Abstract
In order to estimate the likelihood of 1, 3, 6 and 12 month mortality in patients with hip fractures, we applied a variety of machine learning methods using readily available, preoperative data. We used prospectively collected data from a single university hospital in Copenhagen, Denmark for consecutive patients with hip fractures, aged 60 years and older, treated between September 2008 to September 2010 (n = 1186). Preoperative biochemical and anamnestic data were used as predictors and outcome was survival at 1, 3, 6 and 12 months after the fracture. After feature selection for each timepoint a stratified split was done (70/30) before training and validating Random Forest models, extreme gradient boosting (XGB) and Generalized Linear Models. We evaluated and compared each model using receiver operator characteristic (ROC), calibration slope and intercept, Spiegelhalter’s z- test and Decision Curve Analysis. Using combinations of between 10 and 13 anamnestic and biochemical parameters we were able to successfully estimate the likelihood of mortality with an area under the curve on ROC curves of 0.79, 0.80, 0.79 and 0.81 for 1, 3, 6 and 12 month, respectively. The XGB was the overall best calibrated and most promising model. The XGB model most successfully estimated the likelihood of mortality postoperatively. An easy-to-use model could be helpful in perioperative decisions concerning level of care, focused research and information to patients. External validation is necessary before widespread use and is currently underway, an online tool has been developed for educational/experimental purposes (https://hipfx.shinyapps.io/hipfx/).
Similar content being viewed by others
Introduction
Hip fractures are one of the most common orthopedic injuries that require hospitalization and has vast implications for patients and healthcare providers alike. Mortality has been shown to be 5–8-fold higher during the first three months after surgery for hip fracture [1] and incidence rates has been estimated to 2.7 million patients worldwide [2]. Costs from hip fractures in the European Union alone has been estimated to be 19,000 million € annually [3].
Estimating the likelihood of mortality after this widespread and costly injury could be useful in many settings. Perhaps most importantly as an aid when providing patients and their relatives with insight as to the severity of the injury, but also for caregivers to identify patients with a higher risk that might benefit from an elevated level of care such as more intensive monitoring, specialized orthogeriatric care or to triage patients for expedited surgery. Decisions regarding choice of implant for neck of femur fractures that take life expectancy into consideration has also been discussed to avoid overtreating very frail patients with a prosthesis and the added surgical stress and prolonged rehabilitation that comes along with this procedure compared to percutaneous screws. Furthermore, on a larger scale, research on methods to decrease postoperative mortality in this heterogenic group of patients could benefit from estimations of mortality to focus efforts where they are most needed. From a public health perspective, this type of estimations could be useful in comparisons between institutions to adjust for case-mix.
There have been several publications of systems for estimating mortality after hip fracture [4,5,6,7,8,9,10], however all the methods listed above employ traditional frequentist statistics. A wide range of studies has been published demonstrating benefits and excellent performance using machine learning techniques (ML) for prediction modeling in orthopedics and other fields of medicine [11, 12]. Some more recent studies have sought to explore prediction of mortality after hip fracture with ML and achieved good results. However, these studies either use a large number of pre- and postoperative parameters making them impractical for assessment of patients upon admission to the hospital [13, 14], are of a descriptive nature concerning development of models that are not accessible to test or validate on other populations [14,15,16] or focus on a subgroup such as neck of femur fractures, patients that are critically ill or identifying patients with very high short term mortality risk after surgery [17,18,19].
We sought to develop an accurate prediction model for mortality at 1, 3, 6 and 12 months after hip fracture with ML techniques using only parameters available at the time of admission.
Furthermore, we wanted to create a freely available online tool so that estimations could be used to aid in clinical decisions.
Methods
Source of Data
The study is based on a database from Bispebjerg University Hospital in Copenhagen, Denmark, that consists of 1601 hip fracture patients with 65 recorded variables for each patient. Blood samples were taken on admission and data were recorded by the attending physician or a study nurse for the purpose of the database. All hip fracture patients with no known malignant disease were included from September 2008 to September 2010.
