Abstract
Background
Data are limited on the safety and efficacy of combining advanced therapies for refractory patients with IBD.
Aim
To evaluate the real-world efficacy and safety of dual advanced therapy (DAT), combining 2 biologics or a biologic with a small molecule, in children and young adults with refractory IBD.
Methods
Primary outcome of this single IBD center cohort was DAT remission (clinical and biomarker remission) at first assessment (T1). Secondary outcomes included remission at T2, if DAT de-intensification (De-I) occurred and T3, if T2 DAT re-intensification (Re-I) occurred. Efficacy and safety outcomes were described.
Results
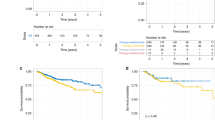
Of the 30 patients [43% female, 30% CD, median age of 18.3 [15.1–19.8] years], all 11 UST + TOFA achieved T1 remission; 6/10 De-I failed at T2; and 4/4 Re-I achieved T3 remission. Of 9 VDZ + TOFA, 6 achieved T1 remission; 5/6 De-I failed at T2; and 1/1 failed T3 Re-I. Of 4 UST + VDZ, 3 achieved T1 remission; 2/3 De-I failed at T2; and 0 had Re-I. Of 5 UST + UPA, 4 achieved T1 remission; 1/5 De-I failed at T2 but recaptured T3 remission post-Re-I. One VDZ + OZA achieved T1 remission and maintained T2 remission post-De-I to OZA monotherapy. At last follow-up, 43% were on original DAT, 17% on one of original DAT, and 40% neither. One UST + TOFA patient developed mild leukopenia and another developed septic arthritis and venous thromboembolism on VDZ + TOFA and prednisone.
Conclusion
Most children and young adults treated with DAT achieved remission with minimal safety events; however, de-intensification had limited success.

Similar content being viewed by others
References
Kayal M, Posner H, Spencer E, Colombel J-F, Stalgis C, Ungaro RC. Net remission rates with biologic and small molecule treatment in ulcerative colitis: a reappraisal of the clinical trial data. Clin Gastroenterol Hepatol. 2023;21:3433-3436.e1.
Kayal M, Ungaro RC, Bader G, Colombel J-F, Sandborn WJ, Stalgis C. Net remission rates with biologic treatment in Crohn’s disease: a reappraisal of the clinical trial data. Clin Gastroenterol Hepatol. 2023;21:1348–1350.
Ferrante M, Panaccione R, Baert F, Bossuyt P, Colombel J-F, Danese S et al. Risankizumab as maintenance therapy for moderately to severely active Crohn’s disease: results from the multicentre, randomised, double-blind, placebo-controlled, withdrawal phase 3 FORTIFY maintenance trial. Lancet. 2022;399:2031–2046.
Stalgis C, Deepak P, Mehandru S, Colombel J-F. Rational combination therapy to overcome the plateau of drug efficacy in inflammatory bowel disease. Gastroenterology. 2021;161:394–399.
Feagan BG, Sands BE, Sandborn WJ, Germinaro M, Vetter M, Shao J et al. Guselkumab plus golimumab combination therapy versus guselkumab or golimumab monotherapy in patients with ulcerative colitis (VEGA): a randomised, double-blind, controlled, phase 2, proof-of-concept trial. Lancet Gastroenterol Hepatol. 2023;8:307–320.
Panaccione R, Ghosh S, Middleton S, Márquez JR, Scott BB, Flint L et al. Combination therapy with infliximab and azathioprine is superior to monotherapy with either agent in ulcerative colitis. Gastroenterology. 2014;146:392-400.e3.
Hirten RP, Iacucci M, Shah S, Ghosh S, Colombel J-F. Combining biologics in inflammatory bowel disease and other immune mediated inflammatory disorders. Clin Gastroenterol Hepatol. 2018;16:1374–1384.
Feagan BG, McDonald JWD, Panaccione R, Enns RA, Bernstein CN, Ponich TP et al. Methotrexate in combination with infliximab is no more effective than infliximab alone in patients with Crohn’s disease. Gastroenterology. 2014;146:681-688.e1.
