Abstract
Background
Multivisceral en bloc resection with the ipsilateral kidney is commonly performed in patients with retroperitoneal liposarcoma (RLPS). We evaluated the effect of nephrectomy on short- and long-term outcomes in patients with RLPS.
Methods
Data from a prospectively maintained database of the Peking University Cancer Hospital Sarcoma Center between April 2011 and August 2022 were analyzed. We classified the RLPS patients who underwent surgery into nephrectomy group (NP) and non-nephrectomy group (non-NP). Patients were matched using a 1:1 propensity score to eliminate baseline differences between groups. Postoperative renal function outcomes, major morbidity, and mortality were analyzed to compare short-term outcomes after nephrectomy. Differences in local recurrence-free survival (LRFS) and overall survival (OS) were compared by Kaplan–Meier analysis with respect to oncological benefits.
Results
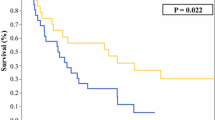
In the matched cohort, patients in the NP group had significantly higher postoperative eGFR and CKD stages, but none required dialysis. Patients between NP and non-NP had a comparable major morbidity (p = 0.820) and 60-day mortality (p = 0.475). Patients in the NP group had a higher 5‐year LRFS rates than those in the non-NP group (34.5 vs. 17.8%, p = 0.015), and similar 5‐year OS rates (52.4 vs. 47.1%, p = 0.401). Nephrectomy was an independent risk factor for LRFS, but not for major morbidity or OS.
Conclusions
RLPS resection with nephrectomy is related to a mild progression of renal impairment; however, dialysis is rare. En bloc nephrectomy for complete resection of RLPS is safe and improves local control.


Similar content being viewed by others
Data availability
All data obtained from the current study are available from the corresponding author upon reasonable request.
References
Schmitz E, Nessim C (2022) Retroperitoneal sarcoma care in 2021. Cancers (Basel) 14(5):1293.
de Bree E, Michelakis D, Heretis I et al (2023) Retroperitoneal soft tissue sarcoma: emerging therapeutic strategies. Cancers (Basel) 15(22):5469
Danieli M, Swallow CJ, Gronchi A (2023) How to treat liposarcomas located in retroperitoneum. Eur J Surg Oncol 49(6):1068–1080
Rust DJ, Kato T, Yoon SS (2022) Treatment for local control of retroperitoneal and pelvis sarcomas: a review of the literature. Surg Oncol 43:101814
Improta L, Tzanis D, Bouhadiba T et al (2020) Overview of primary adult retroperitoneal tumours. Eur J Surg Oncol 46(9):1573–1579
Bonvalot S, Roland C, Raut C et al (2023) Histology-tailored multidisciplinary management of primary retroperitoneal sarcomas. Eur J Surg Oncol 49(6):1061–1067
Improta L, Pasquali S, Iadecola S et al (2023) Organ infiltration and patient risk after multivisceral surgery for primary retroperitoneal liposarcomas. Ann Surg Oncol 30(7):4500–4510
Ruff SM, Grignol VP, Contreras CM et al (2022) Morbidity and mortality after surgery for retroperitoneal sarcoma. Curr Oncol 30(1):492–505
Tirotta F, Bacon A, Collins S et al (2023) Primary retroperitoneal sarcoma: a comparison of survival outcomes in specialist and non-specialist sarcoma centres. Eur J Cancer 188:20–28
Munoz P, Bretcha-Boix P, Artigas V et al (2022) Surgical principles of primary retroperitoneal sarcoma in the era of personalized treatment: a review of the frontline extended surgery. Cancers (Basel) 14(17):4091
Lv A, Liu D-N, Wang Z et al (2023) Short- and long-term surgical outcomes of pancreatic resection for retroperitoneal sarcoma: a long-term single-center experience of 90 cases. J Surg Oncol. 127(4):633–644
Devaud NA, Butte JM, De la Maza JC et al (2023) Complex vascular resections for retroperitoneal soft tissue sarcoma. Curr Oncol 30(3):3500–3515
Swallow CJ, Strauss DC, Bonvalot S et al (2021) Management of primary retroperitoneal sarcoma (RPS) in the adult: an updated consensus approach from the transatlantic Australasian RPS Working Group. Ann Surg Oncol. 28(12):7873–7888
Kallen ME, Hornick JL (2021) The 2020 WHO classification: what’s new in soft tissue tumor pathology? Am J Surg Pathol 45(1):e1–e23