Participants
The database consisted of 1465 patients over 60 years of age that had suffered a hip fracture. Patients below the age of 60 years were excluded as mortality rates in younger patients that suffer hip fractures are drastically lower and we wanted to focus on potentially frail patients with health issues related to aging [20, 21]. Patients with ASA 5 or 6 (n = 1) were excluded. All patients were treated according to local guidelines incorporating a fast track program [22]. During the study period a change was made in the perioperative care of the patients while in the hospital as a dedicated orthogeriatric ward was introduced with both geriatricians and orthopedics attending to patients [23]. This was entered into the dataset as a potential variable for survival. All data analysis was done on completely anonymized datasets.
Outcome
Follow-up data on mortality was collected from the Danish civil registration system on the 10th of October 2013, so records existed for at least 36 months of follow-up time for the patients included last. All citizens and anyone residing legally in Denmark are registered in the Danish Civil Registration System using a unique 10-digit civil registration and vital status was available for all patients in the study.
Predictors
We considered the following variables in the registry for inclusion in the models. They included: age, sex, types of medication at admission, orthogeriatrics (y/n), anesthesia type, fracture type, type of operation, type of permanent residence (own home, nursing home, homeless), where patients were admitted from (own home, assisted living, rehab, hospice, hospital, nursing home), new mobility score (NMS) [24], American Society of Anesthesiologists physical status (ASA) score, body mass index (BMI), survival (yes/no) at 1, 3, 6 and 12 months after admission, biochemistry (hemoglobin, potassium, sodium, creatinine, calcium, albumin, glucose).
Missing Data and Feature Selection
One hundred and nine patients had no registered blood samples and were excluded from further calculations. Blood samples as well as all other data concerning patients were collected and recorded prospectively for the purpose of the database at the time of admission and there was no later changes to this data except for the inclusion of vital status. At the time of calculations, the data were anonymous and there was way to retrospectively use the personal identification numbers to retrieve data from the hospital charts while respecting the boundaries of the ethical permit and patient confidentiality.
Of the 1356 patients that remained, 169 patients were missing both albumin and calcium. There was no statistical significance between mortality and the cases with completely missing blood samples or the group that was missing calcium and albumin using the chi-squared test when compared to rest of the data. As such they were assumed to be missing independently of the outcome and listwise deletion should be unbiased. This was considered a better option than imputing a relatively large proportion of data for these parameters as the decreased amount of data were considered unlikely to have a significant effect on development of prediction models. Of the 1186 patients that remained most parameters had complete data and the parameters that had missing values had less than 10% missing and this was considered an acceptable amount for imputation.
Imputation was done using a random Forest imputation algorithm for missing data [25] that has been shown to outperform several of the other commonly used methods such as KnnImpute, and multiple imputation by chained equations (MICE).
The data were split in training/test partitions with a 70/30 stratified split to ensure that similar proportions of the outcome are preserved in each set.
The Boruta algorithm [26] was used for selecting parameters of importance for the different timepoints (Table 2) on the training set. This is a feature selection algorithm that works by comparing the parameters importance in relevance to the outcome with the importance of the same values permuted at random. It returns all relevant features in relation to the outcome for building prediction models. Some feature engineering was done after noting that digoxin and vitamin K-antagonists were selected by Boruta for several timepoints. Several combinations of having cardiac medications, antihypertensive and anticoagulants in the medical history were created and evaluated for inclusion by repeating the Boruta algorithm. Having prescribed diuretics, betablockers, digoxin, vitamin k antagonists and organic nitrates alone or in combination and was used as a feature and had a higher importance in combination than as individual parameters.
Blood sample values were converted to categories of normal or low for albumin and hemoglobin, normal or high for creatinine, and finally low, normal or high for potassium and calcium. While it might be beneficial to differentiate between extreme variations of abnormal it was determined nonsensical to treat these values as continuous as there should be no difference in variations within the normal range.
Finally, the same parameters and partitions for each timepoint were used to train a random forest (RF), an extreme gradient boosting (XGB) and a genralized linear model (GLM). According to Breiman and Cutler who created the Random Forest algorithm, there is no need for a separate test set or cross-validation when developing models using this technique as the algorithm effectively performs internal leave one out cross-validation (LOOCV) during training [27]. Training was done with LOOCV on the training set for the GLM and XGBoost models to make results comparable to the RF model. Hyperparameter tuning was performed using a gridsearch and internal tenfold cross-validation on the training sets for the RF and the XGBoost models and dummy encoding of categorical variables was done for the XGBoost models.
