Abstract
Parkinson disease (PD) is a neurodegenerative disorder marked by the preferential dysfunction and death of dopaminergic neurons in the substantia nigra. The onset and progression of PD is influenced by a diversity of genetic variants, many of which lack functional characterization. To identify the most high-yield targets for therapeutic intervention, it is important to consider the core cellular compartments and functional pathways upon which the varied forms of pathogenic dysfunction may converge. Here, we review several key PD-linked proteins and pathways, focusing on the mechanisms of their potential convergence in disease pathogenesis. These dysfunctions primarily localize to a subset of subcellular compartments, including mitochondria, lysosomes and synapses. We discuss how these pathogenic mechanisms that originate in different cellular compartments may coordinately lead to cellular dysfunction and neurodegeneration in PD.
Similar content being viewed by others
Introduction
Parkinson disease (PD) is a common neurodegenerative disease that reaches 2–3% prevalence in the population above the age of 65 years1. The pathology of PD first appears in the olfactory nucleus and brainstem and then expands, in stages, to the substantia nigra before further propagating to other parts of the brain2. The preferential death of dopaminergic neurons in these regions, particularly the substantia nigra, results in the diagnostic clinical symptoms of resting tremor, bradykinesia and rigidity3. Various secondary motor symptoms are commonly observed, as are non-motor symptoms such as cognitive impairment, autonomic dysfunction (including anxiety and depression), disordered sleep and anosmia3.
PD is a disorder of diverse genetic aetiology. There are numerous well-established monogenic causes of the disease, and there are probably dozens of genetic variants (including sequence and expression variants) that contribute to sporadic disease risk4,5. This complexity is underscored by the variable penetrance of several PD genes that exhibit Mendelian inheritance patterns and by the observation that sporadic PD is substantially more common than familial PD4,5. Recent meta-analyses of European and multi-ancestry genome-wide association study (GWAS) datasets have identified upwards of 80 risk loci6,7. It is important to note that many of these risk loci are linked to multiple genes, and thus the relationship between specific genes within these loci and PD risk often warrants cautious appraisal. However, the identification of non-causal, risk-associated variants in Mendelian-linked genes (including GBA1, LRRK2, SNCA and VPS13C) in these and other datasets6,7,8 suggests that there may be shared pathogenic mechanisms between monogenic and sporadic PD. In addition to genes, environmental inputs (including exposure to heavy metals or pesticides) are modifiers of disease risk9.
To better understand the cellular pathogenesis of PD and to help to guide the development of therapeutic interventions, it is important to advance our understanding of the cellular functions of the various genes associated with disease risk and to identify the subcellular sites and pathways at which these factors converge to drive disease pathology. In the first part of this Review, we describe the background and physiological functions of several key PD genes and the proteins that they encode (noting that it is not possible to cover all PD-related genes here). We additionally discuss genes with less well-understood involvement in PD but which appear to have functional relationships with these key PD genes. Finally, we describe the current state of research into how these genes might functionally converge on disease pathology, with particular emphasis on interrelated dysfunctions of mitochondria and lysosomes. To focus the scope of this Review, we will only minimally address neuroinflammation10, functions that are non-autonomous to dopaminergic neurons11, or the role of iron and other metals12. However, these mechanisms, which have been covered by other reviews, are all important contributors to PD pathology.
Key Parkinson disease genes
A good starting point to address potential mechanisms of convergent dysfunction in PD is to examine the native function of key PD genes. Here, we discuss a set of PD genes that encode proteins that are involved in cellular pathways and mechanisms associated with PD pathogenesis, and between which there is mounting evidence of functional interaction (Table 1).
α-Synuclein
SNCA encodes the small 140-amino-acid protein α-synuclein. The first causal mutation for PD to be identified was a dominant missense mutation in SNCA that produces an Ala53Thr substitution13. Several additional causal mutations in this gene have since been identified, including triplication of the SNCA locus14. α-Synuclein is the principal component of Lewy bodies (LBs), dense inclusions made up of proteins, lipids and dysfunctional organelles that are a pathological hallmark of PD. The aggregation of α-synuclein that precedes LB formation involves the adoption of a self-templating β-sheet protein structure, largely dependent on misfolding of a short hydrophobic stretch of amino acids that is not conserved in the closely related β- and γ-synucleins15. This misfolded β-sheet structure acts as a template for the conversion of endogenous α-synuclein, first into oligomers and then into larger, insoluble fibrils, and is a critical component of the proposed intercellular propagation of α-synuclein aggregates16. Both pathological mutations in SNCA17 and overexpression of α-synuclein18 are sufficient to enhance the formation of insoluble α-synuclein fibrils and promote the degeneration of dopaminergic neurons in several species, including flies and mice. Ectopic α-synuclein overexpression is even sufficient to produce toxic inclusions in yeast19.
Under physiological conditions, α-synuclein appears to have a role in the function of SNAREs, proteins that mediate the trafficking and fusion of membranous vesicles (including synaptic vesicles, which contain neurotransmitters such as dopamine). At physiological levels, α-synuclein physically binds SNARE proteins and mediates the formation of SNARE complexes20. However, overexpression of wild-type or mutant α-synuclein drives the sequestration of synaptic vesicle SNAREs, with concomitant neuronal dysfunction21. In addition to its synaptic functions22, α-synuclein also appears to have both physiological and pathological functions in the nucleus23.
Within neurons, the levels of α-synuclein are primarily balanced by degradation within lysosomes and, to a lesser extent, by proteasomes24. Within lysosomes, the protease cathepsin D appears to be a key mediator of α-synuclein proteolysis and is itself encoded by a potential PD risk gene25. Inhibition of cathepsin D or knockdown of its encoding gene, CTSD, impairs the degradation of α-synuclein26, whereas its overexpression protects dopaminergic neurons against α-synuclein toxicity in both mice and nematodes27. Cathepsin B is an additional lysosomal protease encoded by a nominated PD risk gene7,28 that has been found to contribute to α-synuclein degradation29. Although α-synuclein can be delivered to lysosomes for degradation through macroautophagy, it has also been reported to be a substrate for lysosomal delivery via client-specific chaperone-mediated autophagy (CMA). Two PD-associated variants of α-synuclein (A53T and A30P) have been proposed to inhibit CMA by non-productively binding (and thus competitively inhibiting) the lysosomal CMA receptor LAMP2 (ref. 30).
A large number of post-translational modifications of α-synuclein have been identified (see ref. 31 for more extensive coverage). Nitrosylated α-synuclein appears extensively within LBs in post-mortem brain tissue from individuals with PD32, and both oxidation and nitrosylation of α-synuclein are sufficient to promote its aggregation in vitro33. Aggregated and LB-associated α-synuclein is heavily phosphorylated at residue S129, a mark that may drive both its insolubility and its aggregation propensity34. Finally, the tyrosine-protein kinase ABL1 has been found to interact with α-synuclein and phosphorylate it at residue Y39, a modification that appears to stabilize α-synuclein and shield it from autophagic degradation35. Both oxidation and Y39-phosphorylation of α-synuclein block its interaction with the chaperones HSPA8 and HSP90AB1, enhancing aggregation36.
PINK1 and parkin
The E3 ubiquitin ligase parkin37 and the kinase PINK1 (ref. 38) are both encoded by genes associated with autosomal-recessive PD. The close genetic interaction of parkin and PINK1 was established in flies, in which loss of either of the genes encoding these proteins produces similar phenotypes (including mitochondrial defects, morphologic and behavioural deficits and loss of dopaminergic neurons), with epistasis experiments showing that parkin acts downstream of PINK1 in a shared pathway39.
The role of PINK1 and parkin in mitophagy is perhaps the most extensively described biological pathway of all PD-related proteins40. Mitophagy is a quality control pathway by which damaged and dysfunctional mitochondria are targeted to the lysosome for degradation. Mitochondrial insults, such as depolarization, mitochondrial protein folding stress or metal toxicity, cause PINK1 (which is normally rapidly degraded41) to be stabilized at the outer mitochondrial membrane (OMM)42. There, it phosphorylates both parkin43 and ubiquitin44, modifications that alleviate an auto-inhibitory conformation of parkin and enforce its association with the mitochondrial membrane.
The ubiquitin ligase activity of parkin results in the extraction of several proteins present in the OMM from the membrane by the protein VCP (also known as p97) and their subsequent proteasomal degradation45. Key parkin substrate proteins include mitofusin-1 (MFN1), MFN246, mitochondrial Rho GTPase 1 (MIRO1) and MIRO2 (ref. 47). The rapid initial degradation of these proteins, which may also involve their phosphorylation by PINK1 (refs. 48,49), promotes the fragmentation (in the case of MFN1 and MFN2) or perinuclear translocation (in the case of MIRO1 and MIRO2) of affected mitochondria, increasing the efficiency of mitochondrial degradation50. The ubiquitination of additional OMM substrates47 promotes the recruitment of autophagic adaptor proteins, which physically link ubiquitinated substrate proteins to the autophagic machinery. One key adaptor in mitophagy is optineurin (OPTN), along with its cofactor, the serine–threonine protein kinase TBK1 (refs. 51,52). Interestingly, parkin also ubiquitinates VCP, several autophagy adaptors and the mitochondria–lysosome contact regulatory proteins TBC1D15 and FIS1 (ref. 53), though the functional consequences of these ubiquitination events are incompletely understood.
Two additional proteins encoded by PD risk genes may be associated with mitophagy. FBXO7, first identified as an autosomal-recessive PD risk gene54, is another E3 ubiquitin ligase. Knockdown of FBXO7 in flies and in the SH-SY5Y neuroblastoma cell line decreased mitophagy, whereas overexpression of FBXO7 rescued morphological and behavioural defects in flies with parkin loss-of-function, but not in flies lacking PINK1. Thus, FBXO7 might act downstream of PINK1 and in parallel with parkin55. Alternatively, it has been proposed that FBXO7 promotes the degradation of PINK1 and that loss of FBXO7 is protective against mitophagy-inducing stress56. Given these disparate findings, it is perhaps unsurprising that other recent work has contested the role of FBXO7 in mitophagy altogether57.
SREBF1 has also been identified as a PD risk gene58. It has been proposed that its protein product, the transcription factor precursor SREBF1, indirectly stabilizes the association of PINK1 with mitochondria in a manner that depends on the ability of SREBF1 to promote cholesterol production59.
PARK7
PARK7, which encodes Parkinson disease protein 7 (PARK7, also known as DJ-1), is a recessive driver of early-onset PD60. Functionally, a key residue of PARK7 is the highly conserved and highly labile C106. In the native protein, C106 is part of a catalytic dyad through which PARK7 detoxifies methylglyoxal by converting it to lactic acid61. Methylglyoxal is a reactive side product of glycolysis and other metabolic pathways that can modify proteins, lipids and nucleic acids, producing cellular challenges that include oxidative stress62. It is also thought that oxidation of C106 serves as a direct sensor of oxidative stress63, promoting switch-like behaviour in PARK7 function. Knockdown of Park7 in mouse neuroblasts increases their susceptibility to oxidative stress and mechanistically related stresses of the endoplasmic reticulum (ER) and proteasome64. However, PARK7 function is most closely related to mitochondrial oxidant stress, and oxidation of C106 results in PARK7 translocation to the OMM65. PARK7 appears to promote the stabilization of the transcription factor NRF2 (ref. 66), a key upstream regulator of mitochondrial function, and loss of PARK7 also increases sensitivity to agents that produce mitochondrial reactive oxygen species (ROS)67. Some studies have suggested that PARK7 may have a role in PINK1 and parkin-mediated mitophagy68,69. It has also been proposed that PARK7 acts as a chaperone that decreases the aggregation of α-synuclein70; alternatively, the detoxification of methylglyoxal by PARK7 may reduce glycation of α-synuclein, which has been reported to enhance its aggregation propensity71.
Much of the body of research around PARK7 lacks substantial replication or complete mechanistic detail. This may be in part owing to the highly pleiotropic nature of PARK7 function, which has been proposed to include redox sensing, chaperone activity, glyoxalase activity, deglycase activity, protease activity, multifunctional regulation of mitochondria and transcriptional co-regulation72. It is also probable that PARK7 dysfunction makes important contributions to PD pathology through cell non-autonomous mechanisms, particularly via astrocytes11, in which glycolysis is elevated and methylglyoxal production is probably enhanced62.
LRRK2
Mutations in LRRK2 that drive autosomal-dominant PD73 cause hyperactivation of the kinase function of LRRK2 (ref. 74). This increases sensitivity to cell death caused by oxidative stress75 or by α-synuclein accumulation76. LRRK2 hyperactivity has been reported in brain tissue from individuals with sporadic PD77 (although this observation has been challenged78), as well as in rat models of PD induced by chemical agents or by α-synuclein overexpression77. It should be noted that LRRK2 is perhaps the PD gene for which there is the most evidence to support cell non-autonomous forms of dysfunction, based on gene expression studies79, as well as experiments in non-neuronal cell types such as astrocytes80 and microglia81.
The key physiological pathways to which LRRK2 contributes are still poorly understood. A small fraction of cellular LRRK2 localizes to endosomes and autophagosomes, and LRRK2 hyperactivation is generally thought to be inhibitory to autophagy82. Additionally, LRRK2 has been variously claimed to have direct and indirect effects on protein expression mediated through both transcription and translation83.
The mechanisms that promote the activation of LRRK2 are better characterized. Translocation of cytosolic LRRK2 to the lysosome membrane is enhanced by PD-associated mutations that increase its kinase activity82, as well as by agents that activate LRRK2 by inducing lysosomal stress, such as LLOMe84 and chloroquine. Interestingly, artificially targeting LRRK2 to various cellular membranes in the absence of stressors, by means of chemically induced heterodimerization, appears sufficient to activate LRRK2 at those compartments85, indicating that its membrane binding and kinase activity are highly coordinated.
Several RAB GTPase proteins (RABs) are key physiological targets of LRRK2, including RAB8A, RAB10, RAB12 and RAB29 (ref. 86), and phosphorylation of these proteins modulates their interactions with upstream regulators and downstream effectors87. However, RAB phosphorylation also drives a feedforward mechanism that promotes additional LRRK2 endolysosomal membrane recruitment induced by activating signals such as lysosomal damage. LRRK2 activation increases the recruitment of RAB8A, RAB10 and RAB12 to endosomes and lysosomes84. In turn, these proteins bind at up to three distinct sites on LRRK2 to cooperatively reinforce its membrane recruitment and activation, and at least one of these sites exclusively binds RABs that have been phosphorylated by LRRK2 (refs. 88,89,90). RAB-mediated recruitment of LRRK2 may constitute a mechanism of lysosomal quality control, and it has been implicated in recruitment of endosomal sorting complexes for transport-III (ESCRT-III) to repair endosome membranes91 and in the regeneration of small, intact vesicles from damaged lysosomes84.
GWASs have also identified an association of PD with several genes encoding LRRK2-accessory proteins. Alterations in the promoter region of RAB29 (also known as RAB7L1) protect against PD risk92. RAB29 has been reported to bind directly to LRRK293 and may mediate recruitment of LRRK2 to the trans-Golgi network94, although it has also been reported that RAB29 is dispensable for the activation of LRRK2 in response to lysosomal stresses95. RAB29 and LRRK2 may additionally complex with the co-chaperone BAG5 and cyclin-G-associated kinase (GAK)96, which are also encoded by genes associated with PD risk58. The role of this complex is not fully clear, though various mechanisms have been suggested related to endosomal network transport and autophagy. Finally, an association between the small GTPase RIT2 and PD has been described97 and it has been found that RIT2 expression is decreased in neurons from individuals with PD linked to mutations in SNCA or LRRK2 (ref. 98). Interestingly, in SH-SY5Y cells with hyperactive LRRK2, overexpression of RIT2 decreased LRRK2 activity and α-synuclein aggregation, suggesting that it is a negative regulator of LRRK2 (ref. 98).