Neuville A, Chibon F, Coindre J-M (2014) Grading of soft tissue sarcomas: from histological to molecular assessment. Pathology 46(2):113–120
Gronchi A, Miceli R, Colombo C et al (2012) Frontline extended surgery is associated with improved survival in retroperitoneal low- to intermediate-grade soft tissue sarcomas. Ann Oncol 23(4):1067–1073
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240(2):205–213
Pattaro C, Riegler P, Stifter G et al (2013) Estimating the glomerular filtration rate in the general population using different equations: effects on classification and association. Nephron Clin Pract 123(1–2):102–111
Foundation NK (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 39(2 Suppl 1):210–218
Rodrigues FB, Bruetto RG, Torres US et al (2013) Incidence and mortality of acute kidney injury after myocardial infarction: a comparison between KDIGO and RIFLE criteria. PLoS ONE 8(7):e69998
Baia M, Ford SJ, Dumitra S et al (2023) Follow-up of patients with retroperitoneal sarcoma. Eur J Surg Oncol 49(6):1125–1132
Hull MA, Niemierko A, Haynes AB et al (2015) Post-operative renal function following nephrectomy as part of en bloc resection of retroperitoneal sarcoma (RPS). J Surg Oncol. 112(1):98
Cho CW, Lee KW, Park H et al (2018) Clinical benefit and residual kidney function of en bloc nephrectomy for perirenal retroperitoneal sarcoma Asia Pac. J Clin Oncol 14(5):e465–e471
Kim DB, Gray R, Li Z et al (2018) Effect of nephrectomy for retroperitoneal sarcoma on post-operative renal function. J Surg Oncol 117(3):425–429
Stahl CC, Schwartz PB, Ethun CG et al (2021) Renal function after retroperitoneal sarcoma resection with nephrectomy: a matched analysis of the United States sarcoma collaborative database. Ann Surg Oncol 28(3):1690–1696
Fairweather M, Lyu H, Conti L et al (2022) Postnephrectomy outcomes following en bloc resection of primary retroperitoneal sarcoma: multicentre study. Br J Surg 109(2):165–168
Tseng WH, Martinez SR, Tamurian RM et al (2011) Contiguous organ resection is safe in patients with retroperitoneal sarcoma: An ACS-NSQIP analysis. J Surg Oncol 103(5):390–394
Wang Z, Wu J, Lv A et al (2018) Infiltration characteristics and influencing factors of retroperitoneal liposarcoma: novel evidence for extended surgery and a tumor grading system. Biosci Trends 12(2):185–192
Fairweather M, Wang J, Jo VY et al (2018) Surgical management of primary retroperitoneal sarcomas: rationale for selective organ resection. Ann Surg Oncol 25(1):98–106
Mussi C, Colombo P, Bertuzzi A et al (2011) Retroperitoneal sarcoma: is it time to change the surgical policy? Ann Surg Oncol 18(8):2136–2142
Anaya DA, Lahat G, Liu J et al (2009) Multifocality in retroperitoneal sarcoma: a prognostic factor critical to surgical decision-making. Ann Surg 249(1):137–142
MacNeill AJ, Gronchi A, Miceli R et al (2018) Postoperative morbidity after radical resection of primary retroperitoneal sarcoma: a report from the transatlantic RPS working group. Ann Surg 267(5):959–964
Bonvalot S, Miceli R, Berselli M et al (2010) Aggressive surgery in retroperitoneal soft tissue sarcoma carried out at high-volume centers is safe and is associated with improved local control. Ann Surg Oncol 17(6):1507–1514
Scosyrev E, Messing EM, Sylvester R et al (2014) Renal function after nephron-sparing surgery versus radical nephrectomy: results from EORTC randomized trial 30904. Eur Urol. 65(2):372–377
Acknowledgements
This study was supported by Beijing Municipal Administration of Hospital's Ascent Plan (approval No. DFL20181104), and Science Foundation of Peking University Cancer Hospital (approval No.XKFZ2421 and No.PY202308).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Xue, G., Wang, Z., Liu, B. et al. Short- and long-term post-nephrectomy outcomes for retroperitoneal liposarcoma from a high-volume sarcoma center: a propensity score matching analysis. Int J Clin Oncol (2024). https://doi.org/10.1007/s10147-024-02530-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10147-024-02530-2