Abstract
Purpose
Distress Thermometer (DT) was adopted to evaluate distress in neuro-oncology on a scale from 1 to 10. DT values above 4 indicate major distress and should initiate psycho(onco)logical co-therapy. However, data about peri-operative distress is scarce. Hence, we evaluated peri-operative distress levels in a neurosurgical patient cohort with various intracranial tumors using the DT.
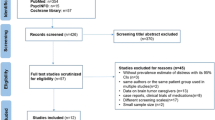
Methods
We conducted a retrospective study including inpatients with brain tumors who underwent surgery in our department between October 2015 and December 2019. Patients were routinely assessed for distress using the DT before or after initial surgery. A comparative analysis was performed via Wilcoxon rank-sum test.
Results
254 patients were eligible. Mean DT value of the entire cohort was 5.4 ± 2.4. 44.5% (n = 114) of all patients exceeded DT values of ≥ 6. In our cohort, poor post-operative neurological performance and occurrence of motor deficits were significantly associated with major distress. When analysed for peri-operative changes, DT values significantly declined within the male sub-cohort (6.0 to 4.6, p = 0.0033) after surgery but remained high for the entire cohort (5.7 and 5.3, p = 0.1407). Sub-cohort analysis for other clinical factors revealed no further significant changes in peri-operative distress.
Conclusion
Distress levels were high across the entire cohort which indicated a high need for psychological support. Motor deficits and poor post-operative neurological performance were significantly associated with DT values above 6. Distress levels showed little peri-operative variation.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CNS:
-
Central Nervous System
- DT:
-
Distress Thermometer
- HRQoL:
-
Health-related quality of live
- KPS:
-
Karnofsky Performance Status
- MRC-NPS:
-
Medical Research Council-Neurological Performance Status
References
Ostrom QT, Price M, Neff C et al (2023) CBTRUS Statistical Report: primary brain and other Central Nervous System tumors diagnosed in the United States in 2016–2020. Neurooncology 25:iv1–iv99. https://doi.org/10.1093/neuonc/noad149
Cagney DN, Martin AM, Catalano PJ et al (2017) Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neurooncology 19:1511–1521. https://doi.org/10.1093/neuonc/nox077
Carlson LE, Angen M, Cullum J et al (2004) High levels of untreated distress and fatigue in cancer patients. Br J Cancer 90:2297–2304. https://doi.org/10.1038/sj.bjc.6601887
Randazzo D, Peters KB (2016) Psychosocial distress and its effects on the health-related quality of life of primary brain tumor patients. CNS Oncol 5:241–249. https://doi.org/10.2217/cns-2016-0010
Fehrenbach MK, Brock H, Mehnert-Theuerkauf A et al (2021) Psychological distress in intracranial neoplasia: a comparison of patients with Benign and Malignant Brain Tumours. Front Psychol 12:664235. https://doi.org/10.3389/fpsyg.2021.664235
Boyes A, Newell S, Girgis A et al (2006) Does routine assessment and real-time feedback improve cancer patients’ psychosocial well-being? Eur J Cancer Care (Engl) 15:163–171. https://doi.org/10.1111/j.1365-2354.2005.00633.x
Goebel S, Stark AM, Kaup L et al (2011) Distress in patients with newly diagnosed brain tumours. Psychooncology 20:623–630. https://doi.org/10.1002/pon.1958
Renovanz M, Gutenberg A, Haug M et al (2013) Postsurgical screening for psychosocial disorders in neurooncological patients. Acta Neurochir (Wien) 155:2255–2261. https://doi.org/10.1007/s00701-013-1884-9
Rapp M, Schipmann S, Hoffmann K et al (2018) Impact of distress screening algorithm for psycho-oncological needs in neurosurgical patients. Oncotarget 9:31650–31663. https://doi.org/10.18632/oncotarget.25833
Weis J, Mehnert-Theuerkauf A (2023) S3-Leitlinie psychoonkologische Diagnostik, Beratung Und Behandlung Von Erwachsenen Krebspatient*innen. https://register.awmf.org/de/leitlinien/detail/032-051OL
Philip J, Collins A, Panozzo S et al (2020) Mapping the nature of distress raised by patients with high-grade glioma and their family caregivers: a descriptive longitudinal study. Neurooncol Pract 7:103–110. https://doi.org/10.1093/nop/npz032