VPS35
Along with VPS29 and VPS26A or VPS26B, VPS35 forms the retromer complex, a key player in endosomal protein sorting and trafficking. The D620N mutation of VPS35, which is generally believed to be dominant negative, causes late-onset PD99,100. This mutation results in impaired maturation of lysosomal hydrolases but does not alter assembly of the retromer complex or the interaction of retromer with cation-independent mannose 6-phosphate receptor (IGF2R, also known as CI-M6PR), a key receptor for lysosomal protein trafficking101. Instead, the D620N mutation may abolish the interaction of retromer with the membrane-transport-associated WASH complex, impairing endosome-to-Golgi retrograde trafficking102 and the initiation of autophagy that is dependent on trafficking of ATG9A to the phagophore103. Although complete knockout of VPS35 produces defects in lysosomal morphologic, functional and proteomic characteristics via the accumulation of missorted endomembrane system proteins104, the effect of the D620N mutation is more subtle, which may underlie conflicting reports about its effect on the sorting of certain membrane proteins, such as GLUT1 (refs. 102,103).
PLA2G6 is an additional gene affected by recessive PD-associated mutations105. This gene encodes a phospholipase that may be functionally connected to VPS35. In flies, PLA2G6 binds VPS35 and enhances retromer complex function, whereas loss of PLA2G6 decreases retromer complex function in a manner that can be rescued by VPS35 overexpression106. PLA2G6 dysfunction has also been linked to elevated ROS and mitochondrial and ER stresses107, though it has not been established how this pathology interacts with the function of VPS35.
GBA1
Glucocerebrosidase (GBA1, also known as GCase), is a lysosomal hydrolase that functions enzymatically to cleave the carbohydrate–lipid link present in both glucosylceramide and gluocosylsphingosine. Homozygous loss of GBA1 drives the autosomal-recessive lysosomal storage disorder Gaucher disease, of which affected individuals often display parkinsonian symptoms108. It is now known that partial loss-of-function of GBA1 is moderately penetrant for the development of PD109, owing to a pathological feedback loop between diminished GBA1 activity and α-synuclein aggregation110, as has been observed across many clinical and genetic models of PD111,112,113,114,115. GBA1 activity is also known to decline with age116, and decreased GBA1 activity has been reported in the brains of individuals with PD that do not carry GBA1 mutations, including those with sporadic PD117.
ATP13A2
ATP13A2 is a P5-ATPase that localizes to endosomes and lysosomes. Mutations in ATP13A2 associated with autosomal-recessive PD have been found to disrupt its trafficking and cause it to be retained in the ER118. Loss-of-function of ATP13A2 has been suggested to hinder autophagic flux via impaired lysosomal function119, as well as to impair the initial formation of exosomes within multivesicular bodies120. ATP13A2 was also reported to function in alleviating the toxicity of various metals, including manganese121 and zinc122. Most recently, it has been demonstrated that ATP13A2 is a polyamine exporter, in the absence of which spermine and spermidine can accumulate in the lysosomal lumen, causing alkalization and membrane rupture123.
Synaptic proteins
Auxilin, synaptojanin-1 and endophilin-A1 are a trio of PD-associated synaptic proteins. Mutations in DNAJC6 (encoding auxilin)124 and SYNJ1 (encoding synaptojanin-1)125,126 have been associated with autosomal-recessive PD, whereas SH3GL2 (encoding endophilin-A1) has been nominated as a risk gene in multiple studies6,7,28. The close functional relationships between these proteins was elucidated well before their association with PD was discovered. During endocytic synaptic vesicle recycling, auxilin and HSPA8 initiate the process of clathrin coat disassembly, which additionally requires the phosphatase activity of synaptojanin-1. Endophilin-A1, in turn, is required for the recruitment of synaptojanin-1 to endocytic vesicles. As such, loss of any of these three proteins results in impaired clathrin uncoating and synaptic vesicle recycling127,128,129. In flies, knockout of DNAJC6 phenocopies several features associated with PD, including age-dependent dopaminergic neuron death and increased sensitivity to both α-synuclein toxicity and paraquat exposure130. Finally, the phosphatase activity of synaptojanin-1 has also been reported to be required for the maturation of autophagosomes within presynaptic terminals131.
VPS13C
Truncation mutants in VPS13C have been identified that cause autosomal-recessive PD, suggesting a loss-of-function mechanism132. Knockdown of VPS13C has been demonstrated to produce mitochondrial morphology defects and to enhance induction of mitophagy in response to mitochondrial depolarization132. Like other members of the VPS13 family133, VPS13C is a bulk lipid transporter at membrane contact sites; however, interestingly, it appears to localize to ER–lysosome contacts, rather than mitochondria-associated contacts134.
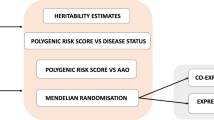
Convergent cellular dysfunction in PD
A question critical to understanding PD is which affected processes are central to the preferential vulnerability of dopaminergic neurons in the substantia nigra and other affected regions. Pinpointing the most relevant subcellular processes is challenging, in part because there are probably multiple distinct pathways that converge on the vulnerability of these neuronal populations, and in part because the various cellular dysfunctions of PD probably reciprocally influence each other. As such, it can be difficult to determine which forms of dysfunction are most directly causal and which may be largely epiphenomenal. Nevertheless, various PD genes do converge on recurring subcellular pathologies, suggesting potential functional nodes that may be central to selective vulnerability (Fig. 1).
a, Under physiological conditions, several Parkinson disease (PD)-related proteins are degraded within the lysosome, including LRRK2 and α-synuclein. Both LRRK2 and α-synuclein have been proposed to be degraded via chaperone-mediated autophagy30,231, whereas α-synuclein can also be degraded by general autophagy24. α-Synuclein degradation may be facilitated by aggregation-preventing chaperone or glyoxalase activity of PARK7 (ref. 70). Other lysosomal functions are homoeostatically maintained, including hydrolysis of glucosylceramide by GBA1 and polyamine export by ATP13A2 (ref. 123). Lysosomal (and overall endomembrane system) proteomic composition is in part maintained through cargo partitioning and sorting processes via endosomes. This involves the actions of VPS35, including its role in recruiting the WASH complex102,103. Parkin-mediated ubiquitination of VPS35 has been proposed to stabilize the association of VPS35 with the WASH complex, which may affect the sorting of several retromer-dependent cargo proteins287. At the mitochondrial inner membrane, reactive oxygen species (ROS) are produced by the electron transport chain. These are sensed by PARK7, allowing for the detection of mitochondrial damage65. If mitochondria accumulate excessive damage, they are cleared by mitophagy, mediated by PINK1 and parkin. Mitophagy involves the decoration of mitochondrial proteins with ubiquitin chains, the recruitment of autophagy adaptors (such as OPTN), and the engulfment of mitochondria into autophagosomes that fuse with lysosomes to degrade the internalized mitochondria40. Potential parallel or upstream contributions of PARK7 to mitophagy have been proposed, perhaps involving recruitment of OPTN or via activation of PTEN212,213,214. b, In PD, pathological mutations and/or exposures to environmental risk factors promote the aggregation of α-synuclein, which impairs membrane and protein trafficking through the endoplasmic reticulum, Golgi and endosomes19,176 (including the trafficking of GBA1 (ref. 110)), exacerbates the unfolded protein response177, and taxes lysosomal proteolysis30,227. Resulting deficiencies in lysosomal GBA1 activity and the accumulation of glucosylceramide within lysosomes further aggravates synuclein oligomerization110. ATP13A2 loss-of-function mutations enhance polyamine accumulation, which can promote lysosomal rupture123. Lysosomal stress and alkalinization or VPS35 deficiencies result in hyperactivation of LRRK2 (ref. 84) (which involves autophosphorylation events). Hyperactive LRRK2 impairs autophagy82, possibly at the point of autophagosome–lysosome fusion80, and may also impair mitophagy through its altered effects on RAB10, MFN1/2 and MIRO1 (refs. 248,250,251,252). A suite of lysosomal and mitochondrial deficiencies converge to impair PINK1 and/or parkin-mediated mitophagy253,254,255,256, the consequences of which are exacerbated by excessive ROS production, including owing to complex I impairment211. Dysfunctional organelles and autophagosomes are caught and accumulate alongside α-synuclein fibrils in Lewy bodies143,146.
α-Synuclein aggregation and Lewy bodies
α-Synuclein aggregation and LB pathology are central to the cellular pathology of PD23. However, whether there is a specific toxic conformer of aggregated α-synuclein has yet to be fully resolved23. Pre-formed α-synuclein fibrils, which mimic an end-state of α-synuclein aggregation, are sufficient to seed the aggregation of native α-synuclein and to reproduce PD-associated neuron-specific functional deficits in mouse primary neurons135. However, mutations in α-synuclein that delay the conversion of soluble oligomeric intermediates into insoluble fibrils result in increased toxicity136. Additionally, some have proposed that the large-scale deposition of α-synuclein fibrils into LBs is a protective process that has an overall effect of decreasing (though probably not eliminating) toxicity137. LB pathology is frequently lacking in certain forms of PD, notably PD associated with mutations in PRKN (encoding parkin)138; conversely, LBs may be observed in brains of asymptomatic individuals without PD mutations139. Although the relative toxicity of LBs compared with that of specific aggregate conformers of α-synuclein remains unresolved, the overall evidence suggests that, at a minimum, the presence of LBs is associated with several cellular dysfunctions139,140.
LBs may contribute to cellular dysfunction via the sequestration of key proteins and organelles. Within LBs, α-synuclein has been shown to interact with and trap tubulin141, the structural constituent of microtubules, which are central to cellular organization and trafficking processes of the cytoskeletal system. α-Synuclein overexpression produces defects in microtubule organization142, which may partly underlie observations of impaired axonal transport in cells with α-synuclein pathology23. Correlative light and electron microscopy experiments show that LBs in the brains of individuals with PD are crowded with dysmorphic membranous organelles, particularly mitochondria, lysosomes and autophagosomes143. This organelle sequestration appears to be dependent on the aggregation of α-synuclein: the degree of mitochondrial association with α-synuclein across diverse brain regions correlates more with the presence of α-synuclein pathology and less with overall α-synuclein expression levels144. Similarly, monomeric α-synuclein does not strongly bind isolated mitochondria in vitro145. In electron microscopy images of brain slices from mice overexpressing human SNCA carrying the A53T mutation, mitochondria present at inclusions are labelled by the autophagy marker LC3-II and often appear partially surrounded by phagophores, indicating abortive or impaired autophagic clearance of LB-associated mitochondria146. Indeed, cross-breeding these mice with Pink1 or Prkn knockout mice exacerbates the accumulation of mitochondria within LBs146. In mice injected with pre-formed α-synuclein fibrils, autophagosomal motility in neurites is also impaired147. Finally, in the brains of people with PD that show LB pathology and in rat models of synucleinopathy driven by an A30P mutation in SNCA, lysosomal proteolysis is diminished148. It will be valuable to more clearly discern whether LBs inflict organelle damage and blunt autophagic response, or whether impaired clearance of damaged cellular structures simply predisposes their incorporation into LBs.
Oxidative stress and oxidized dopamine
Measures of oxidative stress are increased in the post-mortem substantia nigra of people with PD149. Under physiological conditions, ATP generation in neurons occurs primarily through mitochondrial respiration150. This reliance on respiration results in elevated levels of ROS compared with non-neuronal cell types, which may underlie the sensitivity of neurons to additional oxidative stress. Dopaminergic neurons may be particularly sensitive to oxidative stress because dopamine is more readily oxidized than other neurotransmitters, and oxidized dopamine appears to be toxic111. For example, direct injection of dopamine into the rat striatum results in the formation of oxidized dopamine adducts and the specific death of dopaminergic neurons151, and overexpression of human tyrosinase (which converts tyrosine to the dopamine precursor l-DOPA and also oxidizes l-DOPA to dopaquinone) in the rat substantia nigra produces age-dependent dopaminergic neuron loss and motor deficits similar to those seen in PD152. Oxidized dopamine has also been directly observed in the post-mortem brain of individuals with PD, where it is enriched in the substantia nigra153.
Evidence suggests that α-synuclein may be central to the toxicity of oxidized dopamine. Oxidized dopamine has been demonstrated to modify and stabilize α-synuclein protofibrils in vitro154, and the overexpression of α-synuclein in SH-SY5Y cells increases their sensitivity to dopamine overload155. Moreover, in neurons generated from induced pluripotent stem cells (iPSCs) derived from individuals with PD, oxidized dopamine is elevated and α-synuclein solubility is decreased, driving the pathogenic feedback loop between α-synuclein aggregation and loss of GBA1 activity111. Synuclein solubility, lysosomal function and the viability of these cells can be rescued with sustained antioxidant treatment111. Importantly, elevated oxidized dopamine has been observed in iPSC-derived dopaminergic neurons with mutations in PARK7, PINK1, PRKN, LRRK2 and DNAJC6, with corresponding α-synuclein aggregation and GBA1 deficiency invariably observed111,112,113,156.
Dopamine-modified α-synuclein may contribute to other forms of dysfunction beyond GBA1 impairment. α-Synuclein modified by dopamine inhibits CMA in a manner that contributes to dopaminergic neuron death in mice157. The modification of α-synuclein by DOPAL (a metabolite of dopamine) also increases synaptic vesicle leak158, and hypomorphism of VMAT2 (the amine transporter that packages dopamine into synaptic vesicles) in mice results in age-associated oxidative damage and α-synuclein aggregation, with a specific loss of dopaminergic neurons159. Together, these results point to a feedforward mechanism in which oxidized dopamine promotes α-synuclein accumulation and lysosomal dysfunction, driving synaptic defects that result in increased cytosolic dopamine that also becomes oxidized.
Oxidative stress and oxidized dopamine also mediate dysfunction at mitochondria. Dopamine can directly impair mitochondrial respiration in a manner dependent on its oxidation160, and dopamine that is not contained within synaptic vesicles may cause mitochondria-specific ROS production when metabolized by monoamine oxidase (MAO)161. Parkin can be directly modified by ectopically supplied dopamine162 and can be nitrosylated with age or toxic agent exposure163,164. Nitrosylation, which can be a consequence of oxidative stress, inactivates parkin and decreases its solubility. PINK1 can also be inactivated by nitrosylation, including that occurring downstream of α-synuclein overexpression165. Nitrosylation of either PINK1 or parkin has been reported to reduce mitophagy164,165. Modification of PARK7 at residues C53 and C106 by dopamine has also been observed166.
Proteostatic stress
The term proteostasis describes a collection of protein folding and degradation processes that regulate the composition and function of the proteome. The unfolded protein response (UPR) is a transcriptional and translational proteostatic programme centred on the detection of misfolded or unfolded proteins within the ER lumen167. Measures of the UPR are elevated in the brains of people with PD168, and ectopic dopamine also drives the UPR in dopaminergic neuron cultures169. Chemical agents that cause Parkinsonism induce upregulation of the UPR, whereas cells defective for the UPR are more sensitive to these agents170. Some of these agents require de novo protein production to mediate their toxic effects in mouse dopaminergic neuron cultures171, suggesting that proteostatic stress may be a general mechanism underlying neuronal vulnerability. In line with this, reduced protein translation rescues phenotypes associated with PINK1 or parkin deficiency172. Interestingly, PRKN has been found to contain a UPR-responsive promoter and its expression is upregulated in response to ER stress173.
The UPR may also be a key contributor to α-synuclein toxicity. α-Synuclein oligomers are associated with the ER in both the brains of individuals with PD and in mouse models of the disease174, and UPR-inducing stress in the substantia nigra of rats promotes α-synuclein inclusion formation175. Conversely, α-synuclein increases ER stress by impairing ER-to-Golgi (anterograde) vesicle trafficking176, and also directly induces the UPR by binding the unfolded-protein receptor HSPA5 (also known as GRP78/BiP) in the ER lumen177. In rats, knockout of Hspa5 or an age-associated decline in its expression increases α-synuclein toxicity178, whereas overexpressing Hspa5 decreases α-synuclein toxicity in the substantia nigra179. Together, these data indicate that α-synuclein toxicity is increased by proteostatic overload at the ER, to which α-synuclein itself directly contributes.
