Abstract
Epilepsy is one of the most common neurological disorders in the world. Common epileptic drugs generally affect ion channels or neurotransmitters and prevent the emergence of seizures. However, up to a third of the patients suffer from drug-resistant epilepsy, and there is an urgent need to develop new therapeutic strategies that go beyond acute antiepileptic (antiseizure) therapies towards therapeutics that also might have effects on chronic epilepsy comorbidities such as cognitive decline and depression. The mitochondrial calcium uniporter (MCU) mediates rapid mitochondrial Ca2+ transport through the inner mitochondrial membrane. Ca2+ influx is essential for mitochondrial functions, but longer elevations of intracellular Ca2+ levels are closely associated with seizure-induced neuronal damage, which are underlying mechanisms of cognitive decline and depression. Using neuronal-specific MCU knockout mice (MCU−/−ΔN), we demonstrate that neuronal MCU deficiency reduced hippocampal excitability in vivo. Furthermore, in vitro analyses of hippocampal glioneuronal cells reveal no change in total Ca2+ levels but differences in intracellular Ca2+ handling. MCU−/−ΔN reduces ROS production, declines metabolic fluxes, and consequently prevents glioneuronal cell death. This effect was also observed under pathological conditions, such as the low magnesium culture model of seizure-like activity or excitotoxic glutamate stimulation, whereby MCU−/−ΔN reduces ROS levels and suppresses Ca2+ overload seen in WT cells. This study highlights the importance of MCU at the interface of Ca2+ handling and metabolism as a mediator of stress-related mitochondrial dysfunction, which indicates the modulation of MCU as a potential target for future antiepileptogenic therapy.
Similar content being viewed by others
Introduction
Epilepsy is characterized by a heterogeneous spectrum of disorders that have episodic attacks of neuronal hyperexcitability in common. Currently, there are over 25 different antiepileptic drugs (AED) available, which modulate frequency and severity of seizures by affecting ion channels or neurotransmitters. However, up to a third of the patients suffer from refractory epilepsy, and the impact of epilepsy goes well beyond seizures [1].
Epileptogenesis defines a process of converting a non-epileptic brain into one capable of generating spontaneous, recurrent seizures [2]. However, over time, the epileptic neuronal network can expand, and severity of epilepsy might exacerbate. Furthermore, epilepsy is associated with severe comorbidities such as cognitive impairment and affective disorders as depression [3, 4]. Therefore, new therapeutic opportunities are needed to go beyond antiepileptic (antiseizure) therapies towards therapeutics that target the underlying processes leading to the development and progression of the disease and reduction of comorbidities.
In recent years, calcium (Ca2+) signaling has become a focus of research and seems to be a promising new target in the development of new antiepileptic drugs [5]. For instance, levetiracetam might exhibit its function at least partially via Ca2+ signaling, which leads to the hypothesis of Ca2+-mediated epileptogenesis, neuronal plasticity, and neurotoxicity [6].
Neuronal mitochondria have critical cellular functions and are involved in neuronal Ca2+ homeostasis. Mitochondrial Ca2+ overload, as seen in excitotoxic insults, can lead to the inhibition of ATP synthesis and the induction of the mitochondrial permeability transition pore (mPTP), resulting in mitochondrial dysfunction, cell damage, and neuronal death [7]. Therefore, mitochondrial Ca2+ overload could at least in part be involved in the development of acquired epilepsies, and high Ca2+ concentrations might also be initiated by seizures and, therefore, could act as an exacerbating factor in epileptogenesis [8].
In 2004, Clapham et al. discovered the existence of a Ca2+-selective mitochondrial ion channel. The analysis revealed that the current was mediated by the mitochondrial calcium uniporter (MCU), which controls the stress-dependent transport of Ca2+ through the inner mitochondrial membrane [9, 10].
Pharmacological inhibition or genetic ablation of MCU blocks the acute mitochondrial Ca2+ influx. It reduces cell death in numerous in vitro models in stress conditions, presumably due to a lower influx of Ca2+ and a decreased mPTP opening [9, 11,12,13]. Furthermore, the MCU inhibitor (Ru360) attenuates neuronal death in rat hippocampal neurons after a pilocarpine-induced status epilepticus [14], and mice with global MCU deletion showed a disturbance in the generation of gamma oscillation and sharp-wave ripples in hippocampal slice preparations, indicating a crucial role of MCU in generating fast cortical network rhythms [15]. Furthermore, in cardiomyocytes, MCU regulates mitochondrial metabolism via Ca2+ entry, leading to increased oxidative phosphorylation (OXPHOS) and enhancing the production of reducing equivalents for ATP synthesis [16].
During action potential firing, mitochondrial calcium uptake via MCU facilitated neuronal excitability, suggesting a positive feedforward mechanism of the MCU on neuronal excitability [17]. However, the role of neuronal MCU in hyperexcitability has not been characterized yet. Due to the first evidence, MCU might serve as an attractive target from an antiepileptic perspective by inhibiting acute Ca2+ overload and changes in mitochondrial function. In this situation, a selective targeting of neurons, key players in hyperexcitability, is warranted. Non-selective inhibition of all brain cells, particularly of astrocytes, is likely to lead to calcium imbalance and metabolic dysfunction since astrocytes are instrumental for neurons via metabolic support [18, 19].
In this study, we aim to characterize the effect of MCU on neuronal hyperexcitability in vivo and the glioneuronal function in vitro, focusing on calcium levels, ROS, mitochondria, and metabolic adaptations.
