Abstract
Background
The post-reflux swallow-induced peristaltic wave (PSPW) brings salivary bicarbonate to neutralize residual distal esophageal mucosal acidification.
Aims
To determine if reduced saliva production and esophageal body hypomotility would compromise PSPW-induced pH recovery in the distal esophagus.
Methods
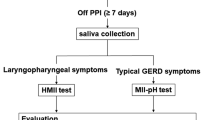
In this multicenter retrospective cross-sectional study, patients with confirmed Sjogren’s syndrome and scleroderma/mixed connective tissue disease (MCTD) who underwent high resolution manometry (HRM) and ambulatory pH-impedance monitoring off antisecretory therapy were retrospectively identified. Patients without these disorders undergoing HRM and pH-impedance monitoring for GERD symptoms were identified from the same time-period. Acid exposure time, numbers of reflux episodes and PSPW, pH recovery with PSPW, and HRM metrics were extracted. Univariate comparisons and multivariable analysis were performed to determine predictors of pH recovery with PSPW.
Results
Among Sjogren’s syndrome (n = 34), scleroderma/MCTD (n = 14), and comparison patients with reflux symptoms (n = 96), the scleroderma/MCTD group had significantly higher AET, higher prevalence of hypomotility, lower detected reflux episodes, and very low numbers of PSPW (p ≤ 0.004 compared to other groups). There was no difference in pH-impedance metrics between Sjogren’s syndrome, and comparison patients (p ≥ 0.481). Proportions with complete pH recovery with PSPW was lower in Sjogren’s patients compared to comparison reflux patients (p = 0.009), predominantly in subsets with hypomotility (p < 0.001). On multivariable analysis, diagnosis of Sjogren’s syndrome, scleroderma/MCTD or neither (p = 0.014) and esophageal hypomotility (p = 0.024) independently predicted lack of complete pH recovery with PSPW, while higher total reflux episodes trended (p = 0.051).
Conclusions
Saliva production and motor function are both important in PSPW related pH recovery.
Graphical Abstract




Similar content being viewed by others
References
Vakil N, van Zanten SV, Kahrilas P et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006;101:1900–1943.
Gyawali CP, Kahrilas PJ, Savarino E et al. Modern diagnosis of GERD: the Lyon Consensus. Gut 2018;67:1351–1362.
Gyawali CP, Yadlapati R, Fass R et al. Updates to the modern diagnosis of GERD: Lyon consensus 2.0. Gut. 2023. https://doi.org/10.1136/gutjnl-2023-330616.
Locke GR 3rd, Talley NJ, Fett SL et al. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County Minnesota. Gastroenterology 1997;112:1448–1456.
El-Serag HB, Sweet S, Winchester CC et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2014;63:871–880.
Tack J, Pandolfino JE. Pathophysiology of Gastroesophageal Reflux Disease. Gastroenterology 2018;154:277–288.
Sifrim D, Roman S, Savarino E et al. Normal values and regional differences in oesophageal impedance-pH metrics: a consensus analysis of impedance-pH studies from around the world. Gut. 2020. https://doi.org/10.1136/gutjnl-2020-322627.
Rogers BD, Valdovinos LR, Crowell MD et al. Number of reflux episodes on pH-impedance monitoring associates with improved symptom outcome and treatment satisfaction in gastro-oesophageal reflux disease (GERD) patients with regurgitation. Gut 2021;70:450–455.
Gyawali CP, Tutuian R, Zerbib F et al. Value of pH Impedance Monitoring While on Twice-Daily Proton Pump Inhibitor Therapy to Identify Need for Escalation of Reflux Management. Gastroenterology 2021;161:1412–1422.
Mittal RK, Balaban DH. The esophagogastric junction. N Engl J Med 1997;336:924–932.
Vegesna AK, Sloan JA, Singh B et al. Characterization of the distal esophagus high-pressure zone with manometry, ultrasound and micro-computed tomography. Neurogastroenterol Motil 2013;25(53–60):e6.
Helm JF, Dodds WJ, Pelc LR et al. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med 1984;310:284–288.
Helm JF, Dodds WJ, Riedel DR et al. Determinants of esophageal acid clearance in normal subjects. Gastroenterology 1983;85:607–612.
Sarosiek J, Rourk RM, Piascik R et al. The effect of esophageal mechanical and chemical stimuli on salivary mucin secretion in healthy individuals. Am J Med Sci 1994;308:23–31.