The final models were used to make predictions on the hold out test sets, performance was assessed by the area under the curve (AUC) of receiver operating characteristics (ROC) curves. Calibration slope and intercept, Spiegelhalter’s z-test and Decision Curve analysis (DCA) were assessed for all models. R software was used for calculations [28]. The manuscript was prepared according to the TRIPOD statement [29].
Results
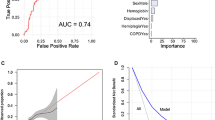
Using only parameters available at admission we were able to train ML models to estimate for 1, 3, 6 and 12 month mortality after hip fracture with good to excellent discrimination on ROC curves. The parameters chosen by the Boruta algorithm for the different timepoints where slightly different but “Permanent/ registered residence”, “Admitted from”, “New Mobility Score”, ASA, potassium, creatinine, albumin, “cardiac medications y/n” and age were relevant for all timepoints. The models performed similarly with an AUC close to 0.80 for all timepoints (Fig. 1).
The RF models had marginally better discrimination than the other models with AUC values of 0.79 (CI 0.72–0.85), 0.80 (CI 0.74–0.85), 0.79 (CI 0.74–0.84), 0.81 (CI 0.76–0.85) for 1, 3, 6 and 12 month mortality, respectively.
ROC curves and AUC values with CI for all timepoints and models are presented in Fig. 2.
While models performed in a similar manner for discrimination, there was big differences in calibration. For datasets of this size, flexible calibration plots will be unstable so mean calibration, calibration slope and intercept are reported as recommended by van Calster et al. [30].
The mean calibration is the average predicted risk compared to the overall event rate for the outcome predicted. The RF model consistently underestimated quite severely while the XGB and GLM models were well aligned with the overall event rate for all timepoints.
The calibration slope has a target value of 1 and is used to evaluate if estimations are exaggerated or too extreme (< 1) or too conservative (> 1) and has also been referred to as the “spread” of the estimates. The intercept has a target value of 0 and is a measure of over- (< 0) or under-estimation (> 0) and should be read together with the slope and indicates calibration across a range of estimations. The XGB model was fairly well calibrated for all timepoints, the GLM uncalibrated for 1 month mortality and all of the RF models were poorly calibrated.
Finally, Spiegelhalter’s z-test was also used as a measure of calibration. A set of observations and associated probabilities are used, and the null hypothesis of the statistical test is that models are well calibrated. P values that are statistically significant indicate poor calibration and the degree of miscalibration corresponds to larger absolute values of z regardless of whether values are positive or negative (Table 1).
The XGB models were the best calibrated overall, the GLM had significant P values for Spiegelhalter’s z-test for the 1- and 3 month models indicating that these were not well calibrated, and the RF was very poorly calibrated on all measurements and timepoints. P-values were significant for all RF models and the z-test had very high values in line with the mean calibration and the values of the calibration slope that also indicated poor calibration of these models.
All calibration measures are reported in Table 2.
The RF models also performed notably worse on DCA plots for all timepoints than the other models. The DCA calculates “net benefit” of using a model to choose patients for a treatment compared to treating all or none, or compared to using another model for this purpose. Considering the DCA for 3 month mortality, a “net benefit” of 0.10 at the 20% probability threshold for the outcome could be interpreted as identifying 10 true positives when using the model on a population of 100 patients.
As the models are intended to be used in a wide variety of settings, one of which is providing information to patients and their relatives, the thresholds are set so that the entire spectrum of positive values are shown. In most settings for clinical use, it is probably thresholds in the lower end that is interesting as the harm of false positives and “unnecessary treatment” is expected to be low with interventions such as increased monitoring or expedited surgery. Of course, if models are used to restrict treatment that could otherwise be beneficial this must be taken into account, however the GLM and the XGB models had a higher “net benefit” for all timepoints than the RF model, indicating that they are better suited for all clinical decisions across the range of thresholds demonstrated. The DCA curves for all models and timepoints are available in Fig. 3, for the 1 month model the DCA is truncated at the threshold of 0.5 as all models had negative values after this point.
The XGB model had the overall best performance, so using the “Shiny” software package in RStudio an interactive app was built for educational purposes to explore how the models could function in clinical practice. The “Shiny” package provides a coding language to create stand-alone web applications that can execute models developed in RStudio based on the input provided in the app. External validation of the models on other patient populations is underway and should be reviewed before putting models to widespread clinical use. The application is available online for evaluation (https://hipfx.shinyapps.io/hipfx/).