Materials and Methods
Mice
Animal housing and all experimental procedures were approved by local governmental authorities (Landesamt für Natur, Umwelt und Verbraucherschutz, NRW, Germany, AZ 84–02.04.2016.A307). Mice were kept under IVC (individually ventilated cages) animal housing conditions. Mice from the Neuron (NEX)-specific Cre-driver line [20] and a loxP flanking for MCU mice (Jackson Labs (line: 029817)) were intercrossed to generate neuron-specific deletion of the MCU gene (MCUfloxNEXCre, further referred as MCU−/−ΔN). All littermates were proved to have shown the deletion of MCU by genotyping (Supplement Fig. 1A). These lines were on a 100% C57BL/6 background.
In Vivo Electrophysiological Recordings
To analyze cortical network activity of mice in vivo, we recorded the spontaneous extracellular unit activity in WT and MCU−/−ΔN mice. For the procedure, mice were under deep pentobarbital anesthesia (50 mg/kg i.p.), supplemented by subcutaneous injection of carprofen (Rimadyl; 5 mg/kg). Electrodes were implanted in the left hemisphere of mice targeting the hippocampal CA1 region, following stereotaxic coordinates [21]: CA1: anteroposterior − 2.00 mm, lateral 1.5 mm from bregma, and dorsoventral 1.5 mm from the brain surface (David Kopf Instruments, USA). After 7–10 days after surgical recovery, a recording of the unit activity was performed. At the end of the experiments, animals were killed by an overdose of pentobarbital (100 mg/kg, i.p), location of the electrode sites was marked by small electrolytic lesions (2.5 mA anodal current for 2 s), and brains were rapidly removed and fixed in 4% phosphate-buffered formaldehyde, pH 7.4. After completion of all experiments, the positions of the recording electrodes were histologically verified using hematoxylin and eosin staining (Supplement Fig. 1B) [22, 23]. Neuronal activity was recorded with a Multichannel Amplifier System (Alpha Omega, Israel), and unit activities were bandpass filtered at 9 kHz at a sampling rate of 40 kHz. Spikes of individual neurons were sorted by time–amplitude window discrimination and principal component analysis (Offline Sorter, Plexon Inc., Dallas, TX, USA) and verified through quantification of cluster separation, as described before [23, 24].
Isolation of Hippocampal Glioneuronal Cultures
Neuronal cell cultures were obtained from WT and MCU−/−ΔN pups (P0-1) as described before [25, 26]. In brief, brains were dissected, and the hippocampus was preparated. After mechanical and chemical dissociation, cells were seeded at a density of 150,000 cells per Coverslip (18 mm diameter). Glioneuronal cultures were incubated at 37.0 °C and 5% CO2 and held in culture for up to 18 days before experiments. Experiments were performed in glioneuronal cultures > 12 DIV to allow for maturation of synapses.
Live Cell Imaging and Staining Procedures
Live cell images were acquired on an epifluorescence inverted microscope equipped with a 40 × oil immersion fluorite objective. Dyes were diluted in artificial cerebrospinal fluid (aCSF; 120 mM NaCl, 2.5 mM KCl, 1.25 mM NaH2PO4, 22 mM NaHCO3, 25 mM glucose, 2 mM CaCl2, 2 mM MgSO4). Live cell imaging setup provided excitation light by an LED lamp passing through a monochromator at 340, 380, or 530 nm (Carn research, Faversham, UK). Emitted fluorescence was reflected with a long-pass filter to a cooled CCD camera (Retiga; QImaging) and digitalized to 12-bit resolution.
To analyze total intracellular Ca2+ levels, a high-affinity radiometric fluorescent dye, fura-2-acetoxymethyl ester (Fura-2-AM), was used, and Ca2+ levels were detected via fluorescence microscopy [27]. Therefore, glioneuronal cultures were incubated with Fura-2-AM and 0.005% Pluronic. Cells were washed with aCSF prior to the experimental procedure. Ca2+ measurements with Fura-2-AM were performed in glioneuronal cultures using excitation light provided by an LED lamp, the beam passing through a monochromator at 340 nm and 380 nm. Emitted fluorescent light was reflected through a 515-nm-long-pass filter to a cooled CCD camera and digitized to 12-bit resolution. Traces are computed as ratios of excitation fluorescence at 340 and 380 nm, with emission at > 515 nm.
Intracellular ROS levels were measured using the cell-permeant reagent Dihydroethidium (DHE). Images were captured at an interval of 5 s while the cells were excited at 530 nm and stained with 16 µM dihydroethidium (DHE, D11347, Invitrogen). Cells were imaged instantly without preincubation to avoid an accumulation of oxidized products, and DHE was present for the entire recording period.
To analyze glutathione levels, monochlorobimane (MCB) was used, which is a non-fluorescent bimane that is spontaneously permeable across cell membrane and forms a fluorescent adduct when combined with reduced glutathione (GSH) in a reaction catalyzed by glutathione s-transferase. Glioneuronal cells were stained with 50 µM monochlorobimane (MCB, M1381MP, Invitrogen) for 40 min. Cells were excited by illumination at 380 nm, and emitted light was detected at 510/80 nm.
A cell death assay was performed to analyze neurotoxicity in glioneuronal cultures. Cells were stained with propidium iodide (PI) (10 µM), which stains only dead cells, in combination with Hoechst 33342 (4.5 µM), which stains all nuclei, and a percentage of PI-positive cells in correlation to all nuclei was calculated.
To further characterize the potential changes in mitochondrial function, we used tetramethylrhodamine (TMRM) to analyze the mitochondrial membrane potential (Δψm). Cells were stained with 30 nM TMRM (T668, Invitrogen) for 40 min. TMRM was not washed out and present during the whole imaging. Cells were imaged with excitation at 530 nm and emission at 705/72 nm [26].