Synaptic vesicle dysfunction
Auxilin, synaptojanin-1 and endophilin-A1 are all key players in synaptic vesicle recycling, which precedes dopamine packaging. A reduction in the functional synaptic vesicle pool as a result of their dysfunction may increase levels of cytosolic dopamine and thus dopamine-associated toxicity180. Furthermore, because α-synuclein binds to synaptic vesicle membranes and SNARE proteins, overexpression or mutation of α-synuclein produces large tangles of synaptic vesicles that fail to properly recycle or traffic between synaptic boutons in primary mouse neurons181,182. Alternatively, the loss of physiologically functional α-synuclein may impair synaptic vesicle recycling: a triple knockout of α-synucleins, β-synucleins and γ-synucleins in mice phenocopies the effects of loss of endophilin-A1 or synaptojanin-1 in hippocampal neurons, decreasing the ability of the neurons to maintain sustained activity183.
LRRK2 may also have a role at synapses. LRRK2 and its fly homologue LRRK have been found to phosphorylate endophilin-A1 (refs. 184,185). The binding and unbinding of endophilin-A1 to synaptic vesicle membranes is important for synaptic vesicle endocytosis and in flies expressing hyperactive human LRRK2, increased endophilin-A1 phosphorylation reduced its membrane binding and impaired synaptic vesicle endocytosis184. Phosphorylation of endophilin-A1 by LRRK2 may additionally be a signal to initiate localized autophagy at synapses, another process that is sensitive to imbalances in LRRK2 activity186. Hyperactive LRRK2 has also been reported to bind and phosphorylate synaptojanin-1 (ref. 187) and auxilin112, which may contribute to synaptic vesicle recycling defects, although additional replication is needed (Fig. 2).
a, In normal physiology of dopamine neurons, α-synuclein interacts with SNARE proteins to mediate synaptic vesicle organization and to promote membrane fusion during exocytosis of docked synaptic vesicles20. During neuronal activity, calcium-mediated activation of CaMKII stimulates parkin to modify synaptojanin-1, which facilitates its recruitment to synaptic vesicle membranes156. At the endocytic bud neck, the activities of synaptojanin-1 and endophilin-A1 promote scission of the clathrin-coated vesicle127,128,129. The phosphatase activity of synaptojanin-1 also recruits auxilin to the vesicle. Auxilin mediates clathrin coat disassembly, after which the synaptic vesicular amine transporter VMAT2 imports dopamine into the recycled synaptic vesicle. After endocytosis, LRRK2 activity promotes the dissociation of endophilin-A1 from the vesicle membrane184. The released endophilin-A1 may also be ubiquitinated by parkin, but the consequences of this are unclear251. b, In Parkinson disease, pathological aggregation of α-synuclein causes uncontrolled clustering of synaptic vesicles and sequestration of SNARE proteins, which impairs synaptic vesicle exocytosis21. Mutations in the genes encoding auxilin, synaptojanin-1 and endophilin-A1 impair synaptic vesicle recycling and clathrin uncoating127,128,129. This phenotype is recapitulated by hyperactive LRRK2, which phosphorylates and thus inactivates auxilin112 and synaptojanin-1 (ref. 187) in addition to promoting endophilin-A1 dissociation from the vesicle membrane184. VPS35 mutation also results in hyperactivation of LRRK2 by unknown mechanisms238. Depletion of the synaptic vesicle pool results in cytosolic accumulation of readily oxidized dopamine112, which modifies parkin to inactivate it and cause its insoluble aggregation162. Oxidized dopamine also modifies α-synuclein154, increasing its aggregation propensity and exacerbating synaptic vesicle clustering and rupture, which may further increase dopamine leak158.
Interestingly, endocytosis is the most energetically expensive step in synaptic vesicle recycling, specifically requiring ATP derived from mitochondrial respiration. In line with this, synaptic vesicle endocytosis is particularly sensitive to deficiencies in this process188.
Mitochondrial dysfunction
Complex I dysfunction
Our first insights into the cellular mechanisms of PD resulted from the observation of parkinsonian symptoms produced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), an impurity in a synthetic opioid189. The toxic metabolic biproduct of MPTP, MPP+, was found to be an inhibitor of complex I of the electron transport chain (ETC)190, a proton pump that helps to establish the mitochondrial proton gradient (and thus membrane potential). Later, other chemicals identified to be environmental risk factors for PD were also found to produce complex I dysfunction, including rotenone191 and paraquat192. Complex I activity is reduced — to a greater extent than other ETC complexes — in post-mortem brain tissue of individuals with PD, with a particularly high reduction in activity observed in the substantia nigra193. Specific defects in complex I stoichiometry have also been observed in the brains of those with PD194.
Several genetic models of PD also converge on complex I dysfunction, including those with mutations in SNCA195, PINK1 (ref. 196) and GBA1 (ref. 197). Interestingly, in PINK1 or PRKN knockout flies, bypassing complex I by overexpressing the yeast protein Ndi1 (ref. 198) or rescuing complex I by treatment with vitamin K2 (ref. 199) rescues PD-associated defects. More indirectly, VPS35 overexpression protects against MPP+ toxicity in the dopaminergic N27 cell line, with D620N mutant VPS35 being less protective than wild-type VPS35200. This protection may involve the interaction of wild-type VPS35 with the mitochondrial SUMO/Ubiquitin E3 ligase MUL1 in a manner that prevents the degradation of MFN1 and MFN2 and subsequent mitochondrial fragmentation201. Indeed, in VPS35 D620N mutant fibroblasts that display impaired complex I activity, pharmacologic inhibition of mitochondrial fission restored complex I function and respiration202.
Importantly, complex I inhibition with rotenone seems sufficient to induce α-synuclein aggregation and LB formation in rats191. Moreover, a recent mouse model in which complex I activity was directly ablated in dopaminergic neurons displayed a suite of PD-related behavioural and cognitive impairments that were responsive to treatment with l-DOPA203.
General mitochondrial dysfunction
The accumulation of dysfunctional mitochondria in LBs may be preceded by a more direct interference of α-synuclein in mitochondrial function. Monomeric α-synuclein has been observed to be localized to mitochondria in the human substantia nigra195. This localization may depend on a cryptic mitochondria-targeting sequence in α-synuclein and on the direct import of α-synuclein into mitochondria through the translocase of the outer membrane (TOM) complex (with increased import of the PD-associated A53T mutant α-synuclein)195. Mitochondrial damage mediated by excessive or mutant α-synuclein has been proposed to include dysfunction of complex I (ref. 195), production of mitochondrial ROS204, and even physical damage and mitochondrial fragmentation205. The mitochondria-specific lipid cardiolipin may accelerate the oligomerization of α-synuclein, amplifying these adverse effects206. Oligomeric, dopamine-modified or S129E phosphomimetic α-synuclein have also been found to bind TOMM20 (a subunit of the TOM complex) and to impair the import of other mitochondrial proteins, including nuclear-encoded complex I subunits, with TOMM20 overexpression rescuing α-synuclein-associated impairment of respiration207.
LRRK2 hyperactivity promotes mitochondrial fragmentation and ROS production. An interaction of active LRRK2 with the mitochondrial fission protein DRP1 may drive this phenotype208. VPS35 carrying the D620N mutation has also been proposed to induce mitochondrial fragmentation and ROS production in rats via increased DRP1 activity209. Alternatively, increased mitochondrial ROS and decreased respiration in LRRK2 mutant cells may be a consequence of increased expression of ETC uncoupling proteins, which promote oxygen consumption without regeneration of ATP210.
PARK7 deficiency has been found to decrease mitophagy, with corresponding increases in ROS, mitochondrial fragmentation and complex I deficits211. Interestingly, in the M17 neuroblastoma cell line, these deficiencies can be rescued by overexpression of PINK1 or PRKN, whereas PARK7 overexpression can reciprocally rescue PINK1 deficiency68. Thus, it has been proposed that PARK7 and PINK1/parkin may constitute parallel mitochondrial quality control mechanisms, perhaps preventing mitochondrial damage and mediating the response to said damage, respectively. However, a more direct link between these mechanisms is also possible, as PARK7 has been proposed to recruit OPTN to mitochondria during PINK1 and parkin-mediated mitophagy, via a direct interaction that is independent of the status of the oxidation-sensitive C106 residue of PARK7 (ref. 69).
It is also possible that the phosphatase and tumour suppressor PTEN represents a mechanistic link between PARK7 and PINK1/parkin. An extended isoform of this protein, PTENα, was found to coprecipitate with both PINK1 and parkin212. Competing claims have suggested that interaction of PTENα with parkin either enhances mitophagy212, or that that the phosphatase activity of PTENα towards parkin and ubiquitin diminishes mitophagy213. However, removal of the entire Pten locus in mouse dopaminergic neurons protected against toxicity induced by MPTP and 6-OHDA (a dopamine analogue that is selectively toxic to dopaminergic neurons)214. Meanwhile, PARK7 has been reported to nitrosylate PTEN in a manner that decreases PTEN activity and protects cell viability in SH-SY5Y cells215. More extensive experimentation will be required to understand the role of PTEN and/or PTENα in the context of these results.
Finally, it is possible that PINK1 and parkin have cellular functions relevant to PD pathogenesis that are distinct from their role in mitophagy. There is no doubt that physiological mitophagy induced by environmental exposures or stresses helps to prevent PD pathogenesis216. However, PINK1 and parkin are not required for basal mitophagy in mice and flies, including in dopaminergic neurons217. At basal levels, PINK1 is rapidly retrotranslocated and proteasomally degraded after mitochondrial import and initial cleavage218, but it may have some residual activity within mitochondria. NDUFA10 (part of complex I) has been found to harbour a PINK1-dependent phosphosite and, in flies, phosphomimetic NDUFA10 can rescue PINK1 deficiency without rescuing depolarization-mediated recruitment of parkin219. However, the direct phosphorylation of NDUFA10 by PINK1 has not been confirmed219. Other functions of PINK1 and parkin distal to mitochondria have also been proposed (Box 1).
Endolysosomal dysfunction
Effect of α-synuclein
Yeast served as an early model of endomembrane system dysfunction caused by exogenous α-synuclein, which was found to impair vesicular trafficking19, block vesicle fusion220 and sequester RAB proteins220. Importantly, interventions that ameliorated α-synuclein toxicity in yeast were also found to be effective in human iPSC-derived neuron cultures221 and, similarly, overexpression of several different RAB proteins alleviates α-synuclein toxicity in human cells222,223. It is also possible that α-synuclein produces lysosomal dysfunction through interactions with ESCRT-III, a complex with membrane-shaping and scission functions that are relevant to multivesicular body formation and lysosomal repair. A synthetic α-synuclein binding peptide that mimics the ESCRT-III subunit CHMP2B and competitively inhibits the α-synuclein–ESCRT-III association was found to rescue endolysosomal function and promote the degradation of α-synuclein in iPSC-derived dopaminergic neurons224.
α-Synuclein also impairs lysosomal proteolytic activity in several other ways. First, α-synuclein oligomers impair proteasome activity225, which may in turn increase the proteolytic load on lysosomes. Indeed, proteasomal inhibition in rat brain slices results in the specific reduction of dopaminergic neuron viability, with the appearance of LB-like α-synuclein inclusions226. Second, inhibition of CMA by α-synuclein may promote compensatory but reduced-efficiency macroautophagy227. Finally, it has been proposed that RAB protein sequestration mediated by α-synuclein blocks autophagosome formation228. α-Synuclein fibrils cannot be degraded by macroautophagy and have been observed to block the maturation of autophagosomes upstream of their fusion with lysosomes229. More work is needed to establish which of these mechanisms of proteolytic dysfunction is most directly caused by pathologic α-synuclein, and which are concomitant, compensatory or indirect.
Reciprocally, α-synuclein toxicity may be a key end point of lysosomal dysfunction. Activation of autophagy with rapamycin or via ATG7 overexpression protects against α-synuclein aggregation and toxicity in mice230, whereas LRRK2 hyperactivity or overexpression in A53T mutant SNCA transgenic mice increases neurodegeneration, with associated defects in mitochondria and microtubules76. One paper has suggested LRRK2 may itself be a CMA substrate, proposing a potential feedback loop in which overexpression of α-synuclein decreases the degradation of LRRK2 and LRRK2 hyperactivity decreases lysosomal proteolysis of α-synuclein231.
The α-synuclein–GBA1 axis
A key indicator of the relevance of endolysosomal dysfunction in PD is the heavy overrepresentation in individuals with PD of genetic variants associated with lysosomal storage disorders25. The contribution of dysfunctional GBA1 to PD has become even clearer with the elucidation of a functional interaction that may be central to α-synuclein pathology110. It has been found that α-synuclein and GBA1 participate in a pathological feedback mechanism, in which α-synuclein aggregation disrupts GBA1 trafficking to lysosomes and elevation of glucosylceramide (upon loss of lysosomal GBA1 activity) reciprocally seeds additional α-synuclein aggregation110. In both GBA1 mutant and A53T SNCA mouse models, exogenous GBA1 expression, or reduction of glucosylceramide accumulation through inhibition of glucosylceramide synthase, reduces α-synuclein aggregation and ameliorates behavioural defects232,233.
The functional interaction of GBA1 and α-synuclein is well-supported physiologically. In the brains of individuals with sporadic PD, regions with elevated α-synuclein accumulation specifically show diminished GBA1 maturation and activity114. Similarly, in GBA1-deficient mice, accumulation of endogenous α-synuclein is increased in an age-dependent manner115. Finally, pharmacologic rescue of GBA1 activity protects against synucleinopathy in iPSC-derived dopaminergic neurons from individuals with PD, including those with sporadic PD or those carrying mutant forms of ATP13A2 (ref. 234).
The LRRK2–VPS35 axis
It is beginning to appear that LRRK2 and VPS35 represent another axis of convergence in PD pathogenesis. Both proteins have been shown to be involved in membrane trafficking84,102 and autophagy82,103, and PD-associated mutations in the genes encoding these proteins appear to converge at both mitochondrial208,209 and lysosomal dysfunctions113,235. More work is required to mechanistically decipher how these proteins functionally intersect. One study has suggested that wild-type LRRK2 and VPS35 physically associate93, though this finding is controversial. Hyperactive LRRK2 has been found to promote α-synuclein aggregation in mice76, whereas silencing VPS35 or altering its function via introduction of the D620N mutation promotes the accumulation of α-synuclein in human cell cultures and fly models235. Studies of CMA have proposed that LAMP2 dysregulation as a consequence of the LRRK2 G2019S mutation231 or the VPS35 D620N mutation236 may underlie α-synuclein accumulation. However, other studies of the VPS35 D620N mutation in mice have contested that it has any effect on α-synuclein aggregation, including in mice expressing human A53T mutant SNCA237. The VPS35 D620N mutation and the LRRK2 G2019S mutation have also been suggested to phenocopy each other in assays of IGF2R mislocalization and neurite shortening in rats93. Recently, it has been found that the VPS35 D620N mutation increases the kinase activity of LRRK2, whereas VPS35 knockout decreases LRRK2 activity238. Further clarification of the mechanism by which VPS35 affects LRRK2 kinase activity will be key to understanding the ways in which they converge on specific types of dysfunction.
Organelle crosstalk and contacts
Mitochondrial and lysosomal dysfunction feature centrally in PD pathogenesis111. There are several mechanisms by which dysfunction in one organelle may be propagated to or influence the physiological function of the other.
Co-regulation of mitochondrial and lysosomal biogenesis
The transcriptional coactivator PGC-1α (also known as PPARGC1A) is a master regulator of mitochondrial biogenesis239. Loss of PGC-1α sensitizes dopaminergic neurons to oxidative stress240 and to α-synuclein toxicity241, whereas activation of Pgc1a expression is protective against rotenone in mice242. Overexpression of PGC1A also rescues specific defects in the transcription of ETC components and protects against α-synuclein overexpression243. Moreover, PGC1A has been identified as a key gene disrupted by nuclear α-synuclein pathology23.
Similarly, the transcription factor TFEB is the master regulator of lysosome biogenesis, alongside the related TFE3 and MITF244. Activation or overexpression of TFEB protects against α-synuclein toxicity in mice245, presumably by stimulating autophagy. In line with this, activation of autophagy protects against several PD-associated defects, including defects associated with PINK1 or parkin loss-of-function172. In macrophages with a LRRK2 G2019S knock-in mutation, TFE3 activity was decreased in a manner reversed by LRRK2 inhibition81, in line with other data suggesting that LRRK2 activity may oppose autophagy.