Xu H, Ye B, Ding Y et al. Factors of Reflux Episodes With Post-reflux Swallow-induced Peristaltic Wave in Gastroesophageal Reflux Disease. J Neurogastroenterol Motil 2020;26:378–383.
Frazzoni M, Manta R, Mirante VG et al. Esophageal chemical clearance is impaired in gastro-esophageal reflux disease–a 24-h impedance-pH monitoring assessment. Neurogastroenterol Motil 2013;25:399–406.
Frazzoni M, Bertani H, Manta R et al. Impairment of chemical clearance is relevant to the pathogenesis of refractory reflux oesophagitis. Dig Liver Dis 2014;46:596–602.
Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am 2014;24:527–543.
Yadlapati R, Kahrilas PJ, Fox MR et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil 2021;33:e14058.
Gyawali CP, Rogers B, Frazzoni M et al. Inter-reviewer Variability in Interpretation of pH-Impedance Studies: The Wingate Consensus. Clin Gastroenterol Hepatol 2021;19:1976–1978.
Frazzoni M, Savarino E, de Bortoli N et al. Analyses of the Post-reflux Swallow-induced Peristaltic Wave Index and Nocturnal Baseline Impedance Parameters Increase the Diagnostic Yield of Impedance-pH Monitoring of Patients With Reflux Disease. Clin Gastroenterol Hepatol 2016;14:40–46.
Frazzoni L, Frazzoni M, de Bortoli N, et al. Postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance can link PPI-responsive heartburn to reflux better than acid exposure time. Neurogastroenterol Motil 2017;29.
Zhang M, Yaman B, Roman S et al. Post-reflux swallow-induced peristaltic wave (PSPW): physiology, triggering factors and role in reflux clearance in healthy subjects. J Gastroenterol 2020;55:1109–1118.
Gyawali CP, Yadlapati R, Fass R, et al. Updates to the modern diagnosis of GERD: Lyon Consensus 2.0. Gut 2023:in press.
Thomas E, Hay EM, Hajeer A et al. Sjogren’s syndrome: a community-based study of prevalence and impact. Br J Rheumatol 1998;37:1069–1076.
Ramos-Casals M, Tzioufas AG, Font J. Primary Sjogren’s syndrome: new clinical and therapeutic concepts. Ann Rheum Dis 2005;64:347–354.
Baldini C, Pepe P, Quartuccio L et al. Primary Sjogren’s syndrome as a multi-organ disease: impact of the serological profile on the clinical presentation of the disease in a large cohort of Italian patients. Rheumatology (Oxford) 2014;53:839–844.
Lepri G, Guiducci S, Bellando-Randone S et al. Evidence for oesophageal and anorectal involvement in very early systemic sclerosis (VEDOSS): report from a single VEDOSS/EUSTAR centre. Ann Rheum Dis 2015;74:124–128.
Denton CP, Khanna D. Systemic sclerosis. Lancet 2017;390:1685–1699.
Crowell MD, Umar SB, Griffing WL et al. Esophageal Motor Abnormalities in Patients With Scleroderma: Heterogeneity, Risk Factors, and Effects on Quality of Life. Clin Gastroenterol Hepatol 2017;15:207–213.
Shreiner AB, Murray C, Denton C et al. Gastrointestinal Manifestations of Systemic Sclerosis. J Scleroderma Relat Disord 2016;1:247–256.
Sharp GC, Irvin WS, Tan EM et al. Mixed connective tissue disease–an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am J Med 1972;52:148–159.
Gutierrez F, Valenzuela JE, Ehresmann GR et al. Esophageal dysfunction in patients with mixed connective tissue diseases and systemic lupus erythematosus. Dig Dis Sci 1982;27:592–597.
Funding
This study was funded in part by the Jewish Heritage Fund for Excellence (BDR).
Author information
Authors and Affiliations
Contributions
Guarantor of the article: CPG. Author roles: LM, TH: data collection, data analysis, manuscript review; BDR: data analysis, manuscript preparation and review; DS, CPG: study concept, data collection and analysis, manuscript preparation and review, and critical review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
LM, TH: no disclosures; BDR: Braintree Labs (consulting); DS: Reckkit Benkiser, UK, Jinshang China (honorarium, research grants); CPG: Consulting: Medtronic, Diversatek; speaking: Carnot.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marchetti, L., Rogers, B.D., Hengehold, T. et al. Saliva Production and Esophageal Motility Influence Esophageal Acid Clearance Related to Post-reflux Swallow-Induced Peristaltic Wave. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08315-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08315-x