All experiments were performed at room temperature, and all imaging parameters were kept constant between experiments.
Evaluation of Metabolic Function
To characterize basal metabolic changes occurring under MCU deficiency in glioneuronal cultures, the Seahorse XFe96 Analyzer (Agilent Technologies) was used. Measurements were performed according to the manufacturer’s instructions. In brief, cells were seeded at 15,000 cells per well on Seahorse XF24 tissue culture plates (Seahorse Bioscience Europe) in neurobasal media for 12 to 18 days at 37 °C and 5% CO2. Before the measurement, cells were washed, and neurobasal media was replaced with aCSF supplemented with 10 mM sodium pyruvate. At any condition, three consecutive measurements of OCR/ECAR were made. OCR/ECAR was evaluated under basal conditions and sequentially exposed to mitochondrial stressors (1 μM oligomycin, 0.5 μM FCCP, and 0.5 µM rotenone plus 0.5 μM antimycin A (all Merck)) [28]. For data analysis, Wave Software (Agilent Technologies) was used.
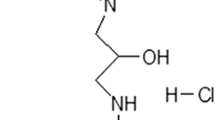
In Vitro Model to Investigate Seizure Activity and Excitotoxicity
To simulate a pathological environment, cells were challenged with a low-Mg2+ extracellular medium to induce epileptiform activity in neurons [29,30,31]. Removing magnesium from culture medium promotes NMDA receptor activation by vesicular glutamate release, resulting in seizure-like activity and Ca2+ oscillations in neurons [26, 32]. Additionally, acute glutamate (100 µM) application was tested to evaluate the effect of MCU on potential excitotoxicity-induced Ca2+ overload.
Statistical Analyses
Data represent mean ± SEM of at least three independent experiments. Prior to statistical analysis, all data were tested for normal distribution and detection of outliers. Data were statistically processed using a two-tailed Student’s t-test with two group comparisons. Comparisons between multiple groups were tested by one-way analysis of variance (ANOVA) followed by Tukey’s post hoc. P < 0.05 was considered statistically significant. Statistical analyses were performed using GraphPad Prism 6 (Version 6.01; San Diego, CA). Analysis for live cell Imaging raw data was done by Metafluor Fluorescence Ratio Imaging Software (Molecular Devices, LLC, Canada/USA), followed by plotting the data with Origin (V2019, OriginLab Corporation, Northampton, MA, USA) and ImageJ (V1.46r, Wayne Rasband, National Institute of Health, USA). Analyses were performed on single cells (Ca2+, DHE, MCB, and TMRM measurements) or regions (cell death analysis).
Results
MCU Deficiency Results in Less Excitability In Vivo
Neuronal excitation is a hallmark of neuronal network function. To examine the effects of neuronal MCU deficiency, we implanted electrodes within the CA1 region of WT and MCU−/−ΔN mice, and in vivo electrophysiological recordings and single unit analysis were performed to analyze the spontaneous excitability. In WT mice, this analysis revealed a consistent neuronal firing rate under resting conditions, which was constant during the observation timeframe, indicating a stable cortical network over time (Fig. 1A). In contrast, neuronal firing and excitation were significantly reduced in MCU−/−ΔN animals, indicating a reduction of neuronal excitation (Fig. 1A–C).
Neuronal excitability in vivo. Neuronal MCU deficiency reduces neuronal firing rate in vivo. A Histogram of the mean neuronal firing rate of WT (left) and MCU−/−∆N (right) mice over time. B Comparison of neuronal firing rate over time. Bargraphs show the mean ± SEM over the complete measurement period. C Quantitative summary of mean neuronal firing rate over time. n = 8 mice/group, ***p < 0.001
Intracellular Calcium Handling in MCU-Deficient Glioneuronal Cultures
Since MCU is responsible for intracellular Ca2+ transport through the inner mitochondrial membrane, we first examine intracellular calcium levels in our glioneuronal cultures. When comparing total Ca2+ levels under baseline condition, no difference was observed between WT and MCU−/−ΔN cells, independent of extracellular calcium concentration (Fig. 2A, B). However, since MCU is known to be active in the context of stress response [33, 34], we further challenged the calcium flux by either stimulation of Ca2+ release of the endoplasmic reticulum (ER) using thapsigargin or mitochondrial calcium release using ionomycin. Here, we observed a decrease in calcium release from the ER with a compensatory increase in calcium release from mitochondria in MCU−/−ΔN neurons compared to WT controls (Fig. 2C–E). This is rather surprising since MCU−/−ΔN cells should intuitively have reduced mitochondrial Ca2+ release capacity because of missing mitochondrial influx through MCU. These effects lead to the hypothesis that MCU−/−ΔN cells might compensate for their mitochondrial Ca2+ flux deficiency under baseline conditions by channeling Ca2+ from the ER, explaining reduced Ca2+ efflux by stimulation with thapsigargin. Whereas additional stimulation of mitochondrial Ca2+ flux is increased, potentially through augmented intramitochondrial Ca2+ levels due to missing release through MCU. This data indicates that cells compensate for the MCU deficiency by using other Ca2+ storages to balance intracellular Ca2+ homeostasis.