Kappelman MD, Wohl DA, Herfarth HH, Firestine AM, Adler J, Ammoury RF et al. Comparative effectiveness of anti-TNF in combination with low-dose methotrexate vs anti-TNF monotherapy in pediatric Crohn’s disease: a pragmatic randomized trial. Gastroenterology. 2023;165:149-161.e7.
Yang E, Panaccione N, Whitmire N, Dulai PS, Vande Casteele N, Singh S et al. Efficacy and safety of simultaneous treatment with two biologic medications in refractory Crohn’s disease. Aliment Pharmacol Ther. 2020;51:1031–1038.
Ahmed W, Galati J, Kumar A, Christos PJ, Longman R, Lukin DJ et al. Dual biologic or small molecule therapy for treatment of inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2022;20:e361–e379.
Moon JS. Clinical aspects and treatments for pediatric inflammatory bowel diseases. Pediatr Gastroenterol Hepatol Nutr. 2019;22:50.
Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015;169:1053.
Olbjørn C, Rove JB, Jahnsen J. Combination of biological agents in moderate to severe pediatric inflammatory bowel disease: a case series and review of the literature. Pediatric Drugs. 2020;22:409–416.
Dolinger MT, Spencer EA, Lai J, Dunkin D, Dubinsky MC. Dual biologic and small molecule therapy for the treatment of refractory pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2021;27:1210–1214.
Wlazło M, Meglicka M, Wiernicka A, Osiecki M, Kierkuś J. Dual biologic therapy in moderate to severe pediatric inflammatory bowel disease: a retrospective study. Children. 2022;10:11.
Yerushalmy-Feler A, Olbjorn C, Kolho K-L, Aloi M, Musto F, Martin-de-Carpi J et al. Dual biologic or small molecule therapy in refractory pediatric inflammatory bowel disease (DOUBLE-PIBD): a multicenter study from the Pediatric IBD Porto Group of ESPGHAN. Inflamm Bowel Dis. 2023. https://doi.org/10.1093/ibd/izad064.
Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1:514.
Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. N Engl J Med. 1987;317:1625–1629.
Yu A, Ha NB, Shi B, Cheng Y-W, Mahadevan U, Beck KR. Real-world experience with tofacitinib dose de-escalation in patients with moderate and severe ulcerative colitis. Clin Gastroenterol Hepatol. 2023;21:3115-3124.e3.
Wetwittayakhlang P, Lakatos PL. Current evidence for combined targeted therapy for the treatment of inflammatory bowel disease. J Can Assoc Gastroenterol. 2023. https://doi.org/10.1093/jcag/gwad032.
Spencer EA, Bergstein S, Dolinger M, Pittman N, Kellar A, Dunkin D et al. Single-center experience with upadacitinib for adolescents with refractory inflammatory bowel disease. Inflamm Bowel Dis. 2023. https://doi.org/10.1093/ibd/izad300.
Author information
Authors and Affiliations
Contributions
AK: conducted the study, collected and interpreted the data, and drafted the manuscript; MTD: collected the data and edited the manuscript; EAS: collected the data and edited the manuscript; MCD: conceptualized and planned the study, interpreted the data, and reviewed and edited the manuscript. Each author has approved the final draft of the manuscript submitted.
Corresponding author
Ethics declarations
Conflict of interest
Michael T. Dolinger: Consulting fees from Neurologica, a subsidiary of Samsung electronics co., ltd, Pfizer, and BMS. Marla C. Dubinsky: Consulting fees from Abbvie, Abivax, AstraZeneca, Boehringer Ingelheim, Geneoscopy, Janssen, Lilly, Merck, Pfizer, Prometheus Biosciences, Prometheus Labs, Takeda. Amelia Kellar: Nothing to disclose. Elizabeth A. Spencer: Nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kellar, A., Dolinger, M.T., Spencer, E.A. et al. Real-World Outcomes of Dual Advanced Therapy in Children and Young Adults with Inflammatory Bowel Disease. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08379-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08379-9