Discussion
This study demonstrated the utility of machine learning techniques in estimating the likelihood of mortality in hip fracture patients. The developed models achieved acceptable to excellent results for both GLM, XGB and Random Forest modeling determined by AUC on ROC curves but with acceptable calibration only for the XGB model. The RF models seem much less suited for clinical use as they were poorly calibrated and had less net benefit on DCA curves. The GLM and the XGB was fairly similar for 6- and 12 month mortality and had a DCA indicating that they could be useful clinically for all timepoints. Overall, the XGB model was the most promising and was well calibrated for all timepoints with non-significant values on Spiegelhalter’s z-test.
These models will need to be externally validated on a different patient material to further corroborate the results.
The Notthingham hip fracture score (NHFS) seems to be most popular of the previously published models for prediction of mortality after hip fracture. This scoring system incorporates age, sex, number of co-morbidities, mini-mental test score at admission, hemoglobin level at admission, presence of malignant disease and whether patients were living in an institution at the time of the fracture as factors. It has been externally validated several times [31,32,33,34,35], with results varying from an AUC of 0.67 in a Swedish study by Jonsson et al. to 0.83 in a smaller Greek study by Tilkeridis et al. This might reflect how different parameters have varying importance in different populations, furthermore how predicting future outcomes is not an exact science.
Several of the previous articles that utilize ML techniques to model mortality after hip fracture have used a mixture of pre- and postoperative parameters as predictors in the final models so they are not directly comparable.
A large study of 19,835 US hip fracture patients identified 47 important parameters from a database with 150 available parameters of mixed pre, intra and postoperative data and developed artificial neural network (ANN), logistic regression and naïve Bayes models with excellent results for 1 month mortality with 0.92, 0.87 and 0.83, respectively. It is unclear what the timeframe was concerning follow-up of postoperative parameters. Feature selection was done by backward variable selection and several of the parameters in our study also had importance in this study such as BMI, creatinine, hypoalbuminemia, pre-op mobility aid, age and sex [13].
Similarly, a different study from the US on 17,140 patients included length of hospital stay as a predictor as well as sociodemographic and clinical factors to predict 30 day and 1 year mortality after hip fracture using logistic regression and multilayer perceptron modeling and obtained an AUC of around 0.76 for both models and timepoints [15]. No holdout or test set was used, the performance was measured as an average of tenfold cross validation. It is not stated if any feature selection was performed or how missing data were handled. Interestingly, patients were excluded if they did not live at home, and this was one of the important features for predicting mortality in our study. It also sheds light on the impact of different organizations across countries and health care systems. In our study approximately 30% lived in a nursing home compared to approximately 5% in the US study and this is likely to cause issues concerning generalizability with models that use this type of compound parameters as it seems that different circumstances in the general health and socioeconomic status of the individual will lead to the different living arrangements across countries and regions.
Differences in methodology makes comparisons to our study difficult and the intended use of systems that include only easily available preoperative parameters and systems that include large numbers of pre- and post-operative parameters are inherently different.
One of the important parameters in our prediction models was pre-fracture residency. Several previous articles have indicated the importance of this parameter for survival in hip fracture populations. There are several possible causes for this association as it is linked to many other important parameters such as walking status, dementia and comorbidities.
An association between walking status and mortality after hip fracture has been found previously and it is also a constituent in several prediction systems in this field [8, 36, 37]. It seems likely that walking ability in hip fracture patients indicate a less frail patient and, in most cases, it is also a prerequisite for not living in a nursing home. Cognitive frailty is another constituent that could be a factor in the parameter pre-fracture residence as these patients are less likely to live independently.
In a study of 116,111 hip fracture patients in Sweden, shorter length of hospital stay was associated with a higher 30 day mortality [38]. The patients in the early discharge group were also more likely to have dementia. One possible explanation for the association between early discharge and dementia could be that these patients were residents of nursing homes and were discharged early for further care at that institution. Unfortunately, there was no data in this study regarding to what type of living situation patients were discharged.
Overall, the association between pre-fracture residence and mortality might be a representation of the general condition of frail patients and as such represent several parameters previously known to be associated with mortality such as age, mental status, comorbidity and walking status.