Calcium homeostasis in MCU−/−∆N glioneuronal cells. A, B Baseline levels (A) of intracellular calcium (fluorescence ratio of 340/380 nm of Fura 2AM) in regular (n = 160 (WT)–204 (MCU) cells) and Ca2+ free media (B) (n = 185 (WT)–118 (MCU) cells). C, D Changes of calcium release in WT and MCU neurons after the addition of thapsigargin (C) (1 µM, n = 293 (WT)–315 (MCU) cells) or ionomycin (D) (1 µM, n = 185 (WT)–118 (MCU) cells). E Representative traces show thapsigargin and ionomycin’s effect on intracellular calcium levels in WT and MCU−/−∆N neurons. All data presented as mean ± SEM, *p < 0.01, ***p < 0.001
MCU Deficiency Is Neuroprotective and Displays Reduced ROS Production
Since we could observe that MCU−/−ΔN cells seem to be less excitable and showed a shift in the intracellular calcium channeling, we aim to clarify the possible effects on cellular physiology. To evaluate the effect of MCU on cell viability, we analyzed cell death rate using propidium iodide in combination with Hoechst 33342 and observed reduced cell death in MCU−/−ΔN glioneuronal cultures (Fig. 3A). Reactive oxygen species (ROS) are known to be involved in signaling, but exacerbated ROS levels are associated with cellular dysfunction and neuronal death [35]. In line with the reduction in cellular death, MCU−/−ΔN cells also display a decrease in intracellular ROS levels (Fig. 3B), as shown before in other cell types [14, 36]. In addition, we further questioned the potential reasons for reduced ROS levels and, therefore, examined the major antioxidative system of glutathione (GSH) using MCB live cell imaging. As demonstrated before, we can observe that GSH levels in astrocytes are elevated in comparison to neuronal cells [37] in both WT and MCU−/−ΔN cultures. However, levels of intracellular GSH are unchanged between WT and MCU−/−ΔN cells (Fig. 3C), indicating other potential causes for reduced ROS levels.
MCU deficiency in cell death and ROS homeostasis. A Analysis of co-staining of glioneuronal cells with propidium iodide and Hoechst 33342 to evaluate cell death (n = 15 (WT)–19 (MCU) regions). B Intracellular ROS levels are measured using DHE (n = 99 (WT)–149 (MCU) cells). C Glutathione (GSH) was measured using the fluorescent agent monochlorobimane (MCB) and analyzed in astrocytes (n = 31 (WT)–33 (MCU) cells) and neurons (n = 68 (WT)–63 (MCU) cells). D Measurements of the membrane potential were assessed using tetramethylrhodamine-methylester (TMRM) (n = 79 (WT)–91 (MCU) cells). Data are presented as foldchange to control (WT) condition. All data presented in mean ± SEM, *p < 0.01
MCU−/−ΔN Cells Show Reduced Metabolic Fluxes
Since we observed a reduction in spontaneous excitation, we ask if MCU-deficient cells show a difference in basal mitochondrial membrane potential (MMP) since a stable MMP is needed for proper neuronal activity [38]. In line with reduced excitation in vivo, we also could observe a depolarization of MMP in MCU−/−ΔN cells in the glioneuronal cultures (Fig. 3D). A stable MMP is also needed for a proper working energy metabolism involving the respiratory chain complex. However, the respirator chain complex is also a major producer of ROS. Therefore, we ask if observed decrease in ROS levels, without alteration of the antioxidative system (GSH), might be explained by alteration of metabolic energy status of MCU−/−ΔN cells. To analyze metabolic function, we used the Seahorse flux analyzer. We observed that MCU−/−ΔN cells show a reduction in the basal oxygen consumption rate (OCR) and maximal OCR (Fig. 4A, C), indicating an overall reduction in oxidative metabolism in these cells. Furthermore, even when neurons are known to preferentially use oxidative phosphorylation (OXPHOS) for energy supply, they also can use, at least in part, glycolysis-derived pyruvate to fuel mitochondria [39, 40]. In line with the reduction of excitation in vivo, we also observed a reduction in the glycolytic flux in MCU−/−ΔN cells (Fig. 4B, D). Moreover, we used the ionophore FCCP to increase the proton leak rate to provoke a consecutive ATP demand, allowing us to determine whether the maximum glycolytic rate has been reached. However, after stimulation with FCCP, MCU−/−ΔN cells did not show differences in the maximum glycolytic capacity. Overall, we can conclude that MCU−/−ΔN cells display a decrease in metabolic fluxes, potentially leading to a reduction of ROS production through oxidative metabolism.
Metabolic adaptation MCU−/−∆N glioneuronal cells. A–D Oxygen consumption rate (OCR) as an indicator of oxidative respiration (A, C) and extracellular acidification rates (ECAR) as indicators of glycolytic activity (B, D) of WT and MCU −/−∆N glioneuronal culture measured with the Seahorse extracellular flux analyzer. Oligomycin blocks the mitochondrial ATP synthase; FCCP is a chemical uncoupler of electron transport and oxidative phosphorylation; rotenone and antimycin A are complex I and III inhibitors (n = 3). A, B Graph shows OCR/ECAR over time in glioneuronal cells. All data presented in mean ± SEM, *p < 0.01
MCU Deficiency Is Protective in Stress Response In Vitro
Since it is known that MCU activity is stress-related, we further examine if MCU−/−ΔN cells show a different response to external stressors. We, therefore, first used the glutamate excitotoxicity model, and indeed, the excessive Ca2+ influx seen in WT cells was reduced in MCU−/−ΔN cultures, indicating a potential protection for Ca2+ overload in MCU−/−ΔN cells (Fig. 5A).