Interestingly, PGC-1α and TFEB appear to be co-regulated. TFEB binding sites are found in the promoter of PGC1A and, accordingly, the activation of TFEB upregulates PGC1A expression246. Reciprocally, TFEB is activated after induction of mitophagy (which upregulates PGC1A), in a manner that requires PINK1 and parkin247.
Reciprocal endolysosomal and mitophagic dysfunction
The hyperactivity of LRRK2 that is linked to lysosomal dysfunction also appears to decrease mitophagy downstream or independently of PINK1 and parkin248, with several associated observations that have yet to be fully contextualized. In PINK1 mutant cell culture models, inhibition of LRRK2 protects against cell death induced by mitophagic stress249. Overexpressed LRRK2 has been reported to interact with MFN1, though the physiological relevance to mitophagy is not yet clear250. It has also been suggested that LRRK2 acts in parallel to PINK1 and parkin to promote the degradation of MIRO1 in response to mitochondrial depolarization, with hyperactive LRRK2 losing its ability to bind MIRO1 (ref. 251). Finally, RAB10 has been found to help to recruit OPTN to mitochondria and thus stimulate efficient mitophagy. Phosphorylation of RAB10 by LRRK2 abolishes this function252. Given these multiple competing models, more work is needed to confidently establish how LRRK2 hyperactivity might temper mitophagy, and how direct that mechanism may be.
In keeping with its functional relationship with LRRK2, VPS35 mutations have also been linked to general mitochondrial dysfunction, including a reduction in complex I activity, decreased respiration, and fragmentation200,202. These dysfunctions imply impaired mitochondrial clearance and, indeed, the D620N mutation of VPS35 was recently found to impair depolarization-induced mitophagy upstream of mitochondrial PINK1 accumulation253,254.
Mitophagy and respiration are impaired by loss-of-function of ATP13A2 (ref. 255), and also by loss of GBA1 (ref. 256), which reduces mitochondrial membrane potential and elevates ROS production197. However, a recent report has claimed that GBA1 may also be weakly targeted to the mitochondria, assisting in the energetics and stability of complex I (ref. 257).
VPS13C may also influence aspects of mitochondria–lysosome crosstalk. In early experiments, knockdown of VPS13C was found to decrease basal mitochondrial membrane potential and increase mitochondrial fragmentation, as well as potentiating depolarization-induced mitophagy132. With the discovery that VPS13C is a bulk lipid transporter localized to ER–lysosome contacts134, recent attention has focused on lysosomal defects produced by loss of VPS13C, which include altered lipid composition, morphological defects and trafficking defects258,259. However, mitochondria remain an important figure in VPS13C-related dysfunction, as activation of the inflammatory cyclic GMP–AMP synthase (cGAS)–stimulator of interferon genes (STING) pathway in the absence of VPS13C is driven by increased levels of cytosolic mitochondrial DNA258, though this finding may be more pertinent to mechanisms of cell non-autonomous PD pathogenesis.
Just as lysosomal dysfunction affects mitophagy, perturbations that impair mitophagy have been found sufficient to produce impairments in lysosomal proteolytic capacity260,261. Interestingly, genetic perturbations that produce excessive mitochondrial ROS have also been found to induce lysosomal dysfunction characterized by unresolved autophagolysosomes containing undigested mitochondria260, perhaps implying that oxidative stress can be propagated to lysosomes via mitophagy.
Mitochondria-to-lysosome crosstalk may also be mediated through mitochondrial-derived vesicles (MDVs), small compartments derived from the mitochondria that vary in composition, regulation, and trafficking262. At least three distinct forms of MDVs that traffic to lysosomes have been described across various mammalian cell culture models, including constitutively produced MDVs262,263, MDVs responsive to ROS produced via inhibition of the ETC264, and MDVs that are triggered by inflammation265. Of these, ROS-responsive MDVs require the presence of functional parkin and PINK1 and may represent a small-scale but early quality control mechanism that precedes a more extensive mitophagic response264. By contrast, inflammation-induced MDVs appear to be inhibited by overexpression of parkin or stimulation of mitophagy265. VPS35 appears to be required at least for the function of constitutively produced MDVs209 (including those targeted to peroxisomes rather than lysosomes266), perhaps by promoting DRP1 recruitment to mitochondria for vesicle scission209,263. However, parkin knockout does not appear to affect constitutive MDV formation263. Altogether, the apparent diversity of MDVs warrants greater investigation and suggests that MDVs must not be treated as monolithic when considering the potential roles of VPS35, PINK1 and parkin.
Interorganelle contacts
Interorganelle contacts are regions of close proximity (10–30 nm) between organelles characterized by dedicated tether proteins, distinct proteomic composition, and one or more specific functions267. These contacts are central to a number of neurodegenerative diseases, with many disease proteins reported to mediate contacts, function at contacts or pathologically associate with contacts267. Mitochondria–lysosome contacts may be particularly relevant to PD (Fig. 3). These contacts, which form independently of mitochondria–lysosome associations during mitophagy, regulate mitochondrial division268 and are highly dynamic, with untethering events being mediated by RAB7A hydrolysis upon recruitment of the GTPase-activating protein TBC1D15 to contact sites by FIS1. Interestingly, even though basal mitochondria–lysosome contacts are devoid of autophagosome markers and unaffected by the genetic ablation of autophagy receptors268, TBC1D15, FIS1 and RAB7A may be required for efficient mitophagy, as knockdown of either TBC1D15 or FIS1 impairs autophagosome resolution downstream of PINK1 and parkin269. It has also been reported that RAB7A phosphorylation by TBK1 during mitochondrial depolarization promotes RAB7A-mediated recruitment of FLCN to the mitochondria to stimulate mitophagy270. Furthermore, RAB7A has been reported to facilitate the juxtaposition of ATG9A-containing autophagosomes with mitochondria271, a process that requires RAB7A to be recruited to mitochondria by a heterodimeric guanine nucleotide exchange factor complex downstream of mitochondrial ubiquitin271. The salient differences between the regulation of RAB7A, TBC1D15 and FIS1 in basal mitochondria–lysosome contacts and their regulation in mitophagy-induced contacts have yet to be fully elucidated.
a, In healthy cells, endoplasmic reticulum (ER)–mitochondrial contact sites (ERMCS) are maintained by a cohort of tethering interactions, including those between VAPB and RMDN3 (ref. 267), and homotypic MFN1–MFN1 interactions267. ERMCs are further maintained by the ITPR3–HSPA9–VDAC1–PARK7 complex, which functions in the transfer of calcium from the ER to mitochondria284. During mitophagy, MFN1 that is ubiquitinated by parkin46 is extracted by VCP45, which breaks apart ERMCS. Vesicles that are regenerating from lysosomal membranes may scission at contact sites between the ER and the lysosome in a manner that is dependent on LRRK2 (refs. 84,283), whereas VPS13C mediates bulk lipid transfer between the ER and the lysosome134. Mitochondria–lysosome contacts, which are important for the fission and dynamic positioning of those organelles, are regulated by the TBC1D15-stimulated GTP hydrolysis of RAB7A, with FIS1 recruiting TBC1D15 to contact sites268. Conversely, parkin-mediated ubiquitination of RAB7A stabilizes it at the lysosomal membrane273. b, Parkinson disease (PD)-related mutations can promote disrupted interorganelle contacts, driving either decreased or increased ERMCS and mitochondria–lysosome contacts. Loss of PARK7 disrupts the ITPR3–HSPA9–VDAC1–PARK7 complex and increases calcium retention in the ER284, whereas pathological α-synuclein species can interact with VAPB, breaking its interaction with RMDN3 and also reducing ERMCS285. Alternatively, loss of parkin activity increases MFN1 levels on the mitochondria, increasing ERMCS by increasing MFN1–MFN1 interactions267. α-Synuclein can accumulate at ERMCS, where it produces mitochondrial fragmentation278. Within lysosomes, loss of GBA1 activity decreases the cytosolic pool of TBC1D15 (indicated by an X), which decreases RAB7A GTP hydrolysis and prolongs mitochondria–lysosome contacts272. Alternatively, loss of parkin can reduce the levels of RAB7A at lysosomes, decreasing mitochondria–lysosome contacts274. Various forms of lysosomal stress and damage produced by PD-related mutations cause hyperactivation of LRRK2, increasing the formation of the lysosomal tubules, which undergo scission at ER contact sites84,283. Loss of VPS13C function causes lysosomal swelling and increased mitochondria–lysosome contacts, through unknown mechanisms (indicated by a ?)259.
Several mutations in PD-related genes have been observed to alter mitochondria–lysosome contacts. Loss of GBA1 increases these contacts through reduced expression of TBC1D15 (ref. 272), whereas loss of parkin decreases the contacts as a result of decreased lysosomal recruitment and GTP binding of RAB7A273,274 (Box 1). Interestingly, the relatively broad cellular distribution of RAB7A becomes more completely lysosomal upon loss of VPS35 (ref. 275). Mitochondria–lysosome contacts are also increased in dopaminergic neurons with VPS13C knockdown259, though the underlying mechanism has yet to be identified.
Mitochondria–lysosome contacts may have additional functions beyond organelle dynamics. In neurons, axonal mitochondria–lysosome contacts have been found to facilitate local translation of mitochondrial proteins276. The contacts may also be involved in amino acid homoeostasis. In yeast, loss of amino acid export from the vacuole (functionally equivalent to lysosomes) results in a specific decline in mitochondrial function277. Similarly, mutations in PRKN that decrease mitochondria–lysosome contacts alter the levels of numerous amino acids within mitochondria and lysosomes in a reciprocal manner274.
Contacts between mitochondria and the ER are also relevant to PD pathology. α-Synuclein with A53T or A30P mutation is enriched at ER–mitochondrial contact sites (ERMCS) in M17 cells and the mouse brain, where it promotes mitochondrial fragmentation278. ERMCS may also be increased in flies deficient for PINK1 or parkin owing to stabilization of the Drosophila MFN homologue Marf, and knockdown of Marf in these flies reduces ERMCS and partially rescues PINK1 or parkin-associated morphological defects and dopaminergic neuron loss279. In line with this, VCP-mediated extraction of MFN2 to break ERMCS is a critical step in the initiation of mitophagy280. Autophagosomes are also known to form at ERMCS281. It has recently been suggested that LRRK2 regulates ERMCS under conditions of ER stress282. LRRK2 may bind parkin and other ring-between-ring E3 ligases in a manner that prevents their activation by the kinase PERK during the UPR. Hyperactive LRRK2 loses association with these ligases, leading to their activation by PERK and the dismantling of ERMCS282. Finally, ER–lysosome contacts may feature in PD pathogenesis, as lysosomal tubules, which are induced after the activation of LRRK2 by lysosomal stress or damage84, have been observed to undergo fission at points of ER contact283. It is not clear yet whether LRRK2 and ER contacts are also involved in the scission of lysosomal tubules during physiological events, such as vesicular membrane regeneration from autophagolysosomes after autophagy.
Finally, one key function of ERMCS is the privileged transfer of calcium from the ER to mitochondria. This is mediated by a complex between the ER calcium exporter ITPR3 and the mitochondrial importer VDAC1, which are connected through HSPA9 and PARK7 (ref. 284). Impaired calcium homoeostasis is a frequent feature in cellular models of PD and may be a consequence of impaired ERMCS (Box 2).
Concluding remarks
A deeper understanding of the cellular biology of each gene and corresponding protein implicated in PD would be insufficient for a complete image of PD pathogenesis, because environmental factors, cell non-autonomous mechanisms and systems biology must also be considered. However, every step forward taken in understanding the cellular biology of PD is another step towards development of mechanism-based therapeutic interventions. A key factor in translating this knowledge into potential therapies will be understanding how the diverse influences on the cellular biology of PD converge on specific pathways amenable to therapeutic targeting.
Significant strides have been made in identifying the convergent cellular biology of PD. Several subcellular compartments have been identified at which we observe the clustering of relevant genes and/or pathology, including mitochondria, lysosomes and synapses. Moreover, some recurring functional nodes have been identified, such as accumulation of α-synuclein and toxic dopamine oxidation. As the state of research progresses, we continue to find more ways that PD risk genes connect into these converging nodes.
However, several important challenges remain. First, it will be valuable to identify which points of convergence are directly causal in the pathogenesis of PD. For example, the UPR at the ER features prominently in the cellular biology of PD, but few PD-related genes function principally at the ER. The biological functions that most directly affect the development of PD will represent the most attractive therapeutic targets. Moreover, putative causal mechanisms should explain the preferential vulnerability of dopaminergic neurons, as in the case of oxidized dopamine toxicity. Some of the genes and mechanisms outlined in this Review also participate in cell non-autonomous contributions to PD pathogenesis, and it will be important to elucidate how cell non-autonomous dysfunction links to the death of these neuronal populations.
Second, it will be important to identify whether PD arises through one specific pathway or (more probably) several. Although the preferential loss of dopaminergic neurons clearly underlies the main clinical manifestation of the disease, we have yet to fully define how many distinct mechanisms produce this selective vulnerability. For example, is the mitophagy axis distinct from the LRRK2–VPS35 axis, or is there an important node between them which has yet to be described? Is the accumulation of toxic oxidized dopamine observed in all forms of PD or just a subset? Are there other important pathological networks that remain to be discovered? Of course, the task of identifying central pathogenic mechanisms is complicated by the fact that the pathways and functions detailed here do not tend to fail in isolation, a consequence of the dense functional and homoeostatic interactions by which they influence each other.
Understanding how cellular dysfunction propagates from one compartment to another in PD will help us to dissect out the root causes of pathology. The lines of causality in PD pathogenesis are smudged both by the existence of positive feedback mechanisms (such as those that link α-synuclein and GBA1, or RABs and LRRK2) and by dysfunctions that may currently appear reciprocal owing to insufficient fine-mapping of mechanisms.
Finally, several neurodegenerative diseases display overlapping disease pathways and pathologies such as protein aggregation, lysosomal dysfunction and age-dependent mechanisms. Thus, researching the convergent mechanisms in PD may yield greater insight into the pathogenesis of other neurodegenerative diseases, shape the scientific approaches which are most fruitful to understanding pathologic dysfunction, and refine our understanding of the factors that make for promising therapeutic targets in neurodegeneration.
References
Poewe, W. et al. Parkinson disease. Nat. Rev. Dis. Prim. 3, 17013 (2017).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211 (2003).
Jankovic, J. Parkinson’s disease: clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 79, 368–376 (2008).
Blauwendraat, C., Nalls, M. A. & Singleton, A. B. The genetic architecture of Parkinson’s disease. Lancet Neurol. 19, 170–178 (2020).
Jia, F., Fellner, A. & Kumar, K. R. Monogenic Parkinson’s disease: genotype, phenotype, pathophysiology, and genetic testing. Genes 13, 471 (2022).
Nalls, M. A. et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 18, 1091–1102 (2019).
Kim, J. J. et al. Multi-ancestry genome-wide association meta-analysis of Parkinson’s disease. Nat. Genet. 56, 27–36 (2024).
Rizig, M. et al. Identification of genetic risk loci and causal insights associated with Parkinson’s disease in African and African admixed populations: a genome-wide association study. Lancet Neurol. 22, 1015–1025 (2023).
Ball, N., Teo, W. P., Chandra, S. & Chapman, J. Parkinson’s disease and the environment. Front. Neurol. 10, 218 (2019).
Tansey, M. G. et al. Inflammation and immune dysfunction in Parkinson disease. Nat. Rev. Immunol. 22, 657–673 (2022).
Kam, T. I., Hinkle, J. T., Dawson, T. M. & Dawson, V. L. Microglia and astrocyte dysfunction in Parkinson’s disease. Neurobiol. Dis. 144, 105028 (2020).
Bjorklund, G., Hofer, T., Nurchi, V. M. & Aaseth, J. Iron and other metals in the pathogenesis of Parkinson’s disease: toxic effects and possible detoxification. J. Inorg. Biochem. 199, 110717 (2019).
Polymeropoulos, M. H. et al. Mutation in the alpha-synuclein gene identified in families with Parkinson’s disease. Science 276, 2045–2047 (1997).