Singer S, Roick J, Danker H et al (2018) Psychiatric co-morbidity, distress, and use of psycho-social services in adult glioma patients-a prospective study. Acta Neurochir (Wien) 160:1187–1194. https://doi.org/10.1007/s00701-018-3527-7
Bleehen NM, Stenning SP (1991) A Medical Research Council trial of two radiotherapy doses in the treatment of grades 3 and 4 astrocytoma. The Medical Research Council Brain Tumour Working Party. Br J Cancer 64:769–774. https://doi.org/10.1038/bjc.1991.396
Weller M, van den Bent M, Tonn JC et al (2017) European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol 18:e315–e329. https://doi.org/10.1016/S1470-2045(17)30194-8
Goldbrunner R, Minniti G, Preusser M et al (2016) EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 17:e383–e391. https://doi.org/10.1016/S1470-2045(16)30321-7
Hoang-Xuan K, Bessell E, Bromberg J et al (2015) Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: guidelines from the European Association for Neuro-Oncology. Lancet Oncol 16:e322–e332. https://doi.org/10.1016/S1470-2045(15)00076-5
Mehnert A, Müller D, Lehmann C et al (2006) Die deutsche Version Des NCCN distress-thermometers. Z für Psychiatrie Psychologie und Psychother 54:213–223. https://doi.org/10.1024/1661-4747.54.3.213
Goebel S, Mehdorn HM (2011) Measurement of psychological distress in patients with intracranial tumours: the NCCN distress thermometer. J Neurooncol 104:357–364. https://doi.org/10.1007/s11060-010-0501-5
Armstrong TS, Vera-Bolanos E, Acquaye AA et al (2016) The symptom burden of primary brain tumors: evidence for a core set of tumor- and treatment-related symptoms. Neurooncology 18:252–260. https://doi.org/10.1093/neuonc/nov166
Wick W (2023) Leitlinien für Diagnostik und Therapie in der Neurologie: Gliome. https://www.awmf.org/leitlinien/detail/ll/030-099.html. Accessed 03 Dec 2023
Rooney AG, McNamara S, Mackinnon M et al (2013) The frequency, longitudinal course, clinical associations, and causes of emotional distress during primary treatment of cerebral glioma. Neurooncology 15:635–643. https://doi.org/10.1093/neuonc/not009
Goebel S, Strenge H, Mehdorn HM (2012) Acute stress in patients with brain cancer during primary care. Support Care Cancer 20:1425–1434. https://doi.org/10.1007/s00520-011-1225-6
Amidei C, Kushner DS (2015) Clinical implications of motor deficits related to brain tumors†. Neurooncol Pract 2:179–184. https://doi.org/10.1093/nop/npv017
Boele FW, Klein M, Reijneveld JC et al (2014) Symptom management and quality of life in glioma patients. CNS Oncol 3:37–47. https://doi.org/10.2217/cns.13.65
Brown PD, Ballman KV, Rummans TA et al (2006) Prospective study of quality of life in adults with newly diagnosed high-grade gliomas. J Neurooncol 76:283–291. https://doi.org/10.1007/s11060-005-7020-9
Kasper J, Wende T, Fehrenbach MK et al (2021) The Prognostic Value of NANO Scale Assessment in IDH-Wild-Type Glioblastoma patients. Front Oncol 11:790458. https://doi.org/10.3389/fonc.2021.790458
Haun MW, Estel S, Rücker G et al (2017) Early palliative care for adults with advanced cancer. Cochrane Database Syst Rev 6:CD011129. https://doi.org/10.1002/14651858.CD011129.pub2
Hickmann A-K, Hechtner M, Nadji-Ohl M et al (2017) Evaluating patients for psychosocial distress and supportive care needs based on health-related quality of life in primary brain tumors: a prospective multicenter analysis of patients with gliomas in an outpatient setting. J Neurooncol 131:135–151. https://doi.org/10.1007/s11060-016-2280-0
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MKF and JK. The first draft of the manuscript was written by MKF and edited by JK. FW and TW prepared tables and provided additional literature research. EG supervised the whole study. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University Leipzig, Medical Faculty (467/16-ck).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fehrenbach, MK., Wilhelmy, F., Wende, T. et al. Perioperative psychological distress in patients with intracranial tumors; a single center study. J Neurooncol (2024). https://doi.org/10.1007/s11060-024-04657-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11060-024-04657-8