Stress response in MCU−/−∆N cells. A Measurements of intercellular calcium in single cells using Fura 2AM after glutamate (100 µM) exposure in WT and MCU−/−ΔN neurons (n = 150 (WT) vs. 157(MCU) cells). B Intracellular ROS levels measured with DHE. To simulate stress conditions during hyperexcitability, the medium was changed to a low Mg2+ medium, and ROS increase was measured after 2 min and 10 min (n = 99 (WT)–149 (MCU) cells). All data presented in mean ± SEM, *p < 0.01
To further evaluate the effects of MCU−/−ΔN as a potential therapeutic target in epilepsy, we additionally used an in vitro hyperexcitability model (low Mg2+ model) to test our hypothesis of potential protective MCU deficiency due to reduced ROS levels. Indeed, as seen under baseline conditions, MCU−/−ΔN cells also show reduced ROS levels under low Mg2+ conditions, indicating MCU as potentially protective in situations of excessive ROS production (Fig. 5B).
Discussion
Since the initial discovery of the MCU channel in 2004, knowledge about its function arose quickly. MCU is involved in stress/pathological reactions in various cell types and is supposed to regulate the activation of a cell death cascade. In neurons, MCU overexpression increased mitochondrial Ca2+ levels following NMDA receptor activation, resulting in excessive Ca2+ influx, which results in MMP depolarization leading to neuronal death [9]. Therefore, manipulating MCU is an attractive target to influence intracellular Ca2+ fluxes and thereby reduce potential Ca2+ overload, as seen in seizures and hyperexcitability [26]. In line with our observation of reduced MMP and reduction in glutamate-dependent Ca2+ influx under MCU deficiency, it was shown before that pharmacological inhibition (using Ru360) of MCU can prevent the glutamate-dependent Ca2+ influx [41], a glutamate-dependent increase of MMP (depolarization) [42] and glutamate-induced mitochondrial swelling [43]. However, more interesting, we observed that MCU deficiency results in a different channeling of intracellular Ca2+ storages since stimulation with thapsigargin (stimulation of ER Ca2+ release) reduces Ca2+ fluxes. In contrast, additional stimulation of mitochondrial Ca2+ release (ionomycin) is increased in MCU-deficient cells, indicating a potential compensatory mechanism of calcium handling in MCU-deficient cells. This observation might explain, at least in part, the effects seen by others, whereas inhibition of MCU only partially inhibits Ca2+ flux in the matrix of isolated mitochondria [11, 44]. In contrast, deletion of MCU completely inhibited Ca2+ uptake in the liver, heart, and skeletal muscle mitochondria [11], indicating a cell type-dependent function of MCU.
Here, we demonstrate that neuronal MCU deficiency reduces cellular death, which might be an effect of reduced ROS production. In line with our results, it was shown before that the pharmacological inhibition of MCU leads to improved mitochondrial morphology and functional stability [45], which results in reduced cell death in the ischemia/reperfusion model [34]. In addition, pharmacological MCU inhibtion was shown to reduce, but not completely prevent, the opening of the mitochondrial permeability transition pore (PTP), which might additionally explains at least in part reduced cell death in MCU-deficient cells [11, 46]. In contrast, activation of MCU with kaempferol leads to an increase in ROS levels [33], and MCU overexpression in vivo is sufficient to trigger gliosis and neuronal loss [47], highlighting the potential of MCU inhibition from a neuroprotective perspective. Notably, all effects in our study were shown in a model of neuron-specific MCU deficiency in glioneuronal cultures. These findings indicate that the protective effect is not hampered by astrocytic MCU function. Furthermore, we deliberately chose this approach as global antagonism of MCU is likely no therapeutic strategy due to the ubiquitous expression of MCU in multiple organs.
In our study, we can demonstrate that neuronal MCU deficiency leads to reduced excitation in vivo and reduces ROS levels in a hyperexcitability model in vitro. It is known that excessive intramitochondrial Ca2+ levels can lead to depolarization of MMP [33]. Therefore, it is counterintuitive that MCU deficiency leads to a reduction of MMP. However, in a physiological setting, mitochondria increase oxidative phosphorylation during periods of stress to meet increased metabolic demand. However, under pathological condition of hyperexcitation, this stress response can be exhausted, resulting in neuronal death. In line with previous results [48], we could demonstrate that MCU-deficient cells showed a decrease in oxidative phosphorylation, which might be explained by the reduction in ROS levels and MMP. This metabolic alteration potentially prevents cells from excess stress reaction by counteracting stress response by rebalancing the ROS homeostasis through metabolic pathway modifications. Oxidative stress is known to occur in pathogenesis of acquired epilepsies [49], but is also involved in pathogenesis of psychiatric disorders, such as depression [50, 51], indicating MCU as a potential target in bidirectional therapeutic option in epilepsy and their comorbidities.
In addition, we also observed a decrease in glycolytic flux measured by the ECAR flux analyzer in neuronal MCU-deficient glioneuronal cultures. It is known that neurons mainly rely on oxidative metabolism to sustain their energy metabolism. However, the glycolytic pathway’s metabolites are needed to maintain mitochondrial function [40]. In comparison to astrocytes, glycolytic rates in neurons are relatively low. Using our neuron-specific approach, we can reveal that the glycolytic distress seen in our glioneuronal cultures under MCU deficiency affects glycolytic downstream pathways in neurons. To correctly interpret the ECAR data, it has to be taken into account that measurements of ECAR rely on consumption that the generated proton efflux (H+) is equivalent to the glycolytic flux within cells [52]. By blockade of the respiratory chain using oligomycin, we can conclude that the measured proton efflux is a result of the cellular glycolytic flux. However, it is known that neurons become energy/metabolite supplied by astrocytes via lactate [39], which might be reused for fuelling the TCA cycle via pyruvate, leading to an additional increase in proton levels [53]. Therefore, we conclude that MCU deficiency might affect neuronal glycolysis but might also influence mitochondrial function via the TCA cycle. However, the underlying mechanisms of these effects are still elusive.