While the introduction of geriatric care did not end up as an important predictor in our data, several previous studies have shown that interventions such as dedicated orthogeriatric care perioperatively can decrease postoperative mortality. In a study from the Netherlands, 1-year mortality was decreased from 35 to 23% [39] and several other studies have shown similar results [23, 40]. As these measurements are done on cohorts of “hip fracture patients” as a group, the effect on the subgroup of patients at high risk is likely much higher than that reported. An accurate means of risk stratification could be used to identify which patients might benefit from more intensive monitoring and care in an effort to decrease postoperative mortality and optimize use of healthcare resources.
One of the predictors featured only for 6 and 12 month survival was BMI. Several previous studies have shown an association between low BMI, poor nutritional status and increased mortality in hip fracture patients [41,42,43]. Evaluation and correction of malnutrition within this timeframe could be interesting to evaluate further.
The presence of cardiac medications/vitamin k-antagonists in the medical history as a parameter in all the prediction models most likely reflects the increased risk of mortality induced by heart conditions as a co-morbidity rather than a risk induced from the medications in their own right. However, it could be of interest to follow patients with this type of cardiac medication and a higher risk of mortality to evaluate if their cardiac status remained unchanged or if the presence of this parameter as a predictor indicates deterioration of their preexisting cardiac morbidity after surgery and perioperative ordeals such as dehydration, decreased mobility, rehabilitation and administered opiates.
Application of machine learning techniques in the emerging age of “big data” in health care has many interesting opportunities and is being used effectively in many other fields already. Hopefully these techniques can provide medical research and clinical decision-making with many new tools. However, while similar methods might be used in areas such as personalized advertising and insurance it will be up to the medical community to ensure that prediction models created by patient data and intended for use in a medical setting is used for the patients’ best medical interest and not commercial purposes. Furthermore, ethical considerations need to be made concerning the intended use and how do distribute results at an early stage even in a medical setting. Identifying patients at risk can be used as an argument both for limiting and optimizing treatment depending on the setting, and decisions about how to handle predictions with a negative outlook and how this information is recorded and communicated during hospital stay and aftercare need to be made so that the overall treatment of patients is not affected negatively.
This study has several limitations. Estimations are based on a population from one single University Hospital in Copenhagen, Denmark, and our study population might not be comparable to other populations. Furthermore, there is always a risk of overfitting predictive models to the study population that they were trained on.
The data are about 10 years old but several large studies have shown that mortality rates after hip fracture have remained stable during the last centuries so for the purpose of creating a predictive model it was considered that this data would not be outdated [44, 45].
Some of these limitations will be investigated in future prospective studies with external validation on other populations that are currently being planned.
There is a risk that the use of pre-fracture residence might not translate well to other populations because of regional differences in health care systems so that a different set of criteria will be used to determine which patients are eligible for assisted living in a nursing home or similar institution.
In conclusion, we successfully developed models capable of estimating 1-, 3-, 6- and 12 month mortality after hip fracture surgery with good discrimination and calibration. The models are based on readily available parameters to facilitate ease of use in a clinical setting.
An online tool based on the XGB models has been developed for educational purposes and is freely available at: (https://hipfx.shinyapps.io/hipfx/).