Singleton, A. B. et al. alpha-Synuclein locus triplication causes Parkinson’s disease. Science 302, 841 (2003).
Giasson, B. I., Murray, I. V., Trojanowski, J. Q. & Lee, V. M. A hydrophobic stretch of 12 amino acid residues in the middle of alpha-synuclein is essential for filament assembly. J. Biol. Chem. 276, 2380–2386 (2001).
Luk, K. C. et al. Pathological alpha-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science 338, 949–953 (2012).
Conway, K. A., Harper, J. D. & Lansbury, P. T. Accelerated in vitro fibril formation by a mutant alpha-synuclein linked to early-onset Parkinson disease. Nat. Med. 4, 1318–1320 (1998).
Masliah, E. et al. Dopaminergic loss and inclusion body formation in alpha-synuclein mice: implications for neurodegenerative disorders. Science 287, 1265–1269 (2000). This work is, to our knowledge, the first to model overexpression of human α-synuclein in mice, which developed Lewy body-like inclusions, dopaminergic neuron terminal loss and motor deficits.
Outeiro, T. F. & Lindquist, S. Yeast cells provide insight into alpha-synuclein biology and pathobiology. Science 302, 1772–1775 (2003).
Burre, J. et al. Alpha-synuclein promotes SNARE-complex assembly in vivo and in vitro. Science 329, 1663–1667 (2010). This paper provides evidence for a physiological role of α-synuclein in SNARE complex assembly through association with VAMP2.
Nemani, V. M. et al. Increased expression of alpha-synuclein reduces neurotransmitter release by inhibiting synaptic vesicle reclustering after endocytosis. Neuron 65, 66–79 (2010).
Runwal, G. M. & Edwards, R. H. The role of alpha-synuclein in exocytosis. Exp. Neurol. 373, 114668 (2024).
Wong, Y. C. & Krainc, D. α-Synuclein toxicity in neurodegeneration: mechanism and therapeutic strategies. Nat. Med. 23, 1–13 (2017).
Vogiatzi, T., Xilouri, M., Vekrellis, K. & Stefanis, L. Wild type alpha-synuclein is degraded by chaperone-mediated autophagy and macroautophagy in neuronal cells. J. Biol. Chem. 283, 23542–23556 (2008).
Robak, L. A. et al. Excessive burden of lysosomal storage disorder gene variants in Parkinson’s disease. Brain 140, 3191–3203 (2017).
Sevlever, D., Jiang, P. & Yen, S. H. Cathepsin D is the main lysosomal enzyme involved in the degradation of alpha-synuclein and generation of its carboxy-terminally truncated species. Biochemistry 47, 9678–9687 (2008).
Qiao, L. et al. Lysosomal enzyme cathepsin D protects against alpha-synuclein aggregation and toxicity. Mol. Brain 1, 17 (2008).
Chang, D. et al. A meta-analysis of genome-wide association studies identifies 17 new Parkinson’s disease risk loci. Nat. Genet. 49, 1511–1516 (2017).
McGlinchey, R. P. & Lee, J. C. Cysteine cathepsins are essential in lysosomal degradation of alpha-synuclein. Proc. Natl Acad. Sci. USA 112, 9322–9327 (2015).
Cuervo, A. M., Stefanis, L., Fredenburg, R., Lansbury, P. T. & Sulzer, D. Impaired degradation of mutant alpha-synuclein by chaperone-mediated autophagy. Science 305, 1292–1295 (2004).
Manzanza, N. O., Sedlackova, L. & Kalaria, R. N. Alpha-synuclein post-translational modifications: implications for pathogenesis of Lewy body disorders. Front. Aging Neurosci. 13, 690293 (2021).
Giasson, B. I. et al. Oxidative damage linked to neurodegeneration by selective alpha-synuclein nitration in synucleinopathy lesions. Science 290, 985–989 (2000).
Souza, J. M., Giasson, B. I., Chen, Q., Lee, V. M. & Ischiropoulos, H. Dityrosine cross-linking promotes formation of stable alpha-synuclein polymers. Implication of nitrative and oxidative stress in the pathogenesis of neurodegenerative synucleinopathies. J. Biol. Chem. 275, 18344–18349 (2000).
Fujiwara, H. et al. alpha-Synuclein is phosphorylated in synucleinopathy lesions. Nat. Cell Biol. 4, 160–164 (2002).
Mahul-Mellier, A. L. et al. c-Abl phosphorylates alpha-synuclein and regulates its degradation: implication for alpha-synuclein clearance and contribution to the pathogenesis of Parkinson’s disease. Hum. Mol. Genet. 23, 2858–2879 (2014).
Burmann, B. M. et al. Regulation of alpha-synuclein by chaperones in mammalian cells. Nature 577, 127–132 (2020).
Kitada, T. et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature 392, 605–608 (1998).
Valente, E. M. et al. Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science 304, 1158–1160 (2004).
Pickrell, A. M. & Youle, R. J. The roles of PINK1, parkin, and mitochondrial fidelity in Parkinson’s disease. Neuron 85, 257–273 (2015).
Li, J. et al. PINK1/parkin-mediated mitophagy in neurodegenerative diseases. Ageing Res. Rev. 84, 101817 (2023).
Meissner, C., Lorenz, H., Weihofen, A., Selkoe, D. J. & Lemberg, M. K. The mitochondrial intramembrane protease PARL cleaves human Pink1 to regulate Pink1 trafficking. J. Neurochem. 117, 856–867 (2011).
Narendra, D. P. et al. PINK1 is selectively stabilized on impaired mitochondria to activate Parkin. PLoS Biol. 8, e1000298 (2010). This key early paper in the mitophagy field establishes that mitochondrial depolarization impairs the proteolytic processing of PINK1, resulting in its stable association with the outer mitochondrial membrane and the recruitment of parkin in a manner dependent on its kinase activity.
Kondapalli, C. et al. PINK1 is activated by mitochondrial membrane potential depolarization and stimulates parkin E3 ligase activity by phosphorylating serine 65. Open Biol. 2, 120080 (2012). This paper demonstrates that PINK1 phosphorylation of parkin is a critical modification for the activation of parkin ubiquitin ligase activity in the early stages of mitophagy.
Koyano, F. et al. Ubiquitin is phosphorylated by PINK1 to activate parkin. Nature 510, 162–166 (2014). In this paper, the authors found that ubiquitin phosphorylation by PINK1 facilitates the alleviation of parkin autoinhibition, rounding out our understanding of the broad mechanistic details of PINK1/parkin-mediated initiation of mitophagy.
Kim, N. C. et al. VCP is essential for mitochondrial quality control by PINK1/parkin and this function is impaired by VCP mutations. Neuron 78, 65–80 (2013).
Ziviani, E., Tao, R. N. & Whitworth, A. J. Drosophila parkin requires PINK1 for mitochondrial translocation and ubiquitinates mitofusin. Proc. Natl Acad. Sci. USA 107, 5018–5023 (2010).
Chan, N. C. et al. Broad activation of the ubiquitin-proteasome system by parkin is critical for mitophagy. Hum. Mol. Genet. 20, 1726–1737 (2011).
Chen, Y. & Dorn, G. W. II PINK1-phosphorylated mitofusin 2 is a parkin receptor for culling damaged mitochondria. Science 340, 471–475 (2013).
Wang, X. et al. PINK1 and parkin target Miro for phosphorylation and degradation to arrest mitochondrial motility. Cell 147, 893–906 (2011).
Twig, G., Hyde, B. & Shirihai, O. S. Mitochondrial fusion, fission and autophagy as a quality control axis: the bioenergetic view. Biochim. Biophys. Acta 1777, 1092–1097 (2008).
Wong, Y. C. & Holzbaur, E. L. Optineurin is an autophagy receptor for damaged mitochondria in parkin-mediated mitophagy that is disrupted by an ALS-linked mutation. Proc. Natl Acad. Sci. USA 111, E4439–E4448 (2014).
Lazarou, M. et al. The ubiquitin kinase PINK1 recruits autophagy receptors to induce mitophagy. Nature 524, 309–314 (2015).
Sarraf, S. A. et al. Landscape of the PARKIN-dependent ubiquitylome in response to mitochondrial depolarization. Nature 496, 372–376 (2013). Various proteomic experiments conducted in this paper provide a large dataset of parkin-dependent ubiquitylation sites across the human proteome.
Di Fonzo, A. et al. FBXO7 mutations cause autosomal recessive, early-onset parkinsonian-pyramidal syndrome. Neurology 72, 240–245 (2009).
Burchell, V. S. et al. The Parkinson’s disease-linked proteins Fbxo7 and parkin interact to mediate mitophagy. Nat. Neurosci. 16, 1257–1265 (2013).
Liu, Y. et al. Chemical inhibition of FBXO7 reduces inflammation and confers neuroprotection by stabilizing the mitochondrial kinase PINK1. JCI Insight 5, e131834 (2020).
Kraus, F. et al. PARK15/FBXO7 is dispensable for PINK1/parkin mitophagy in iNeurons and HeLa cell systems. EMBO Rep. 24, e56399 (2023).
Do, C. B. et al. Web-based genome-wide association study identifies two novel loci and a substantial genetic component for Parkinson’s disease. PLoS Genet. 7, e1002141 (2011).
Ivatt, R. M. et al. Genome-wide RNAi screen identifies the Parkinson disease GWAS risk locus SREBF1 as a regulator of mitophagy. Proc. Natl Acad. Sci. USA 111, 8494–8499 (2014).
Bonifati, V. et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science 299, 256–259 (2003).
Lee, J. Y. et al. Human DJ-1 and its homologs are novel glyoxalases. Hum. Mol. Genet. 21, 3215–3225 (2012).
Allaman, I., Belanger, M. & Magistretti, P. J. Methylglyoxal, the dark side of glycolysis. Front. Neurosci. 9, 23 (2015).
Wilson, M. A., Collins, J. L., Hod, Y., Ringe, D. & Petsko, G. A. The 1.1-A resolution crystal structure of DJ-1, the protein mutated in autosomal recessive early onset Parkinson’s disease. Proc. Natl Acad. Sci. USA 100, 9256–9261 (2003).
Yokota, T. et al. Down regulation of DJ-1 enhances cell death by oxidative stress, ER stress, and proteasome inhibition. Biochem. Biophys. Res. Commun. 312, 1342–1348 (2003).
Canet-Aviles, R. M. et al. The Parkinson’s disease protein DJ-1 is neuroprotective due to cysteine-sulfinic acid-driven mitochondrial localization. Proc. Natl Acad. Sci. USA 101, 9103–9108 (2004). This early paper on the characterization of the role of PARK7 in PD demonstrates that PD-associated chemical insults promote the relocalization of PARK7 to the outer mitochondrial membrane in a manner dependent on the ability of residue C106 to be oxidized.
Clements, C. M., McNally, R. S., Conti, B. J., Mak, T. W. & Ting, J. P. DJ-1, a cancer- and Parkinson’s disease-associated protein, stabilizes the antioxidant transcriptional master regulator Nrf2. Proc. Natl Acad. Sci. USA 103, 15091–15096 (2006).
Kim, R. H. et al. Hypersensitivity of DJ-1-deficient mice to 1-methyl-4-phenyl-1,2,3,6-tetrahydropyrindine (MPTP) and oxidative stress. Proc. Natl Acad. Sci. USA 102, 5215–5220 (2005).
Thomas, K. J. et al. DJ-1 acts in parallel to the PINK1/parkin pathway to control mitochondrial function and autophagy. Hum. Mol. Genet. 20, 40–50 (2011). To our knowledge, this is the first paper to suggest a relationship between PARK7 and PINK1/parkin mitophagy, proposing parallel contributions to mitochondrial health based on reciprocal rescue of PINK1 or PARK7 loss by overexpression of the other in a dopaminergic neuroblastoma cell line.
Imberechts, D. et al. DJ-1 is an essential downstream mediator in PINK1/parkin-dependent mitophagy. Brain 145, 4368–4384 (2022).
Shendelman, S., Jonason, A., Martinat, C., Leete, T. & Abeliovich, A. DJ-1 is a redox-dependent molecular chaperone that inhibits alpha-synuclein aggregate formation. PLoS Biol. 2, e362 (2004).
Konig, A., Vicente Miranda, H. & Outeiro, T. F. Alpha-synuclein glycation and the action of anti-diabetic agents in Parkinson’s disease. J. Parkinsons Dis. 8, 33–43 (2018).
Mencke, P. et al. The role of DJ-1 in cellular metabolism and pathophysiological implications for Parkinson’s disease. Cells 10, 347 (2021).
Zimprich, A. et al. Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron 44, 601–607 (2004).
Smith, W. W. et al. Kinase activity of mutant LRRK2 mediates neuronal toxicity. Nat. Neurosci. 9, 1231–1233 (2006). This paper establishes LRRK2 kinase hyperactivation as a key source of neuronal toxicity produced by PD-linked LRRK2 mutations.
West, A. B. et al. Parkinson’s disease-associated mutations in LRRK2 link enhanced GTP-binding and kinase activities to neuronal toxicity. Hum. Mol. Genet. 16, 223–232 (2007).
Lin, X. et al. Leucine-rich repeat kinase 2 regulates the progression of neuropathology induced by Parkinson’s-disease-related mutant alpha-synuclein. Neuron 64, 807–827 (2009).
Di Maio, R. et al. LRRK2 activation in idiopathic Parkinson’s disease. Sci. Transl. Med. 10, eaar5429 (2018).
Fernandez, B. et al. Evaluation of current methods to detect cellular leucine-rich repeat kinase 2 (LRRK2) kinase activity. J. Parkinsons Dis. 12, 1423–1447 (2022).
Moehle, M. S. et al. LRRK2 inhibition attenuates microglial inflammatory responses. J. Neurosci. 32, 1602–1611 (2012).
di Domenico, A. et al. Patient-specific iPSC-derived astrocytes contribute to non-cell-autonomous neurodegeneration in Parkinson’s disease. Stem Cell Rep. 12, 213–229 (2019).
Yadavalli, N. & Ferguson, S. M. LRRK2 suppresses lysosome degradative activity in macrophages and microglia through MiT-TFE transcription factor inhibition. Proc. Natl Acad. Sci. USA 120, e2303789120 (2023).
Alegre-Abarrategui, J. et al. LRRK2 regulates autophagic activity and localizes to specific membrane microdomains in a novel human genomic reporter cellular model. Hum. Mol. Genet. 18, 4022–4034 (2009). The finding of this paper — that LRRK2 can localize to autophagic vesicles to negatively regulate autophagy — has shaped a significant amount of the research related to the role of LRRK2 in PD.
Berwick, D. C., Heaton, G. R., Azeggagh, S. & Harvey, K. LRRK2 biology from structure to dysfunction: research progresses, but the themes remain the same. Mol. Neurodegener. 14, 49 (2019).
Bonet-Ponce, L. et al. LRRK2 mediates tubulation and vesicle sorting from lysosomes. Sci. Adv. 6, eabb2454 (2020).
Kluss, J. H., Bonet-Ponce, L., Lewis, P. A. & Cookson, M. R. Directing LRRK2 to membranes of the endolysosomal pathway triggers RAB phosphorylation and JIP4 recruitment. Neurobiol. Dis. 170, 105769 (2022).
Steger, M. et al. Phosphoproteomics reveals that Parkinson’s disease kinase LRRK2 regulates a subset of Rab GTPases. eLife 5, e12813 (2016). The phosphoproteomic dataset of LRRK2 substrates produced in this work identifies several RAB proteins as key targets.
Steger, M. et al. Systematic proteomic analysis of LRRK2-mediated Rab GTPase phosphorylation establishes a connection to ciliogenesis. eLife 6, e31012 (2017).
Vides, E. G. et al. A feed-forward pathway drives LRRK2 kinase membrane recruitment and activation. eLife 11, e79771 (2022).
Dhekne, H. S. et al. Genome-wide screen reveals Rab12 GTPase as a critical activator of Parkinson’s disease-linked LRRK2 kinase. eLife 12, e87098 (2023).
Wang, X. et al. Rab12 is a regulator of LRRK2 and its activation by damaged lysosomes. eLife 12, e87255 (2023).