It is known that MCU gets activated through larger intracellular Ca2+ levels as seen under pathological conditions [54], and increased Ca2+ levels are involved in hyperexcitation and trigger opening of the membrane permeability transition pore (PTP). Under pathological conditions such as epileptic seizures and excitotoxicity, this increased Ca2+ entry via the MCU might affect the tightly regulated mitochondrial energy metabolism. Novorolsky et al. demonstrated that acute siRNA-mediated MCU knockdown protected cortical neuron cultures from mitochondrial deficits by resembling mitochondrial respiration following oxygen and glucose deprivation [55], which might prevent cells from metabolic exhaustion in pathological conditions.
In conclusion, we could demonstrate that neuronal MCU deficiency results in a neuroprotective phenotype under stress conditions as hyperexcitation. This might be the effect of reduced oxidative stress, potentially modulated by different Ca2+ channeling and neuronal metabolic adaptations. These results indicate MCU as a potential target in future neuroprotective therapies.
Data availability
No datasets were generated or analysed during the current study.
References
Thijs RD, Surges R, O’Brien TJ, Sander JW (2019) Epilepsy in adults. The Lancet 393:689–701. https://doi.org/10.1016/S0140-6736(18)32596-0
Kobow K, Auvin S, Jensen F et al (2012) Finding a better drug for epilepsy: antiepileptogenesis targets. Epilepsia 53:1868–1876. https://doi.org/10.1111/j.1528-1167.2012.03716.x
Hermann BP, Struck AF, Busch RM et al (2021) Neurobehavioural comorbidities of epilepsy: towards a network-based precision taxonomy. Nat Rev Neurol 17:731–746. https://doi.org/10.1038/s41582-021-00555-z
Keezer MR, Sisodiya SM, Sander JW (2016) Comorbidities of epilepsy: current concepts and future perspectives. Lancet Neurol 15:106–115. https://doi.org/10.1016/S1474-4422(15)00225-2
Kovac S, Dinkova Kostova AT, Herrmann AM et al (2017) Metabolic and homeostatic changes in seizures and acquired epilepsy—mitochondria, calcium dynamics and reactive oxygen species. Int J Mol Sci 18:1935. https://doi.org/10.3390/ijms18091935
Nagarkatti N, Deshpande LS, DeLorenzo RJ (2008) Levetiracetam inhibits both ryanodine and IP3 receptor activated calcium induced calcium release in hippocampal neurons in culture. Neurosci Lett 436:289–293. https://doi.org/10.1016/j.neulet.2008.02.076
Sullivan PG, Rabchevsky AG, Waldmeier PC, Springer JE (2005) Mitochondrial permeability transition in CNS trauma: cause or effect of neuronal cell death? J Neurosci Res 79:231–239. https://doi.org/10.1002/jnr.20292
Kovács R, Kardos J, Heinemann U, Kann O (2005) Mitochondrial calcium ion and membrane potential transients follow the pattern of epileptiform discharges in hippocampal slice cultures. J Neurosci 25:4260–4269. https://doi.org/10.1523/JNEUROSCI.4000-04.2005
Qiu J, Tan Y-W, Hagenston AM et al (2013) Mitochondrial calcium uniporter Mcu controls excitotoxicity and is transcriptionally repressed by neuroprotective nuclear calcium signals. Nat Commun 4:2034. https://doi.org/10.1038/ncomms3034
Kirichok Y, Krapivinsky G, Clapham DE (2004) The mitochondrial calcium uniporter is a highly selective ion channel. Nature 427:360–364. https://doi.org/10.1038/nature02246
Hamilton J, Brustovetsky T, Rysted JE et al (2018) Deletion of mitochondrial calcium uniporter incompletely inhibits calcium uptake and induction of the permeability transition pore in brain mitochondria. J Biol Chem 293:15652–15663. https://doi.org/10.1074/jbc.RA118.002926
Nichols M, Pavlov EV, Robertson GS (2018) Tamoxifen-induced knockdown of the mitochondrial calcium uniporter in Thy1-expressing neurons protects mice from hypoxic/ischemic brain injury. Cell Death Dis 9:606. https://doi.org/10.1038/s41419-018-0607-9
Niescier RF, Hong K, Park D, Min K-T (2018) MCU Interacts with Miro1 to modulate mitochondrial functions in neurons. J Neurosci Off J Soc Neurosci 38:4666–4677. https://doi.org/10.1523/JNEUROSCI.0504-18.2018
Wang C, Xie N, Wang Y et al (2015) Role of the mitochondrial calcium uniporter in rat hippocampal neuronal death after pilocarpine-induced status epilepticus. Neurochem Res 40:1739–1746. https://doi.org/10.1007/s11064-015-1657-3
Bas-Orth C, Schneider J, Lewen A et al (2020) The mitochondrial calcium uniporter is crucial for the generation of fast cortical network rhythms. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab 40:2225–2239. https://doi.org/10.1177/0271678X19887777
Wu Y, Rasmussen TP, Koval OM et al (2015) The mitochondrial uniporter controls fight or flight heart rate increases. Nat Commun 6:6081. https://doi.org/10.1038/ncomms7081
Groten CJ, MacVicar BA (2022) Mitochondrial Ca2+ uptake by the MCU facilitates pyramidal neuron excitability and metabolism during action potential firing. Commun Biol 5:1–15. https://doi.org/10.1038/s42003-022-03848-1