References
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
Odén A, McCloskey EV, Johansson H, Kanis JA (2013) Assessing the impact of osteoporosis on the burden of hip fractures. Calcif Tissue Int 92:42–49
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Burgos E, Gomez-Arnau JI, Diez R, Munoz L, Fernandez-Guisasola J, Garcia del Valle S (2008) Predictive value of six risk scores for outcome after surgical repair of hip fracture in elderly patients. Acta Anaesthesiol Scand 52:125–131
Maxwell MJ, Moran CG, Moppett IK (2008) Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth 101:511–517
Ramanathan TS, Moppett IK, Wenn R, Moran CG (2005) POSSUM scoring for patients with fractured neck of femur. Br J Anaesth 94:430–433
Pugely AJ, Martin CT, Gao Y, Klocke NF, Callaghan JJ, Marsh JL (2014) A risk calculator for short-term morbidity and mortality after hip fracture surgery. J Orthop Trauma 28:63–69
Holt G, Smith R, Duncan K, Finlayson DF, Gregori A (2008) Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the scottish hip fracture audit. J Bone Joint Surg Br 90:1357–1363
Dawe EJ, Lindisfarne E, Singh T, McFadyen I, Stott P (2013) Sernbo score predicts survival after intracapsular hip fracture in the elderly. Ann R Coll Surg Engl 95:29–33
Sanz-Reig J, Salvador Marín J, Ferrández Martínez J, Orozco Beltrán D, Martínez López JF, Quesada Rico JA (2018) Prognostic factors and predictive model for in-hospital mortality following hip fractures in the elderly. Chin J Traumatol 21:163–169
Helm JM, Swiergosz AM, Haeberle HS, Karnuta JM, Schaffer JL, Krebs VE, Spitzer AI, Ramkumar PN (2020) Machine learning and artificial intelligence: definitions, applications, and future directions. Curr Rev Musculoskelet Med 13:69–76
Jayatilake S, Ganegoda GU (2021) Involvement of machine learning tools in healthcare decision making. J Healthcare Eng 2021:6679512
DeBaun MR, Chavez G, Fithian A, Oladeji K, Van Rysselberghe N, Goodnough LH, Bishop JA, Gardner MJ (2020) Artificial neural networks predict 30-day mortality after hip fracture: insights from machine learning. J Am Acad Orthop Surg 29:977
Li Y, Chen M, Lv H, Yin P, Zhang L, Tang P (2021) A novel machine-learning algorithm for predicting mortality risk after hip fracture surgery. Injury 52:1487–1493
Cary MP Jr, Zhuang F, Draelos RL, Pan W, Amarasekara S, Douthit BJ, Kang Y, Colón-Emeric CS (2021) Machine learning algorithms to predict mortality and allocate palliative care for older patients with hip fracture. J Am Med Dir Assoc 22:291–296
Forssten MP, Bass GA, Ismail AM, Mohseni S, Cao Y (2021) Predicting 1-year mortality after hip fracture surgery: an evaluation of multiple machine learning approaches. J Pers Med 11:727
Oosterhoff JHF, Savelberg A, Karhade AV, Gravesteijn BY, Doornberg JN, Schwab JH, Heng M (2022) Development and internal validation of a clinical prediction model using machine learning algorithms for 90 day and 2 year mortality in femoral neck fracture patients aged 65 years or above. Eur J Trauma Emerg Surg 48:4669–4682
Lei M, Han Z, Wang S, Han T, Fang S, Lin F, Huang T (2023) A machine learning-based prediction model for in-hospital mortality among critically ill patients with hip fracture: an internal and external validated study. Injury 54:636–644
Harris AHS, Trickey AW, Eddington HS, Seib CD, Kamal RN, Kuo AC, Ding Q, Giori NJ (2022) A tool to estimate risk of 30-day mortality and complications after hip fracture surgery: accurate enough for some but not all purposes? A study from the ACS-NSQIP database. Clin Orthop Relat Res 480:2335–2346
Ekegren CL, Edwards ER, Page R, Hau R, de Steiger R, Bucknill A, Liew S, Oppy A, Gabbe BJ (2016) Twelve-month mortality and functional outcomes in hip fracture patients under 65 years of age. Injury 47:2182–2188
Thoors O, Mellner C, Hedström M (2021) Good clinical outcome for the majority of younger patients with hip fractures: a Swedish nationwide study on 905 patients younger than 50 years of age. Acta Orthop 92:292–296
Pedersen SJ, Borgbjerg FM, Schousboe B, Pedersen BD, Jørgensen HL, Duus BR, Lauritzen JB (2008) A comprehensive hip fracture program reduces complication rates and mortality. J Am Geriatr Soc 56:1831–1838
Stenqvist C, Madsen CM, Riis T, Jørgensen HL, Duus BR, Lauritzen JB, van der Mark S (2016) Orthogeriatric service reduces mortality in patients with hip fracture. Geriatr Orthop Surg Rehabil 7:67–73
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br 75:797–798
Stekhoven DJ, Bühlmann P (2012) MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28:112–118
Kursa MB, Rudnicki WR (2010) Feature selection with the boruta package. J Stat Softw 36:1–13
Breiman L (2001) Random forests. Mach Learn 45:5–32
