with severe tricuspid regurgitation had a significantly lower GSI (1.14 ± 0.10 vs. 1.26 ± 0.08, p < 0.001) and a higher GSI Z-score (-0.98 ± 1.01 vs. 0.25 ± 0.87, p < 0.001) as well as a significantly lower right ventricular FAC (36.50 ± 7.34% vs. 45.19 ± 3.39%, p < 0.001), FAC Z-score (-1.02 ± 1.41 vs. 0.49 ± 0.74, p < 0.001), and GLS (-21.01 ± 5.66% vs. 45.19 ± 3.49%, p < 0.001). The SI and SI Z-score were significantly lower in segments 1–18 of the right ventricle in fetuses with severe tricuspid regurgitation (p < 0.05); furthermore, FS of segments 1–12 and 19–24 and the FS Z-score of segments 18–24 were significantly lower in fetuses with severe tricuspid regurgitation (p < 0.05). Fetal HQ is useful for evaluation of cardiac morphology and function in fetuses with severe tricuspid regurgitation and can provide important reference information for both clinical diagnosis and treatment.





Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in the article. Further enquiries can be directed to the corresponding author.
References
Scala C et al (2017) Fetal tricuspid regurgitation in the First Trimester as a screening marker for congenital heart defects: systematic review and Meta-analysis. Fetal Diagn Ther 42(1):1–8. https://doi.org/10.1159/000455947
Pereira S et al (2011) Contribution of fetal tricuspid regurgitation in first-trimester screening for major cardiac defects. Obstet Gynecol 117(6):1384–1391. https://doi.org/10.1097/AOG.0b013e31821aa720
Zhou J et al (2014) Relationship between isolated mild tricuspid valve regurgitation in second-trimester fetuses and postnatal congenital cardiac disorders. J Ultrasound Med 33(9):1677–1682. https://doi.org/10.7863/ultra.33.9.1677
Wang TKM, Unai S, Xu B (2021) Contemporary review in the multi-modality imaging evaluation and management of tricuspid regurgitation. Cardiovasc Diagn Ther 11(3):804–817. https://doi.org/10.21037/cdt.2020.01.06
Xu J et al (2021) Risk factors for postoperative recurrent tricuspid regurgitation after concomitant tricuspid annuloplasty during left heart surgery and the association between tricuspid annular circumference and secondary tricuspid regurgitation. BMC Cardiovasc Disord 21(1):50. https://doi.org/10.1186/s12872-021-01870-5
Tchantchaleishvili V, Rajab TK, Cohn LH (2017) Posterior suture annuloplasty for functional tricuspid regurgitation. Ann Cardiothorac Surg 6(3):262–265. https://doi.org/10.21037/acs.2017.05.04
Hahn RT (2016) State-of-the-art review of Echocardiographic Imaging in the evaluation and treatment of functional tricuspid regurgitation. Circ Cardiovasc Imaging 9(12):e005332. https://doi.org/10.1161/circimaging.116.005332
Lee SH et al (2022) Clinical significance of right ventricular-pulmonary arterial coupling in patients with tricuspid regurgitation before closure of atrial septal defect. Front Cardiovasc Med 9:896711. https://doi.org/10.3389/fcvm.2022.896711
Dong SZ, Zhu M (2016) MR imaging of fetal cardiac malposition and congenital cardiovascular anomalies on the four-chamber view. Springerplus 5(1):1214. https://doi.org/10.1186/s40064-016-2833-x
An S et al (2021) Fetal heart and descending aorta detection in four-Chamber View of fetal Echocardiography. Annu Int Conf IEEE Eng Med Biol Soc 2021:2722–2725. https://doi.org/10.1109/embc46164.2021.9630562
Liu H et al (2022) Diagnosis of fetal congenitally unguarded tricuspid valve orifice by echocardiography. Echocardiography 39(10):1324–1327. https://doi.org/10.1111/echo.15457
Luo L et al (2021) Quantitative evaluation of fetal ventricular function by speckle tracking echocardiography. Echocardiography 38(11):1924–1931. https://doi.org/10.1111/echo.15240
Nogué L et al (2022) Feasibility of 4D-Spatio temporal image correlation (STIC) in the Comprehensive Assessment of the fetal heart using FetalHQ(®). J Clin Med 11(5):1414. https://doi.org/10.3390/jcm11051414
Nakata M et al (2020) Assessment of fetal cardiac function with echocardiography. J Obstet Gynaecol Res 46(1):31–38. https://doi.org/10.1111/jog.14143
Mondillo S et al (2011) Speckle-tracking echocardiography: a new technique for assessing myocardial function. J Ultrasound Med 30(1):71–83. https://doi.org/10.7863/jum.2011.30.1.71