Seifert G, Steinhäuser C (2013) Neuron–astrocyte signaling and epilepsy. Exp Neurol 244:4–10. https://doi.org/10.1016/j.expneurol.2011.08.024
Boison D, Steinhäuser C (2018) Epilepsy and astrocyte energy metabolism. Glia 66:1235–1243. https://doi.org/10.1002/glia.23247
Goebbels S, Bormuth I, Bode U et al (2006) Genetic targeting of principal neurons in neocortex and hippocampus of NEX-Cre mice. Genesis 44:611–621. https://doi.org/10.1002/dvg.20256
Paxinos and Franklin’s the Mouse Brain in Stereotaxic Coordinates, Compact - 5th Edition. https://www.elsevier.com/books/paxinos-and-franklins-the-mouse-brain-in-stereotaxic-coordinates-compact/franklin/978-0-12-816159-3. Accessed 20 Oct 2021
Cerina M, Narayanan V, Göbel K et al (2017) The quality of cortical network function recovery depends on localization and degree of axonal demyelination. Brain Behav Immun 59:103–117. https://doi.org/10.1016/j.bbi.2016.08.014
Narayanan V, Heiming RS, Jansen F et al (2011) Social defeat: impact on fear extinction and amygdala-prefrontal cortical theta synchrony in 5-HTT deficient mice. PLoS One 6:e22600. https://doi.org/10.1371/journal.pone.0022600
Narayanan V, Cerina M, Göbel K et al (2018) Impairment of frequency-specific responses associated with altered electrical activity patterns in auditory thalamus following focal and general demyelination. Exp Neurol 309:54–66. https://doi.org/10.1016/j.expneurol.2018.07.010
Herrmann AM, Göbel K, Simon OJ et al (2010) Glatiramer acetate attenuates pro-inflammatory t cell responses but does not directly protect neurons from inflammatory cell death. Am J Pathol 177:3051–3060. https://doi.org/10.2353/ajpath.2010.100442
Kovac S, Domijan A-M, Walker MC, Abramov AY (2012) Prolonged seizure activity impairs mitochondrial bioenergetics and induces cell death. J Cell Sci 125:1796–1806. https://doi.org/10.1242/jcs.099176
Hundehege P, Fernandez-Orth J, Römer P et al (2018) Targeting voltage-dependent calcium channels with pregabalin exerts a direct neuroprotective effect in an animal model of multiple sclerosis. Neurosignals 26:77–93. https://doi.org/10.1159/000495425
Klotz L, Eschborn M, Lindner M et al (2019) Teriflunomide treatment for multiple sclerosis modulates T cell mitochondrial respiration with affinity-dependent effects. SciTransl Med 11. https://doi.org/10.1126/scitranslmed.aao5563
Kovacs R, Schuchmann S, Gabriel S et al (2001) Ca2+ signalling and changes of mitochondrial function during low-Mg2+-induced epileptiform activity in organotypic hippocampal slice cultures. Eur J Neurosci 13:1311–1319. https://doi.org/10.1046/j.0953-816x.2001.01505.x
Mody I, Lambert JD, Heinemann U (1987) Low extracellular magnesium induces epileptiform activity and spreading depression in rat hippocampal slices. J Neurophysiol 57:869–888. https://doi.org/10.1152/jn.1987.57.3.869
Sombati S, Delorenzo RJ (1995) Recurrent spontaneous seizure activity in hippocampal neuronal networks in culture. J Neurophysiol 73:1706–1711. https://doi.org/10.1152/jn.1995.73.4.1706
Shekh-Ahmad T, Eckel R, Dayalan Naidu S et al (2018) KEAP1 inhibition is neuroprotective and suppresses the development of epilepsy. Brain J Neurol 141:1390–1403. https://doi.org/10.1093/brain/awy071
Hamilton S, Terentyeva R, Kim TY et al (2018) Pharmacological modulation of mitochondrial Ca2+ content regulates sarcoplasmic reticulum Ca2+ release via oxidation of the ryanodine receptor by mitochondria-derived reactive oxygen species. Front Physiol 9:1831. https://doi.org/10.3389/fphys.2018.01831
Yu S, Zheng S, Leng J et al (2016) Inhibition of mitochondrial calcium uniporter protects neurocytes from ischemia/reperfusion injury via the inhibition of excessive mitophagy. Neurosci Lett 628:24–29. https://doi.org/10.1016/j.neulet.2016.06.012
Di Meo S, Reed TT, Venditti P, Victor VM (2016) Role of ROS and RNS sources in physiological and pathological conditions. Oxid Med Cell Longev 2016:e1245049. https://doi.org/10.1155/2016/1245049
Li Y, Wang C, Lian Y et al (2020) Role of the mitochondrial calcium uniporter in Mg2+-free-induced epileptic hippocampal neuronal apoptosis. Int J Neurosci 130:1024–1032. https://doi.org/10.1080/00207454.2020.1715978
Gola L, Bierhansl L, Csatári J et al (2023) NOX4-derived ROS are neuroprotective by balancing intracellular calcium stores. Cell Mol Life Sci 80:127. https://doi.org/10.1007/s00018-023-04758-z
Kann O, Kovács R (2007) Mitochondria and neuronal activity. Am J Physiol-Cell Physiol 292:C641–C657. https://doi.org/10.1152/ajpcell.00222.2006
Yellen G (2018) Fueling thought: management of glycolysis and oxidative phosphorylation in neuronal metabolism. J Cell Biol 217:2235–2246. https://doi.org/10.1083/jcb.201803152
Bonvento G, Bolaños JP (2021) Astrocyte-neuron metabolic cooperation shapes brain activity. Cell Metab 33:1546–1564. https://doi.org/10.1016/j.cmet.2021.07.006