Herbst, S. et al. LRRK2 activation controls the repair of damaged endomembranes in macrophages. EMBO J. 39, e104494 (2020). This recent work provides mechanistic evidence for a physiological role of LRRK2 in membrane repair processes initiated upon lysosomal damage.
Gan-Or, Z. et al. Association of sequence alterations in the putative promoter of RAB7L1 with a reduced Parkinson disease risk. Arch. Neurol. 69, 105–110 (2012).
MacLeod, D. A. et al. RAB7L1 interacts with LRRK2 to modify intraneuronal protein sorting and Parkinson’s disease risk. Neuron 77, 425–439 (2013).
Purlyte, E. et al. Rab29 activation of the Parkinson’s disease-associated LRRK2 kinase. EMBO J. 37, 1–18 (2018).
Kalogeropulou, A. F. et al. Endogenous Rab29 does not impact basal or stimulated LRRK2 pathway activity. Biochem. J. 477, 4397–4423 (2020).
Beilina, A. et al. Unbiased screen for interactors of leucine-rich repeat kinase 2 supports a common pathway for sporadic and familial Parkinson disease. Proc. Natl Acad. Sci. USA 111, 2626–2631 (2014).
Pankratz, N. et al. Meta-analysis of Parkinson’s disease: identification of a novel locus, RIT2. Ann. Neurol. 71, 370–384 (2012).
Obergasteiger, J. et al. The small GTPase Rit2 modulates LRRK2 kinase activity, is required for lysosomal function and protects against alpha-synuclein neuropathology. NPJ Parkinsons Dis. 9, 44 (2023).
Vilarino-Guell, C. et al. VPS35 mutations in Parkinson disease. Am. J. Hum. Genet. 89, 162–167 (2011).
Zimprich, A. et al. A mutation in VPS35, encoding a subunit of the retromer complex, causes late-onset Parkinson disease. Am. J. Hum. Genet. 89, 168–175 (2011).
Follett, J. et al. The Vps35 D620N mutation linked to Parkinson’s disease disrupts the cargo sorting function of retromer. Traffic 15, 230–244 (2014).
McGough, I. J. et al. Retromer binding to FAM21 and the WASH complex is perturbed by the Parkinson disease-linked VPS35(D620N) mutation. Curr. Biol. 24, 1678 (2014).
Zavodszky, E. et al. Mutation in VPS35 associated with Parkinson’s disease impairs WASH complex association and inhibits autophagy. Nat. Commun. 5, 3828 (2014). Although the pathological role of the VPS35 mutation in PD is still being clarified, the finding described in this paper — that the D620N mutation impairs the association of the retromer complex with the WASH complex — offers a potential direction for more mechanistic insight.
Daly, J. L. et al. Multi-omic approach characterises the neuroprotective role of retromer in regulating lysosomal health. Nat. Commun. 14, 3086 (2023). The multi-omic dataset produced in this paper shows severe changes to the composition of lysosomes upon knockout of VPS35, bolstering the associations being made between VPS35 and lysosomal function.
Paisan-Ruiz, C. et al. Characterization of PLA2G6 as a locus for dystonia-parkinsonism. Ann. Neurol. 65, 19–23 (2009).
Lin, G. et al. Phospholipase PLA2G6, a Parkinsonism-associated gene, affects Vps26 and Vps35, retromer function, and ceramide levels, similar to alpha-synuclein gain. Cell Metab. 28, 605–618.e6 (2018).
Chiu, C. C. et al. PARK14 (D331Y) PLA2G6 causes early-onset degeneration of substantia nigra dopaminergic neurons by inducing mitochondrial dysfunction, ER stress, mitophagy impairment and transcriptional dysregulation in a knockin mouse model. Mol. Neurobiol. 56, 3835–3853 (2019).
Tayebi, N. et al. Gaucher disease with parkinsonian manifestations: does glucocerebrosidase deficiency contribute to a vulnerability to parkinsonism? Mol. Genet. Metab. 79, 104–109 (2003).
Sidransky, E. et al. Multicenter analysis of glucocerebrosidase mutations in Parkinson’s disease. N. Engl. J. Med. 361, 1651–1661 (2009).
Mazzulli, J. R. et al. Gaucher disease glucocerebrosidase and alpha-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell 146, 37–52 (2011). This paper identifies a pathogenic feedforward mechanism between α-synuclein accumulation and the impaired trafficking and lysosomal activity of GBA1, offering a potential key point of convergent dysfunction in the pathogenesis of PD.
Burbulla, L. F. et al. Dopamine oxidation mediates mitochondrial and lysosomal dysfunction in Parkinson’s disease. Science 357, 1255–1261 (2017). The experiments in this work identify the production of oxidized dopamine in iPSC-derived dopaminergic neurons across a variety of genetic PD models as a key pathologic event influencing the accumulation of insoluble α-synuclein.
Nguyen, M. & Krainc, D. LRRK2 phosphorylation of auxilin mediates synaptic defects in dopaminergic neurons from patients with Parkinson’s disease. Proc. Natl Acad. Sci. USA 115, 5576–5581 (2018).
Ysselstein, D. et al. LRRK2 kinase activity regulates lysosomal glucocerebrosidase in neurons derived from Parkinson’s disease patients. Nat. Commun. 10, 5570 (2019).
Murphy, K. E. et al. Reduced glucocerebrosidase is associated with increased alpha-synuclein in sporadic Parkinson’s disease. Brain 137, 834–848 (2014).
Taguchi, Y. V. et al. Glucosylsphingosine promotes alpha-synuclein pathology in mutant GBA-associated Parkinson’s disease. J. Neurosci. 37, 9617–9631 (2017).
Rocha, E. M. et al. Progressive decline of glucocerebrosidase in aging and Parkinson’s disease. Ann. Clin. Transl. Neurol. 2, 433–438 (2015).
Gegg, M. E. et al. Glucocerebrosidase deficiency in substantia nigra of Parkinson disease brains. Ann. Neurol. 72, 455–463 (2012).
Ramirez, A. et al. Hereditary parkinsonism with dementia is caused by mutations in ATP13A2, encoding a lysosomal type 5 P-type ATPase. Nat. Genet. 38, 1184–1191 (2006).
Dehay, B. et al. Loss of P-type ATPase ATP13A2/PARK9 function induces general lysosomal deficiency and leads to Parkinson disease neurodegeneration. Proc. Natl Acad. Sci. USA 109, 9611–9616 (2012).
Tsunemi, T., Hamada, K. & Krainc, D. ATP13A2/PARK9 regulates secretion of exosomes and alpha-synuclein. J. Neurosci. 34, 15281–15287 (2014).
Gitler, A. D. et al. Alpha-synuclein is part of a diverse and highly conserved interaction network that includes PARK9 and manganese toxicity. Nat. Genet. 41, 308–315 (2009).
Tsunemi, T. & Krainc, D. Zn2+ dyshomeostasis caused by loss of ATP13A2/PARK9 leads to lysosomal dysfunction and alpha-synuclein accumulation. Hum. Mol. Genet. 23, 2791–2801 (2014).
van Veen, S. et al. ATP13A2 deficiency disrupts lysosomal polyamine export. Nature 578, 419–424 (2020).
Edvardson, S. et al. A deleterious mutation in DNAJC6 encoding the neuronal-specific clathrin-uncoating co-chaperone auxilin, is associated with juvenile parkinsonism. PLoS ONE 7, e36458 (2012).
Krebs, C. E. et al. The Sac1 domain of SYNJ1 identified mutated in a family with early-onset progressive parkinsonism with generalized seizures. Hum. Mutat. 34, 1200–1207 (2013).
Quadri, M. et al. Mutation in the SYNJ1 gene associated with autosomal recessive, early-onset parkinsonism. Hum. Mutat. 34, 1208–1215 (2013).
Schuske, K. R. et al. Endophilin is required for synaptic vesicle endocytosis by localizing synaptojanin. Neuron 40, 749–762 (2003).
Verstreken, P. et al. Synaptojanin is recruited by endophilin to promote synaptic vesicle uncoating. Neuron 40, 733–748 (2003).
Yim, Y. I. et al. Endocytosis and clathrin-uncoating defects at synapses of auxilin knockout mice. Proc. Natl Acad. Sci. USA 107, 4412–4417 (2010).
Song, L. et al. Auxilin underlies progressive locomotor deficits and dopaminergic neuron loss in a Drosophila model of Parkinson’s disease. Cell Rep. 18, 1132–1143 (2017).
Vanhauwaert, R. et al. The SAC1 domain in synaptojanin is required for autophagosome maturation at presynaptic terminals. EMBO J. 36, 1392–1411 (2017).
Lesage, S. et al. Loss of VPS13C function in autosomal-recessive parkinsonism causes mitochondrial dysfunction and increases PINK1/parkin-dependent mitophagy. Am. J. Hum. Genet. 98, 500–513 (2016).
Dziurdzik, S. K. & Conibear, E. The Vps13 family of lipid transporters and its role at membrane contact sites. Int. J. Mol. Sci. 22, 2905 (2021).
Kumar, N. et al. VPS13A and VPS13C are lipid transport proteins differentially localized at ER contact sites. J. Cell Biol. 217, 3625–3639 (2018).
Volpicelli-Daley, L. A. et al. Exogenous alpha-synuclein fibrils induce Lewy body pathology leading to synaptic dysfunction and neuron death. Neuron 72, 57–71 (2011).
Winner, B. et al. In vivo demonstration that alpha-synuclein oligomers are toxic. Proc. Natl Acad. Sci. USA 108, 4194–4199 (2011).
Chartier, S. & Duyckaerts, C. Is Lewy pathology in the human nervous system chiefly an indicator of neuronal protection or of toxicity? Cell Tissue Res. 373, 149–160 (2018).
Schneider, S. A. & Alcalay, R. N. Neuropathology of genetic synucleinopathies with parkinsonism: review of the literature. Mov. Disord. 32, 1504–1523 (2017).
Koeglsperger, T. et al. Neuropathology of incidental Lewy body & prodromal Parkinson’s disease. Mol. Neurodegener. 18, 32 (2023).
Poulopoulos, M., Levy, O. A. & Alcalay, R. N. The neuropathology of genetic Parkinson’s disease. Mov. Disord. 27, 831–842 (2012).
Alim, M. A. et al. Tubulin seeds alpha-synuclein fibril formation. J. Biol. Chem. 277, 2112–2117 (2002).
Lee, H. J., Khoshaghideh, F., Lee, S. & Lee, S. J. Impairment of microtubule-dependent trafficking by overexpression of alpha-synuclein. Eur. J. Neurosci. 24, 3153–3162 (2006).
Shahmoradian, S. H. et al. Lewy pathology in Parkinson’s disease consists of crowded organelles and lipid membranes. Nat. Neurosci. 22, 1099–1109 (2019). In this work, correlative light and electron microscopy of Lewy pathology in tissue samples from individuals with advanced cases of PD demonstrates the dense sequestration of membranous cellular content, including specific enrichment of mitochondria, lysosomes and autophagosomes.
Liu, G. et al. alpha-Synuclein is differentially expressed in mitochondria from different rat brain regions and dose-dependently down-regulates complex I activity. Neurosci. Lett. 454, 187–192 (2009).
Wang, X. et al. Pathogenic alpha-synuclein aggregates preferentially bind to mitochondria and affect cellular respiration. Acta Neuropathol. Commun. 7, 41 (2019).
Chen, L., Xie, Z., Turkson, S. & Zhuang, X. A53T human alpha-synuclein overexpression in transgenic mice induces pervasive mitochondria macroautophagy defects preceding dopamine neuron degeneration. J. Neurosci. 35, 890–905 (2015).
Volpicelli-Daley, L. A. et al. Formation of alpha-synuclein Lewy neurite-like aggregates in axons impedes the transport of distinct endosomes. Mol. Biol. Cell 25, 4010–4023 (2014).
Chu, Y., Dodiya, H., Aebischer, P., Olanow, C. W. & Kordower, J. H. Alterations in lysosomal and proteasomal markers in Parkinson’s disease: relationship to alpha-synuclein inclusions. Neurobiol. Dis. 35, 385–398 (2009).
Dexter, D. T. et al. Basal lipid peroxidation in substantia nigra is increased in Parkinson’s disease. J. Neurochem. 52, 381–389 (1989).
Herrero-Mendez, A. et al. The bioenergetic and antioxidant status of neurons is controlled by continuous degradation of a key glycolytic enzyme by APC/C-Cdh1. Nat. Cell Biol. 11, 747–752 (2009).
Hastings, T. G., Lewis, D. A. & Zigmond, M. J. Role of oxidation in the neurotoxic effects of intrastriatal dopamine injections. Proc. Natl Acad. Sci. USA 93, 1956–1961 (1996).
Carballo-Carbajal, I. et al. Brain tyrosinase overexpression implicates age-dependent neuromelanin production in Parkinson’s disease pathogenesis. Nat. Commun. 10, 973 (2019).
Spencer, J. P. et al. Conjugates of catecholamines with cysteine and GSH in Parkinson’s disease: possible mechanisms of formation involving reactive oxygen species. J. Neurochem. 71, 2112–2122 (1998).
Conway, K. A., Rochet, J. C., Bieganski, R. M. & Lansbury, P. T. Jr. Kinetic stabilization of the alpha-synuclein protofibril by a dopamine-alpha-synuclein adduct. Science 294, 1346–1349 (2001).
Junn, E. & Mouradian, M. M. Human alpha-synuclein over-expression increases intracellular reactive oxygen species levels and susceptibility to dopamine. Neurosci. Lett. 320, 146–150 (2002).
Song, P. et al. Parkinson’s disease-linked parkin mutation disrupts recycling of synaptic vesicles in human dopaminergic neurons. Neuron 111, 3775–3788.e7 (2023).
Martinez-Vicente, M. et al. Dopamine-modified alpha-synuclein blocks chaperone-mediated autophagy. J. Clin. Invest. 118, 777–788 (2008).
Plotegher, N. et al. DOPAL derived alpha-synuclein oligomers impair synaptic vesicles physiological function. Sci. Rep. 7, 40699 (2017). This work supports the connection between oxidized dopamine and α-synuclein pathology with the finding that α-synuclein modified by oxidized dopamine has increased oligomerization tendency and may increase synaptic vesicle leakage.
Caudle, W. M. et al. Reduced vesicular storage of dopamine causes progressive nigrostriatal neurodegeneration. J. Neurosci. 27, 8138–8148 (2007).
Berman, S. B. & Hastings, T. G. Dopamine oxidation alters mitochondrial respiration and induces permeability transition in brain mitochondria: implications for Parkinson’s disease. J. Neurochem. 73, 1127–1137 (1999).
Graves, S. M. et al. Dopamine metabolism by a monoamine oxidase mitochondrial shuttle activates the electron transport chain. Nat. Neurosci. 23, 15–20 (2020). This paper establishes a potential connection between oxidized dopamine and mitochondrial dysfunction, finding that cytosolic dopamine oxidized by mitochondrial monoamine oxidase increases electron transport chain activity, resulting in increased generation of mitochondrial ROS.
LaVoie, M. J., Ostaszewski, B. L., Weihofen, A., Schlossmacher, M. G. & Selkoe, D. J. Dopamine covalently modifies and functionally inactivates parkin. Nat. Med. 11, 1214–1221 (2005).
Chung, K. K. et al. S-Nitrosylation of parkin regulates ubiquitination and compromises parkin’s protective function. Science 304, 1328–1331 (2004).
Rizza, S. et al. S-Nitrosylation drives cell senescence and aging in mammals by controlling mitochondrial dynamics and mitophagy. Proc. Natl Acad. Sci. USA 115, E3388–E3397 (2018).
Oh, C. K. et al. S-Nitrosylation of PINK1 attenuates PINK1/parkin-dependent mitophagy in hiPSC-based Parkinson’s disease models. Cell Rep. 21, 2171–2182 (2017).
Girotto, S. et al. Dopamine-derived quinones affect the structure of the redox sensor DJ-1 through modifications at Cys-106 and Cys-53. J. Biol. Chem. 287, 18738–18749 (2012).