Cho MJ (2022) Right atrial mechanics on Speckle-Tracking Echocardiography: clinical implications in children. J Cardiovasc Imaging 30(2):123–124. https://doi.org/10.4250/jcvi.2021.0192
Enzensberger C et al (2014) Assessment of fetal cardiac function–established and novel methods. Z Geburtshilfe Neonatol 218(2):56–63. https://doi.org/10.1055/s-0034-1371849
DeVore GR et al (2018) 24-segment sphericity index: a new technique to evaluate fetal cardiac diastolic shape. Ultrasound Obstet Gynecol 51(5):650–658. https://doi.org/10.1002/uog.17505
Hata T et al (2020) Evaluation of 24-segment sphericity index of fetal heart using FetalHQ. J Matern Fetal Neonatal Med 1–7. https://doi.org/10.1080/14767058.2020.1856808
Scheier M et al (2010) Prediction of fetal anemia in rhesus disease by measurement of fetal middle cerebral artery peak systolic velocity. Ultrasound Obstet Gynecol 23(5):432–436
Al-Bawardy R et al (2013) Tricuspid regurgitation in patients with pacemakers and implantable cardiac defibrillators: a comprehensive review. Clin Cardiol 36(5):249–254. https://doi.org/10.1002/clc.22104
Shen Y et al (2022) A preliminary study on fetal cardiac morphology and systolic function of normal and anemic pregnant women by fetal heart quantification technology. Transl Pediatr 11(8):1336–1345. https://doi.org/10.21037/tp-22-315
DeVore GR (2017) Computing the Z score and Centiles for cross-sectional analysis: a practical Approach. J Ultrasound Med 36(3):459–473
Prihadi EA et al (2019) Morphologic types of Tricuspid Regurgitation: characteristics and prognostic implications. JACC Cardiovasc Imaging 12(3):491–499. https://doi.org/10.1016/j.jcmg.2018.09.027
Cruz-Lemini M et al (2016) Fetal cardiovascular remodeling persists at 6 months in infants with intrauterine growth restriction. Ultrasound Obstet Gynecol 48(3):349–356. https://doi.org/10.1002/uog.15767
DeVore GR, Satou G, Sklansky M (2017) Abnormal fetal findings Associated with a global sphericity index of the 4-Chamber View below the 5th Centile. J Ultrasound Med 36(11):2309–2318. https://doi.org/10.1002/jum.14261
Wang D et al (2021) Evaluation of prenatal changes in fetal cardiac morphology and function in maternal diabetes mellitus using a novel fetal speckle-tracking analysis: a prospective cohort study. Cardiovasc Ultrasound 19(1):25. https://doi.org/10.1186/s12947-021-00256-z
Lee W et al (2022) Cardiac size, shape, and ventricular contractility in fetuses at Sea Level with an estimated weight less-than 10th Centile. J Ultrasound Med. https://doi.org/10.1002/jum.15954
Torigoe F et al (2020) Fetal echocardiographic prediction score for perinatal mortality in tricuspid valve dysplasia and Ebstein’s anomaly. Ultrasound Obstet Gynecol 55(2):226–232. https://doi.org/10.1002/uog.20302
Acknowledgements
We thank Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the English text of a draft of this manuscript.
Funding
This study was supported by General Cooperative Research Program of The Sci-Tech Academy of Zhejiang University (ZJU Cooperation No. 2021-KYY- 518053-0055).
Author information
Authors and Affiliations
Contributions
YL and BZ conducted the experiments and wrote the main manuscript. MP, LH, and XL analyzed the data and prepared figures. XZ and XP provided the experimental resources. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical Approval
The study protocol was reviewed and approved by ethics committee of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine (approval number ZJSM-2020-0316).
Consent to Participate
Written informed consent was obtained from all study participants.
Conflict of Interest
The authors declare that they have no conflicts of interest. All authors contributed to the article and approved the submitted version.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lou, Y., Zhao, B., Pan, M. et al. Quantitative Analysis of Morphology and Function in the Fetal Heart with Severe Tricuspid Regurgitation by Speckle Tracking Imaging. Pediatr Cardiol 45, 740–748 (2024). https://doi.org/10.1007/s00246-024-03454-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-024-03454-4