Strokin M, Reiser G (2016) Mitochondrial Ca2+ processing by a unit of mitochondrial Ca2+ uniporter and Na+/Ca2+ exchanger supports the neuronal Ca2+ influx via activated glutamate receptors. Neurochem Res 41:1250–1262. https://doi.org/10.1007/s11064-015-1819-3
Abramov AY, Duchen MR (2008) Mechanisms underlying the loss of mitochondrial membrane potential in glutamate excitotoxicity. Biochim Biophys Acta BBA - Bioenerg 1777:953–964. https://doi.org/10.1016/j.bbabio.2008.04.017
Shalbuyeva N, Brustovetsky T, Bolshakov A, Brustovetsky N (2006) Calcium-dependent spontaneously reversible remodeling of brain mitochondria. J Biol Chem 281:37547–37558. https://doi.org/10.1074/jbc.M607263200
Doczi J, Turiák L, Vajda S et al (2011) Complex contribution of cyclophilin D to Ca2+-induced permeability transition in brain mitochondria, with relation to the bioenergetic state. J Biol Chem 286:6345–6353. https://doi.org/10.1074/jbc.M110.196600
Zhao L, Li S, Wang S et al (2015) The effect of mitochondrial calcium uniporter on mitochondrial fission in hippocampus cells ischemia/reperfusion injury. Biochem Biophys Res Commun 461:537–542. https://doi.org/10.1016/j.bbrc.2015.04.066
Yu N, Wang S, Wang P, Li Y, Li S, Wang L, Chen H, Wang Y (2012) The calcium uniporter regulates the permeability transition pore in isolated cortical mitochondria. Neural Regen Res 7(2):109–113. https://doi.org/10.3969/j.issn.1673-5374.2012.02.005
Granatiero V, Pacifici M, Raffaello A et al (2019) Overexpression of mitochondrial calcium uniporter causes neuronal death. Oxid Med Cell Longev 2019:1681254. https://doi.org/10.1155/2019/1681254
Nichols M, Elustondo PA, Warford J et al (2017) Global ablation of the mitochondrial calcium uniporter increases glycolysis in cortical neurons subjected to energetic stressors. J Cereb Blood Flow Metab 37:3027–3041. https://doi.org/10.1177/0271678X16682250
Borowicz-Reutt KK, Czuczwar SJ (2020) Role of oxidative stress in epileptogenesis and potential implications for therapy. Pharmacol Rep 72:1218–1226. https://doi.org/10.1007/s43440-020-00143-w
Ravizza T, Onat FY, Brooks-Kayal AR et al (2017) WONOEP appraisal: biomarkers of epilepsy-associated comorbidities. Epilepsia 58:331–342. https://doi.org/10.1111/epi.13652
Gangar K, Bhatt LK (2020) Therapeutic targets for the treatment of comorbidities associated with epilepsy. Curr Mol Pharmacol 13:85–93. https://doi.org/10.2174/1874467212666191203101606
Plitzko B, Loesgen S (2018) Measurement of oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) in culture cells for assessment of the energy metabolism. Bio-Protoc 8:e2850. https://doi.org/10.21769/BioProtoc.2850
Schmidt CA, Fisher-Wellman KH, Neufer PD (2021) From OCR and ECAR to energy: perspectives on the design and interpretation of bioenergetics studies. J Biol Chem 297:101140. https://doi.org/10.1016/j.jbc.2021.101140
Chamberland S, Zamora Moratalla A, Topolnik L (2019) Calcium extrusion mechanisms in dendrites of mouse hippocampal CA1 inhibitory interneurons. Cell Calcium 77:49–57. https://doi.org/10.1016/j.ceca.2018.12.002
Novorolsky RJ, Nichols M, Kim JS et al (2020) The cell-permeable mitochondrial calcium uniporter inhibitor Ru265 preserves cortical neuron respiration after lethal oxygen glucose deprivation and reduces hypoxic/ischemic brain injury. J Cereb Blood Flow Metab 40:1172–1181. https://doi.org/10.1177/0271678X20908523
Acknowledgements
The authors thank I. Loesman for expert technical assistance.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
L.B. performed experiments, analyzed and interpreted the data, and was major in writing the manuscript. L.G. performed the majority of experiments, analyzed and interpreted the data, and co-wrote the manuscript. S.K. and L.B. designed the experiments and contributed to the execution. S.K., L.G., and L.B. were responsible for data interpretation and/or advice (with the input of other co-authors). V.N. performed and analyzed the in vivo experiments. A.D., S.G.M and H.W. reviewed, critically discussed, and edited the manuscript. S.K. conceptualized and directed the study. All authors discussed the results and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants performed by any of the authors. All animal studies have been approved by local authorities (Landesamt für Natur, Umwelt und Verbraucherschutz Nordrhein-Westfalen; AZ 84–02.04.2016.A307) and were conducted according to the German Animal Protection Law.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bierhansl, L., Gola, L., Narayanan, V. et al. Neuronal Mitochondrial Calcium Uniporter (MCU) Deficiency Is Neuroprotective in Hyperexcitability by Modulation of Metabolic Pathways and ROS Balance. Mol Neurobiol (2024). https://doi.org/10.1007/s12035-024-04148-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-024-04148-x