R Core Team (2018) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594
Van Calster B, McLernon DJ, van Smeden M, Wynants L, Steyerberg EW, Topic Group ‘Evaluating diagnostic tests and prediction models’ of the Si (2019) Calibration: the Achilles heel of predictive analytics. BMC Med 17:230
Tilkeridis K, Ververidis A, Kiziridis G, Kotzamitelos D, Galiatsatos D, Mavropoulos R, Rechova KV, Drosos G (2018) Validity of Nottingham hip fracture score in different health systems and a new modified version validated to the Greek population. Med Sci Monit 24:7665–7672
Jonsson MH, Bentzer P, Turkiewicz A, Hommel A (2018) Accuracy of the physiological and operative severity score for the enumeration of mortality and morbidity score and the Nottingham risk score in hip fracture patients in Sweden—a prospective observational study. Acta Anaesthesiol Scand 62:1057–1063
Wiles MD, Moran CG, Sahota O, Moppett IK (2011) Nottingham hip fracture score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br J Anaesth 106:501–504
Moppett IK, Parker M, Griffiths R, Bowers T, White SM, Moran CG (2012) Nottingham hip fracture score: longitudinal and multi-centre assessment. Br J Anaesth 109:546–550
Rushton PR, Reed MR, Pratt RK (2015) Independent validation of the Nottingham hip fracture score and identification of regional variation in patient risk within England. Bone Joint J 97:100–103
Nijmeijer WS, Folbert EC, Vermeer M, Slaets JP, Hegeman JH (2016) Prediction of early mortality following hip fracture surgery in frail elderly: the Almelo hip fracture score (AHFS). Injury 47:2138–2143
Iosifidis M, Iliopoulos E, Panagiotou A, Apostolidis K, Traios S, Giantsis G (2016) Walking ability before and after a hip fracture in elderly predict greater long-term survivorship. J Orthop Sci 21:48–52
Nordström P, Gustafson Y, Michaëlsson K, Nordström A (2015) Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ 350:h696
Folbert EC, Hegeman JH, Vermeer M, Regtuijt EM, van der Velde D, Ten Duis HJ, Slaets JP (2017) Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28:269–277
Middleton M, Wan B, da Assunçao R (2017) Improving hip fracture outcomes with integrated orthogeriatric care: a comparison between two accepted orthogeriatric models. Age Ageing 46:465–470
Malafarina V, Reginster JY, Cabrerizo S, Bruyère O, Kanis JA, Martinez JA, Zulet MA (2018) Nutritional status and nutritional treatment are related to outcomes and mortality in older adults with hip fracture. Nutrients 10:555
Modig K, Erdefelt A, Mellner C, Cederholm T, Talbäck M, Hedström M (2019) “Obesity paradox” holds true for patients with hip fracture: a registry-based cohort study. J Bone Joint Surg Am 101:888–895
Akinleye SD, Garofolo G, Culbertson MD, Homel P, Erez O (2018) The role of BMI in hip fracture surgery. Geriat Orthop Surg Rehabilit 9:2151458517747414
Meyer AC, Ek S, Drefahl S, Ahlbom A, Hedström M, Modig K (2021) Trends in hip fracture incidence, recurrence, and survival by education and comorbidity: a Swedish register-based study. Epidemiology 32:425–433
Gundel O, Thygesen LC, Gögenur I, Ekeloef S (2020) Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop 91:58–62
Acknowledgements
We would like to express our gratitude to Jonathan A. Forsberg for providing valuable advice, guidance, and support throughout the project.
Funding
Open access funding provided by Karolinska Institute. No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Author MM prepared the first draft of the paper and did the statistical analysis of the data. He is the guarantor. All authors were involved in the design of the study and interpretation of the results. All authors revised the paper critically for intellectual content and approved the final version. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
Corresponding author
Ethics declarations
Conflict of interest
Authors Mosfeldt, Jørgensen, Lauritzen and Jansson declare that they have no conflict of interest.
Ethical Approval
The study was approved by the local ethics committee (HB-2007-103) and by the Danish data protection agency (2012-58-0004, BHH-2014-050) and was carried out in line with the Helsinki Declaration. Data were anonymized during the course of the study.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Human and Animal Rights
No animals were used and the information about ethical approval is already in the text.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mosfeldt, M., Jørgensen, H.L., Lauritzen, J.B. et al. Development and Internal Validation of a Multivariable Prediction Model for Mortality After Hip Fracture with Machine Learning Techniques. Calcif Tissue Int (2024). https://doi.org/10.1007/s00223-024-01208-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00223-024-01208-1