Hetz, C., Zhang, K. & Kaufman, R. J. Mechanisms, regulation and functions of the unfolded protein response. Nat. Rev. Mol. Cell Biol. 21, 421–438 (2020).
Hoozemans, J. J. et al. Activation of the unfolded protein response in Parkinson’s disease. Biochem. Biophys. Res. Commun. 354, 707–711 (2007).
Dukes, A. A., Van Laar, V. S., Cascio, M. & Hastings, T. G. Changes in endoplasmic reticulum stress proteins and aldolase A in cells exposed to dopamine. J. Neurochem. 106, 333–346 (2008).
Ryu, E. J. et al. Endoplasmic reticulum stress and the unfolded protein response in cellular models of Parkinson’s disease. J. Neurosci. 22, 10690–10698 (2002). This early and influential paper demonstrates that chemical agents associated with PD induce the UPR and, reciprocally, that impairment of the UPR sensitizes neurons to these chemical agents.
Holtz, W. A. & O’Malley, K. L. Parkinsonian mimetics induce aspects of unfolded protein response in death of dopaminergic neurons. J. Biol. Chem. 278, 19367–19377 (2003).
Tain, L. S. et al. Rapamycin activation of 4E-BP prevents parkinsonian dopaminergic neuron loss. Nat. Neurosci. 12, 1129–1135 (2009).
Bouman, L. et al. Parkin is transcriptionally regulated by ATF4: evidence for an interconnection between mitochondrial stress and ER stress. Cell Death Differ. 18, 769–782 (2011).
Colla, E. et al. Accumulation of toxic alpha-synuclein oligomer within endoplasmic reticulum occurs in alpha-synucleinopathy in vivo. J. Neurosci. 32, 3301–3305 (2012).
Coppola-Segovia, V. et al. ER stress induced by tunicamycin triggers alpha-synuclein oligomerization, dopaminergic neurons death and locomotor impairment: a new model of Parkinson’s disease. Mol. Neurobiol. 54, 5798–5806 (2017).
Cooper, A. A. et al. Alpha-synuclein blocks ER-Golgi traffic and Rab1 rescues neuron loss in Parkinson’s models. Science 313, 324–328 (2006). This paper describes various experiments, performed in yeast and supported in animal models, that point to impaired ER and Golgi trafficking as a key mediator of the toxicity of α-synuclein.
Bellucci, A. et al. Induction of the unfolded protein response by alpha-synuclein in experimental models of Parkinson’s disease. J. Neurochem. 116, 588–605 (2011).
Salganik, M. et al. The loss of glucose-regulated protein 78 (GRP78) during normal aging or from siRNA knockdown augments human alpha-synuclein (alpha-syn) toxicity to rat nigral neurons. Neurobiol. Aging 36, 2213–2223 (2015).
Gorbatyuk, M. S. et al. Glucose regulated protein 78 diminishes alpha-synuclein neurotoxicity in a rat model of Parkinson disease. Mol. Ther. 20, 1327–1337 (2012).
Nguyen, M., Wong, Y. C., Ysselstein, D., Severino, A. & Krainc, D. Synaptic, mitochondrial, and lysosomal dysfunction in Parkinson’s disease. Trends Neurosci. 42, 140–149 (2019).
Diao, J. et al. Native alpha-synuclein induces clustering of synaptic-vesicle mimics via binding to phospholipids and synaptobrevin-2/VAMP2. eLife 2, e00592 (2013).
Wang, L. et al. α-Synuclein multimers cluster synaptic vesicles and attenuate recycling. Curr. Biol. 24, 2319–2326 (2014).
Vargas, K. J. et al. Synucleins regulate the kinetics of synaptic vesicle endocytosis. J. Neurosci. 34, 9364–9376 (2014).
Matta, S. et al. LRRK2 controls an EndoA phosphorylation cycle in synaptic endocytosis. Neuron 75, 1008–1021 (2012). This paper reports a potential physiological role of LRRK2 kinase activity at the synapse, modulating the activity of endophilin-A1 to regulate the dynamic process of synaptic vesicle recycling.
Arranz, A. M. et al. LRRK2 functions in synaptic vesicle endocytosis through a kinase-dependent mechanism. J. Cell Sci. 128, 541–552 (2015).
Soukup, S. F. et al. A LRRK2-dependent EndophilinA phosphoswitch is critical for macroautophagy at presynaptic terminals. Neuron 92, 829–844 (2016).
Islam, M. S. et al. Human R1441C LRRK2 regulates the synaptic vesicle proteome and phosphoproteome in a Drosophila model of Parkinson’s disease. Hum. Mol. Genet. 25, 5365–5382 (2016).
Pathak, D. et al. The role of mitochondrially derived ATP in synaptic vesicle recycling. J. Biol. Chem. 290, 22325–22336 (2015).
Langston, J. W., Ballard, P., Tetrud, J. W. & Irwin, I. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science 219, 979–980 (1983).
Hasegawa, E., Takeshige, K., Oishi, T., Murai, Y. & Minakami, S. 1-Methyl-4-phenylpyridinium (MPP+) induces NADH-dependent superoxide formation and enhances NADH-dependent lipid peroxidation in bovine heart submitochondrial particles. Biochem. Biophys. Res. Commun. 170, 1049–1055 (1990).
Betarbet, R. et al. Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat. Neurosci. 3, 1301–1306 (2000).
Cocheme, H. M. & Murphy, M. P. Complex I is the major site of mitochondrial superoxide production by paraquat. J. Biol. Chem. 283, 1786–1798 (2008).
Schapira, A. H. et al. Mitochondrial complex I deficiency in Parkinson’s disease. J. Neurochem. 54, 823–827 (1990). This key early paper establishes that electron transport chain complex I is a potential pathological point of convergence in PD, finding that complex I activity is specifically reduced in individuals with PD, relative to control individuals.
Keeney, P. M., Xie, J., Capaldi, R. A. & Bennett, J. P. Jr. Parkinson’s disease brain mitochondrial complex I has oxidatively damaged subunits and is functionally impaired and misassembled. J. Neurosci. 26, 5256–5264 (2006).
Devi, L., Raghavendran, V., Prabhu, B. M., Avadhani, N. G. & Anandatheerthavarada, H. K. Mitochondrial import and accumulation of alpha-synuclein impair complex I in human dopaminergic neuronal cultures and Parkinson disease brain. J. Biol. Chem. 283, 9089–9100 (2008). This influential paper highlighted mitochondria as a potential site of α-synuclein pathology, with experiments finding that α-synuclein is imported into mitochondria and that a PD-associated α-synuclein mutant has more extensive import and inhibition of complex I.
Morais, V. A. et al. Parkinson’s disease mutations in PINK1 result in decreased complex I activity and deficient synaptic function. EMBO Mol. Med. 1, 99–111 (2009).
Cleeter, M. W. et al. Glucocerebrosidase inhibition causes mitochondrial dysfunction and free radical damage. Neurochem. Int. 62, 1–7 (2013).
Vilain, S. et al. The yeast complex I equivalent NADH dehydrogenase rescues pink1 mutants. PLoS Genet. 8, e1002456 (2012).
Vos, M. et al. Vitamin K2 is a mitochondrial electron carrier that rescues pink1 deficiency. Science 336, 1306–1310 (2012).
Bi, F., Li, F., Huang, C. & Zhou, H. Pathogenic mutation in VPS35 impairs its protection against MPP(+) cytotoxicity. Int. J. Biol. Sci. 9, 149–155 (2013).
Tang, F. L. et al. VPS35 deficiency or mutation causes dopaminergic neuronal loss by impairing mitochondrial fusion and function. Cell Rep. 12, 1631–1643 (2015).
Zhou, L., Wang, W., Hoppel, C., Liu, J. & Zhu, X. Parkinson’s disease-associated pathogenic VPS35 mutation causes complex I deficits. Biochim. Biophys. Acta Mol. Basis Dis. 1863, 2791–2795 (2017).
Gonzalez-Rodriguez, P. et al. Disruption of mitochondrial complex I induces progressive parkinsonism. Nature 599, 650–656 (2021). In this work, mice with dopaminergic neuron-specific knockdown of a complex I component develop l-DOPA-responsive Parkinsonian deficits in learning, behaviour and motor coordination, supporting a central role of complex I impairment in PD pathogenesis.
Dryanovski, D. I. et al. Calcium entry and alpha-synuclein inclusions elevate dendritic mitochondrial oxidant stress in dopaminergic neurons. J. Neurosci. 33, 10154–10164 (2013).
Nakamura, K. et al. Direct membrane association drives mitochondrial fission by the Parkinson disease-associated protein alpha-synuclein. J. Biol. Chem. 286, 20710–20726 (2011).
Choi, M. L. et al. Pathological structural conversion of alpha-synuclein at the mitochondria induces neuronal toxicity. Nat. Neurosci. 25, 1134–1148 (2022).
Di Maio, R. et al. alpha-Synuclein binds to TOM20 and inhibits mitochondrial protein import in Parkinson’s disease. Sci. Transl. Med. 8, 342ra378 (2016).
Wang, X. et al. LRRK2 regulates mitochondrial dynamics and function through direct interaction with DLP1. Hum. Mol. Genet. 21, 1931–1944 (2012).
Wang, W. et al. Parkinson’s disease-associated mutant VPS35 causes mitochondrial dysfunction by recycling DLP1 complexes. Nat. Med. 22, 54–63 (2016).
Papkovskaia, T. D. et al. G2019S leucine-rich repeat kinase 2 causes uncoupling protein-mediated mitochondrial depolarization. Hum. Mol. Genet. 21, 4201–4213 (2012).
Krebiehl, G. et al. Reduced basal autophagy and impaired mitochondrial dynamics due to loss of Parkinson’s disease-associated protein DJ-1. PLoS ONE 5, e9367 (2010).
Li, G. et al. PTENα regulates mitophagy and maintains mitochondrial quality control. Autophagy 14, 1742–1760 (2018).
Wang, L. et al. PTEN-L is a novel protein phosphatase for ubiquitin dephosphorylation to inhibit PINK1-parkin-mediated mitophagy. Cell Res. 28, 787–802 (2018).
Domanskyi, A. et al. Pten ablation in adult dopaminergic neurons is neuroprotective in Parkinson’s disease models. FASEB J. 25, 2898–2910 (2011).
Choi, M. S. et al. Transnitrosylation from DJ-1 to PTEN attenuates neuronal cell death in Parkinson’s disease models. J. Neurosci. 34, 15123–15131 (2014).
Sliter, D. A. et al. Parkin and PINK1 mitigate STING-induced inflammation. Nature 561, 258–262 (2018).
McWilliams, T. G. et al. Basal mitophagy occurs independently of PINK1 in mouse tissues of high metabolic demand. Cell Metab. 27, 439–449.e5 (2018).
Yamano, K. & Youle, R. J. PINK1 is degraded through the N-end rule pathway. Autophagy 9, 1758–1769 (2013).
Morais, V. A. et al. PINK1 loss-of-function mutations affect mitochondrial complex I activity via NdufA10 ubiquinone uncoupling. Science 344, 203–207 (2014).
Gitler, A. D. et al. The Parkinson’s disease protein alpha-synuclein disrupts cellular Rab homeostasis. Proc. Natl Acad. Sci. USA 105, 145–150 (2008).
Chung, C. Y. et al. Identification and rescue of alpha-synuclein toxicity in Parkinson patient-derived neurons. Science 342, 983–987 (2013).
Mazzulli, J. R., Zunke, F., Isacson, O., Studer, L. & Krainc, D. α-Synuclein-induced lysosomal dysfunction occurs through disruptions in protein trafficking in human midbrain synucleinopathy models. Proc. Natl Acad. Sci. USA 113, 1931–1936 (2016).
Goncalves, S. A. et al. shRNA-based screen identifies endocytic recycling pathway components that act as genetic modifiers of alpha-synuclein aggregation, secretion and toxicity. PLoS Genet. 12, e1005995 (2016).
Nim, S. et al. Disrupting the alpha-synuclein-ESCRT interaction with a peptide inhibitor mitigates neurodegeneration in preclinical models of Parkinson’s disease. Nat. Commun. 14, 2150 (2023).
Lindersson, E. et al. Proteasomal inhibition by alpha-synuclein filaments and oligomers. J. Biol. Chem. 279, 12924–12934 (2004).
McNaught, K. S. et al. Impairment of the ubiquitin-proteasome system causes dopaminergic cell death and inclusion body formation in ventral mesencephalic cultures. J. Neurochem. 81, 301–306 (2002).
Xilouri, M., Vogiatzi, T., Vekrellis, K., Park, D. & Stefanis, L. Abberant alpha-synuclein confers toxicity to neurons in part through inhibition of chaperone-mediated autophagy. PLoS ONE 4, e5515 (2009).
Winslow, A. R. et al. α-Synuclein impairs macroautophagy: implications for Parkinson’s disease. J. Cell Biol. 190, 1023–1037 (2010).
Tanik, S. A., Schultheiss, C. E., Volpicelli-Daley, L. A., Brunden, K. R. & Lee, V. M. Lewy body-like alpha-synuclein aggregates resist degradation and impair macroautophagy. J. Biol. Chem. 288, 15194–15210 (2013). This paper supports autophagy as an important node in the toxicity of α-synuclein, with experiments demonstrating that α-synuclein oligomers are refractory to autophagic degradation and inhibit autophagosome maturation.
Crews, L. et al. Selective molecular alterations in the autophagy pathway in patients with Lewy body disease and in models of alpha-synucleinopathy. PLoS ONE 5, e9313 (2010).
Orenstein, S. J. et al. Interplay of LRRK2 with chaperone-mediated autophagy. Nat. Neurosci. 16, 394–406 (2013).
Sardi, S. P. et al. Augmenting CNS glucocerebrosidase activity as a therapeutic strategy for parkinsonism and other Gaucher-related synucleinopathies. Proc. Natl Acad. Sci. USA 110, 3537–3542 (2013).
Sardi, S. P. et al. Glucosylceramide synthase inhibition alleviates aberrations in synucleinopathy models. Proc. Natl Acad. Sci. USA 114, 2699–2704 (2017).
Mazzulli, J. R. et al. Activation of beta-glucocerebrosidase reduces pathological alpha-synuclein and restores lysosomal function in Parkinson’s patient midbrain neurons. J. Neurosci. 36, 7693–7706 (2016).
Miura, E. et al. VPS35 dysfunction impairs lysosomal degradation of alpha-synuclein and exacerbates neurotoxicity in a Drosophila model of Parkinson’s disease. Neurobiol. Dis. 71, 1–13 (2014).
Tang, F. L. et al. VPS35 in dopamine neurons is required for endosome-to-Golgi retrieval of lamp2a, a receptor of chaperone-mediated autophagy that is critical for alpha-synuclein degradation and prevention of pathogenesis of Parkinson’s disease. J. Neurosci. 35, 10613–10628 (2015).
Chen, X. et al. Parkinson’s disease-linked D620N VPS35 knockin mice manifest tau neuropathology and dopaminergic neurodegeneration. Proc. Natl Acad. Sci. USA 116, 5765–5774 (2019).
Mir, R. et al. The Parkinson’s disease VPS35[D620N] mutation enhances LRRK2-mediated Rab protein phosphorylation in mouse and human. Biochem. J. 475, 1861–1883 (2018). The findings of this paper offer a link between VPS35 and LRRK2 in PD pathogenesis, showing that LRRK2 activity is increased in cells with the VPS35 D620N mutation in a manner that can be rescued by VPS35 suppression.
Puigserver, P. et al. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell 92, 829–839 (1998).
St-Pierre, J. et al. Suppression of reactive oxygen species and neurodegeneration by the PGC-1 transcriptional coactivators. Cell 127, 397–408 (2006).
Ciron, C. et al. PGC-1alpha activity in nigral dopamine neurons determines vulnerability to alpha-synuclein. Acta Neuropathol. Commun. 3, 16 (2015).
Yang, L. et al. Neuroprotective effects of the triterpenoid, CDDO methyl amide, a potent inducer of Nrf2-mediated transcription. PLoS ONE 4, e5757 (2009).
Zheng, B. et al. PGC-1α, a potential therapeutic target for early intervention in Parkinson’s disease. Sci. Transl. Med. 2, 52ra73 (2010).
Settembre, C. et al. TFEB links autophagy to lysosomal biogenesis. Science 332, 1429–1433 (2011).
Decressac, M. et al. TFEB-mediated autophagy rescues midbrain dopamine neurons from alpha-synuclein toxicity. Proc. Natl Acad. Sci. USA 110, E1817–E1826 (2013). This paper provides another link between α-synuclein pathology and autophagy, showing that α-synuclein toxicity is reduced by overexpression or activation of TFEB, a transcription factor that is a master regulator of lysosome biogenesis.
Settembre, C. et al. TFEB controls cellular lipid metabolism through a starvation-induced autoregulatory loop. Nat. Cell Biol. 15, 647–658 (2013).
Nezich, C. L., Wang, C., Fogel, A. I. & Youle, R. J. MiT/TFE transcription factors are activated during mitophagy downstream of parkin and Atg5. J. Cell Biol. 210, 435–450 (2015).
Bonello, F. et al. LRRK2 impairs PINK1/parkin-dependent mitophagy via its kinase activity: pathologic insights into Parkinson’s disease. Hum. Mol. Genet. 28, 1645–1660 (2019).
Cooper, O. et al. Pharmacological rescue of mitochondrial deficits in iPSC-derived neural cells from patients with familial Parkinson’s disease. Sci. Transl. Med. 4, 141ra190 (2012).
Stafa, K. et al. Functional interaction of Parkinson’s disease-associated LRRK2 with members of the dynamin GTPase superfamily. Hum. Mol. Genet. 23, 2055–2077 (2014).
Hsieh, C. H. et al. Functional impairment in Miro degradation and mitophagy is a shared feature in familial and sporadic Parkinson’s disease. Cell Stem Cell 19, 709–724 (2016).
Wauters, F. et al. LRRK2 mutations impair depolarization-induced mitophagy through inhibition of mitochondrial accumulation of RAB10. Autophagy 16, 203–222 (2020).
Ma, K. Y., Fokkens, M. R., Reggiori, F., Mari, M. & Verbeek, D. S. Parkinson’s disease-associated VPS35 mutant reduces mitochondrial membrane potential and impairs PINK1/parkin-mediated mitophagy. Transl. Neurodegener. 10, 19 (2021).
Hanss, Z. et al. Mitochondrial and clearance impairment in p.D620N VPS35 patient-derived neurons. Mov. Disord. 36, 704–715 (2021).
Gusdon, A. M., Zhu, J., Van Houten, B. & Chu, C. T. ATP13A2 regulates mitochondrial bioenergetics through macroautophagy. Neurobiol. Dis. 45, 962–972 (2012).
Osellame, L. D. et al. Mitochondria and quality control defects in a mouse model of Gaucher disease — links to Parkinson’s disease. Cell Metab. 17, 941–953 (2013).
Baden, P. et al. Glucocerebrosidase is imported into mitochondria and preserves complex I integrity and energy metabolism. Nat. Commun. 14, 1930 (2023).
Hancock-Cerutti, W. et al. ER-lysosome lipid transfer protein VPS13C/PARK23 prevents aberrant mtDNA-dependent STING signaling. J. Cell Biol. 221, e202106046 (2022).
Schröder, L. F. et al. VPS13C regulates phospho-Rab10-mediated lysosomal function in human dopaminergic neurons. J. Cell Biol. 223, e202304042 (2024).
Demers-Lamarche, J. et al. Loss of mitochondrial function impairs lysosomes. J. Biol. Chem. 291, 10263–10276 (2016).
Guerra, F. et al. Synergistic effect of mitochondrial and lysosomal dysfunction in Parkinson’s disease. Cells 8, 452 (2019).
Sugiura, A., McLelland, G. L., Fon, E. A. & McBride, H. M. A new pathway for mitochondrial quality control: mitochondrial-derived vesicles. EMBO J. 33, 2142–2156 (2014).
Konig, T. et al. MIROs and DRP1 drive mitochondrial-derived vesicle biogenesis and promote quality control. Nat. Cell Biol. 23, 1271–1286 (2021).
McLelland, G. L., Soubannier, V., Chen, C. X., McBride, H. M. & Fon, E. A. Parkin and PINK1 function in a vesicular trafficking pathway regulating mitochondrial quality control. EMBO J. 33, 282–295 (2014).
Matheoud, D. et al. Parkinson’s disease-related proteins PINK1 and parkin repress mitochondrial antigen presentation. Cell 166, 314–327 (2016).
Braschi, E. et al. Vps35 mediates vesicle transport between the mitochondria and peroxisomes. Curr. Biol. 20, 1310–1315 (2010).
Kim, S., Coukos, R., Gao, F. & Krainc, D. Dysregulation of organelle membrane contact sites in neurological diseases. Neuron 110, 2386–2408 (2022).
Wong, Y. C., Ysselstein, D. & Krainc, D. Mitochondria-lysosome contacts regulate mitochondrial fission via RAB7 GTP hydrolysis. Nature 554, 382–386 (2018). The demonstration in this paper that mitochondria and lysosomes engage in dynamic contacts that are independent of mitophagy suggests a possible functional node of convergence for pathogenic PD proteins that operate primarily at either of these organelles.
Yamano, K., Fogel, A. I., Wang, C., van der Bliek, A. M. & Youle, R. J. Mitochondrial Rab GAPs govern autophagosome biogenesis during mitophagy. eLife 3, e01612 (2014).
Heo, J. M. et al. RAB7A phosphorylation by TBK1 promotes mitophagy via the PINK-PARKIN pathway. Sci. Adv. 4, eaav0443 (2018).
Yamano, K. et al. Endosomal Rab cycles regulate parkin-mediated mitophagy. eLife 7, e31326 (2018).
Kim, S., Wong, Y. C., Gao, F. & Krainc, D. Dysregulation of mitochondria-lysosome contacts by GBA1 dysfunction in dopaminergic neuronal models of Parkinson’s disease. Nat. Commun. 12, 1807 (2021).
Song, P., Trajkovic, K., Tsunemi, T. & Krainc, D. Parkin modulates endosomal organization and function of the endo-lysosomal pathway. J. Neurosci. 36, 2425–2437 (2016).
Peng, W., Schroder, L. F., Song, P., Wong, Y. C. & Krainc, D. Parkin regulates amino acid homeostasis at mitochondria-lysosome (M/L) contact sites in Parkinson’s disease. Sci. Adv. 9, eadh3347 (2023).
Jimenez-Orgaz, A. et al. Control of RAB7 activity and localization through the retromer-TBC1D5 complex enables RAB7-dependent mitophagy. EMBO J. 37, 235–254 (2018).
Cioni, J. M. et al. Late endosomes act as mRNA translation platforms and sustain mitochondria in axons. Cell 176, 56–72.e15 (2019). This paper demonstrates that axonal interactions between late endosomes and mitochondria are found to support the local translation of mitochondrial proteins, expanding the functional role of mitochondria–lysosome contacts.
Hughes, A. L. & Gottschling, D. E. An early age increase in vacuolar pH limits mitochondrial function and lifespan in yeast. Nature 492, 261–265 (2012).
Guardia-Laguarta, C. et al. α-Synuclein is localized to mitochondria-associated ER membranes. J. Neurosci. 34, 249–259 (2014). The finding of this study that α-synuclein localizes to ER–mitochondria contacts, where it induces mitochondrial fragmentation, suggests a potential mechanistic connection between mitochondrial and ER stresses produced by pathological α-synuclein.
Celardo, I. et al. Mitofusin-mediated ER stress triggers neurodegeneration in pink1/parkin models of Parkinson’s disease. Cell Death Dis. 7, e2271 (2016).
McLelland, G. L. et al. Mfn2 ubiquitination by PINK1/parkin gates the p97-dependent release of ER from mitochondria to drive mitophagy. eLife 7, e32866 (2018).
Hamasaki, M. et al. Autophagosomes form at ER-mitochondria contact sites. Nature 495, 389–393 (2013).
Toyofuku, T., Okamoto, Y., Ishikawa, T., Sasawatari, S. & Kumanogoh, A. LRRK2 regulates endoplasmic reticulum-mitochondrial tethering through the PERK-mediated ubiquitination pathway. EMBO J. 39, e100875 (2020).
Bonet-Ponce, L. & Cookson, M. R. The endoplasmic reticulum contributes to lysosomal tubulation/sorting driven by LRRK2. Mol. Biol. Cell 33, ar124 (2022).
Liu, Y. et al. DJ-1 regulates the integrity and function of ER-mitochondria association through interaction with IP3R3-Grp75-VDAC1. Proc. Natl Acad. Sci. USA 116, 25322–25328 (2019).
Paillusson, S. et al. α-Synuclein binds to the ER-mitochondria tethering protein VAPB to disrupt Ca2+ homeostasis and mitochondrial ATP production. Acta Neuropathol. 134, 129–149 (2017).
Parrado-Fernandez, C. et al. Reduction of PINK1 or DJ-1 impair mitochondrial motility in neurites and alter ER-mitochondria contacts. J. Cell Mol. Med. 22, 5439–5449 (2018).
Williams, E. T. et al. Parkin mediates the ubiquitination of VPS35 and modulates retromer-dependent endosomal sorting. Hum. Mol. Genet. 27, 3189–3205 (2018).
Cao, M., Milosevic, I., Giovedi, S. & De Camilli, P. Upregulation of parkin in endophilin mutant mice. J. Neurosci. 34, 16544–16549 (2014).
Sanyal, A., Novis, H. S., Gasser, E., Lin, S. & LaVoie, M. J. LRRK2 kinase inhibition rescues deficits in lysosome function due to heterozygous GBA1 expression in human iPSC-derived neurons. Front. Neurosci. 14, 442 (2020).
Dagda, R. K. et al. Beyond the mitochondrion: cytosolic PINK1 remodels dendrites through protein kinase A. J. Neurochem. 128, 864–877 (2014).
Ko, H. S. et al. Phosphorylation by the c-Abl protein tyrosine kinase inhibits parkin’s ubiquitination and protective function. Proc. Natl Acad. Sci. USA 107, 16691–16696 (2010).
Shin, J. H. et al. PARIS (ZNF746) repression of PGC-1α contributes to neurodegeneration in Parkinson’s disease. Cell 144, 689–702 (2011).
Lee, Y. et al. PINK1 primes parkin-mediated ubiquitination of PARIS in dopaminergic neuronal survival. Cell Rep. 18, 918–932 (2017).
Kostic, M. et al. PKA phosphorylation of NCLX reverses mitochondrial calcium overload and depolarization, promoting survival of PINK1-deficient dopaminergic neurons. Cell Rep. 13, 376–386 (2015).
Ham, S. J. et al. PINK1 and parkin regulate IP(3)R-mediated ER calcium release. Nat. Commun. 14, 5202 (2023).
Betzer, C. et al. Alpha-synuclein aggregates activate calcium pump SERCA leading to calcium dysregulation. EMBO Rep. 19, e44617 (2018).
Schondorf, D. C. et al. iPSC-derived neurons from GBA1-associated Parkinson’s disease patients show autophagic defects and impaired calcium homeostasis. Nat. Commun. 5, 4028 (2014).
Medina, D. L. et al. Lysosomal calcium signalling regulates autophagy through calcineurin and TFEB. Nat. Cell Biol. 17, 288–299 (2015).
Zhang, X. et al. MCOLN1 is a ROS sensor in lysosomes that regulates autophagy. Nat. Commun. 7, 12109 (2016).
Pollmanns, M. R. et al. Activated endolysosomal cation channel TRPML1 facilitates maturation of alpha-synuclein-containing autophagosomes. Front. Cell Neurosci. 16, 861202 (2022).
Bademosi, A. T. et al. EndophilinA-dependent coupling between activity-induced calcium influx and synaptic autophagy is disrupted by a Parkinson-risk mutation. Neuron 111, 1402–1422.13 (2023).
Lautenschlager, J. et al. C-Terminal calcium binding of alpha-synuclein modulates synaptic vesicle interaction. Nat. Commun. 9, 712 (2018).
Acknowledgements
The authors thank fellow members of the Krainc laboratory for the discussion and feedback related to the topics covered and the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
The authors both contributed to all aspects of article preparation.
Corresponding author
Ethics declarations
Competing interests
D.K. is the Founder and Scientific Advisory Board Chair of Vanqua Bio, serves on the scientific advisory boards of The Silverstein Foundation, Intellia Therapeutics and AcureX Therapeutics, and is a Venture Partner at OrbiMed. The authors declare that they have no other competing interests.
Peer review
Peer review information
Nature Reviews Neuroscience thanks Suzanne Pfeffer; Helene Plun-Favreau, who co-reviewed with Benjamin O’Callaghan; Darren Moore; and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Chaperone-mediated autophagy
-
(CMA). A form of protein degradation in which client proteins, recognized by chaperones based on the presence of a CMA motif, are directly imported into lysosomes through the receptor LAMP2. It is possible that CMA may be highly cell type or context specific.
- Chaperones
-
Proteins that assist in the folding or unfolding of other client proteins.
- Electron transport chain
-
A series of complexes in the inner mitochondrial membrane that use the energy from redox reactions involving electron transfer to establish a proton gradient between the mitochondrial matrix and intermembrane space. ATP synthase harvests the electrochemical potential of this gradient to regenerate ATP.
- Endosomes
-
Small membranous vesicles that mediate protein and lipid trafficking, recycling and sorting between other compartments of the endomembrane system, including the plasma membrane, trans-Golgi network and lysosomes.
- Exosomes
-
One of a category of small membranous vesicles that form within multivesicular bodies and are released into the extracellular space upon fusion of the multivesicular body with the plasma membrane.
- Lewy body
-
A dense inclusion of α-synuclein fibrils, ubiquitin, trapped organelles and other cellular materials that is a pathological hallmark in dopaminergic neurons in many models and clinical presentations of Parkinson disease.
- Lysosome
-
An acidic, membrane-bound compartment of the endomembrane system that contains a suite of proteases and other degradative enzymes. Lysosomes also have nutrient-sensing and signalling functions.
- Macroautophagy
-
Also referred to simply as autophagy. A process by which bulk cytosolic content, including organelles, are enveloped within double-membraned phagophores, which mature into autophagosomes and then fuse with lysosomes to mediate the degradation of the enveloped content.
- Mitophagy
-
A type of autophagy specific to mitochondria. Mitophagy can be initiated by the kinase activity of PINK1 and the ubiquitin ligase activity of parkin in response to various forms of mitochondrial stress or damage.
- Multivesicular body
-
(MVB). A membrane-bound compartment that contains internal vesicles generated by the inward budding of small vesicles from the outer, limiting membrane into the lumen of the compartment.
- Oxidative stress
-
Cellular damage that accrues through the generation of reactive oxygen species in excess of the antioxidant capacity of a cell.
- Phagophore
-
A membranous sheet that forms during the initial stages of autophagy. The phagophore folds around and sequesters cargo targeted for degradation before enclosing to form an autophagosome.
- Proteasomes
-
Cytosolic, megadalton-scale protease complexes, generally involved in the degradation of ubiquitinated proteins.
- Retromer complex
-
A protein complex consisting of VPS35, VPS39 and either VPS26A or VPS26B, which functions in sorting and retrograde trafficking of transmembrane proteins from endosomes to the trans-Golgi network or recycling from endosomes to the plasma membrane.
- Sporadic PD
-
Cases of Parkinson disease (PD) without an attributable genetic cause. Also called idiopathic PD.
- Synaptic vesicle recycling
-
The process by which the membrane and protein components of synaptic vesicles are recovered from the plasma membrane after neurotransmitter release (via endocytosis) and used to regenerate new synaptic vesicles.
- Trans-Golgi network
-
A membrane compartment downstream of the endoplasmic reticulum in the secretory pathway, which mediates the initial processing and sorting of proteins that will be either secreted or retained within the lumen of other membrane compartments.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Coukos, R., Krainc, D. Key genes and convergent pathogenic mechanisms in Parkinson disease. Nat. Rev. Neurosci. (2024). https://doi.org/10.1038/s41583-024-00812-2
Accepted:
Published:
DOI: https://doi.org/10.1038/s41583-024-00812-2